Abstract
Background
The objective of this study is to test how certain signs and symptoms related to COVID-19 in children predict the positivity or negativity of the SARS-CoV-2 nasopharyngeal swab in children.
Methods
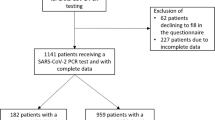
We review the data of children who were tested for SARS-CoV-2 for a suspected infection. We compared the clinical characteristics of the subjects who tested positive and negative, including the sensibility, positive and negative predictive value of different combination of signs and symptoms.
Results
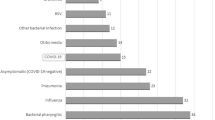
Of all the suspected infected, 2596 tested negative (96.2%) and 103 tested positive (3.8%). The median age was 7.0 and 5.3 years for the positive and negative ones, respectively. The female to male ratio was ~1:1.3. Fever and respiratory symptoms were mostly reported. Most positive children had a prior exposure to SARS-CoV-2-infected subjects (59.2%). A total of 99.3% of patients without fever nor exposure to the virus proved negative to the SARS-CoV-2 test.
Conclusions
Our study suggests that a child without fever or contact with infected subjects is SARS-CoV-2 negative. If this were to be confirmed, many resources would be spared, with improved care of both COVID-19 and not COVID-19-affected children.
Impact
-
Key message: lack of fever and exposure to SARS-CoV-2-infected people highly predicts a negative results of the SARS-CoV-2 nasopharyngeal swab in the paediatric population.
-
Added value to the current literature: this is the first article to prove this point.
-
Impact: reduction of emergency department accesses of children with suspected SARS-CoV-2 infection; increased outpatient management of children with cough or other common respiratory symptoms of infancy; sparing of many human and material health resources.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
World Health Organization. Coronavirus disease 2019 (COVID-19): situation report https://www.who.int/publications/m/item/weekly-epidemiological-update-8-december-2020 (2020).
Italian National Health Institute (Istituto Superiore di Sanità). Coronavirus epidemic: situation report https://www.epicentro.iss.it/coronavirus/, https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_2-dicembre-2020.pdf (2020).
Dong, Y. et al. Epidemiology of COVID-19 among children in China. Pediatrics 145, e20200702 (2020).
Parri, N., Lenge, M. & Buonsenso, D., Coronavirus Infection in Pediatric Emergency Departments (CONFIDENCE) Research Group. Children with COVID-19 in pediatric emergency departments in Italy. N. Engl. J. Med. 383, 187–90 (2020).
Heald-Sargent, T. et al. Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr. 174, 902–3 (2020).
Palmas, G. et al. Nasal swab as preferred clinical specimen for COVID-19 testing in children. Pediatr. Infect. Dis. J. 39, e267–e270 (2020).
Stokes, E. K. et al. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb. Mortal. Wkly Rep. 69, 759–65 (2020).
Hoang, A. et al. COVID-19 in 7780 pediatric patients: a systematic review. EClinicalMedicine 24, 100433 (2020).
Otto, W. R. et al. The epidemiology of severe acute respiratory syndrome coronavirus 2 in a pediatric healthcare network in the United States. J. Pediatr. Infect. Dis. Soc. 9, 523–9 (2020).
Zimmermann, P. & Curtis, N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr. Infect. Dis. J. 39, 355–68 (2020).
Murillo-Zamora, E., Aguilar-Sollano, F., Delgado-Enciso, I. & Hernandez-Suarez, C. M. Predictors of laboratory-positive COVID-19 in children and teenagers. Public Health 189, 153–7 (2020).
Sun, Y. et al., National Centre for Infectious Diseases COVID-19 Outbreak Research Team. Epidemiological and Clinical Predictors of COVID-19. Clin. Infect. Dis. 71, 786–92 (2020).
Thomas, J. et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 25, e204573 (2020).
Lee, B. & Raszka, W. V. Jr COVID-19 transmission and children: the child is not to blame. Pediatrics 146, e2020004879 (2020).
Villani, A. et al. School in Italy: a safe place for children and adolescents. Ital. J. Pediatr. 47, 23 (2021).
Author information
Authors and Affiliations
Contributions
Conceptualized and designed the article: M.R., U.R., G.P., and M.P. Collected data: M.R., M.A., and A.T.. Analyzed the data: M.R. Verified the underlying data and statistical analysis: M.R., U.R., and G.P. Drafted and wrote the manuscript and tables: M.R. Provided laboratory expertise, contributed to acquisition, analysis and interpretation of data: S.R., L. Colagrossi, L.P., L. Coltella, and M.A. Revised the manuscript for important intellectual content: B.S., A.R., C.F.P., P.R., and A.V. Reviewed and accepted the final manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The work was approved by our Ethics Committee. Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roversi, M., Raucci, U., Pontrelli, G. et al. Diagnosis of COVID-19 in children guided by lack of fever and exposure to SARS-CoV-2. Pediatr Res 91, 1196–1202 (2022). https://doi.org/10.1038/s41390-021-01585-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01585-5
This article is cited by
-
The impact of the pandemic on non-COVID-19 causes of death in the United States: a multiple cause of death analysis
European Journal of Epidemiology (2025)