Abstract
Background
Shiga toxin-producing Escherichia coli is responsible for post-diarrheal (D+) hemolytic uremic syndrome (HUS), which is a cause of acute renal failure in children. The glycolipid globotriaosylceramide (Gb3) is the main receptor for Shiga toxin (Stx) in kidney target cells. Eliglustat (EG) is a specific and potent inhibitor of glucosylceramide synthase, first step of glycosphingolipid biosynthesis, actually used for the treatment of Gaucher’s disease. The aim of the present work was to evaluate the efficiency of EG in preventing the damage caused by Stx2 in human renal epithelial cells.
Methods
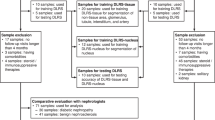
Human renal tubular epithelial cell (HRTEC) primary cultures were pre-treated with different dilutions of EG followed by co-incubation with EG and Stx2 at different times, and cell viability, proliferation, apoptosis, tubulogenesis, and Gb3 expression were assessed.
Results
In HRTEC, pre-treatments with 50 nmol/L EG for 24 h, or 500 nmol/L EG for 6 h, reduced Gb3 expression and totally prevented the effects of Stx2 on cell viability, proliferation, and apoptosis. EG treatment also allowed the development of tubulogenesis in 3D-HRTEC exposed to Stx2.
Conclusions
EG could be a potential therapeutic drug for the prevention of acute kidney injury caused by Stx2.
Impact
-
For the first time, we have demonstrated that Eliglustat prevents Shiga toxin 2 cytotoxic effects on human renal epithelia, by reducing the expression of the toxin receptor globotriaosylceramide.
-
The present work also shows that Eliglustat prevents Shiga toxin 2 effects on tubulogenesis of renal epithelial cells.
-
Eliglustat, actually used for the treatment of patients with Gaucher’s disease, could be a therapeutic strategy to prevent the renal damage caused by Shiga toxin.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Karmali, M. A. et al. The association between hemolytic uremic syndrome and infection by verotoxin-producing Escherichia coli. J. Infect. Dis. 151, 775–782 (1985).
Gianantonio, C., Vitacco, M., Mendiaharzu, F. & Rutty, A. The hemolytic-uremic syndrome. J. Pediatr. 64, 478–491 (1964).
Rivas, M., Chinen, I., Miliwebsky, E. & Masana, M. Risk factors for Shiga toxin-producing Escherichia coli-associated human diseases. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.EHEC-0002-2013 (2014).
Balestracci, A., Battaglia, L. M., Toledo, I., Martin, S. M. & Alvarado, C. Prodromal phase of hemolytic uremic syndrome related to shiga toxin-producing Escherichia coli: the wasted time. Pediatr. Emerg. Care https://doi.org/10.1097/PEC.0000000000001850 (2019).
National System of Procurement and Transplant Information of the Argentine Republic. Report of patients registered on the waiting list. http://www.sintra.incucai.gov.ar (2020).
Repetto, H. A. Epidemic hemolytic-uremic syndrome in children. Kidney Int. 52, 1708–1719 (1997).
Frank, C. H. et al. Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany. N. Engl. J. Med. 365, 1771–1780 (2011).
Cody, E. M. & Dixon, B. P. Hemolytic uremic syndrome. Pediatr. Clin. North Am. 66, 235–246 (2019).
Hussein, H. S. & Bollinger, L. M. Prevalence of Shiga toxin-producing Escherichia coli in beef cattle. J. Food Prot. 68, 2224–2241 (2005).
Meichtri, L. et al. Shiga toxin-producing Escherichia coli in healthy young beef steers from Argentina: prevalence and virulence properties. Int. J. Food Microbiol. 96, 189–198 (2004).
Ludwig, K. et al. Shiga toxin-producing Escherichia coli infection and antibodies against Stx2 and Stx1 in household contacts of children with enteropathic hemolytic-uremic syndrome. J. Clin. Microbiol. 40, 1773–1782 (2002).
Rivas, M., Miliwebsky, E., Chinen, I., Deza, N. & Leotta, G. The epidemiology of hemolytic uremic syndrome in Argentina. Diagnosis of the etiologic agent, reservoirs and routes of transmission. Medicine 66, 27–32 (2006).
Kaper, J. B., Nataro, J. P. & Mobley, H. L. Pathogenic Escherichia coli. Nat. Rev. Microbiol. 2, 123–140 (2004).
Basu, D. & Tumer, N. E. Do the A subunits contribute to the differences in the toxicity of Shiga toxin 1 and Shiga toxin 2? Toxins 7, 1467–1485 (2015).
O’Brien, A. D. & Holmes, R. K. Shiga and Shiga-like toxins. Microbiol. Rev. 51, 206–220 (1987).
Lingwood, C. A. Role of verotoxin receptors in pathogenesis. Trends Microbiol. 4, 147–153 (1996).
Sandvig, K. et al. Retrograde transport of endocytosed Shiga toxin to the endoplasmic reticulum. Nature 358, 510–512 (1992).
Johannes, L. & Römer, W. Shiga toxins – from cell biology to biomedical applications. Nat. Rev. Microbiol. 8, 105–116 (2010).
Endo, Y. et al. Site of action of a Vero toxin (VT2) from E. coli O157:H7 and of Shiga toxin on eukaryotic ribosomes. RNA N-glycosidase activity of the toxins. Eur. J. Biochem. 171, 45–50 (1988).
Tesh, V. L. Activation of cell stress response pathways by Shiga toxins. Cell. Microbiol. 14, 1–9 (2012).
Psotka, M. A. et al. Shiga toxin 2 targets the murine renal collecting duct epithelium. Infect. Immun. 77, 959–969 (2009).
Obrig, T. G. & Karpman, D. Shiga toxin pathogenesis: kidney complications and renal failure. Curr. Top. Microbiol. Immunol. 357, 105–136 (2012).
Legros, N. et al. Colocalization of receptors for Shiga toxins with lipid rafts in primary human renal glomerular endothelial cells and influence of D-PDMP on synthesis and distribution of glycosphingolipid receptors. Glycobiology 27, 947–965 (2017).
Legros, N. et al. Shiga toxin glycosphingolipid receptors and their lipid membrane ensemble in primary human blood-brain barrier endothelial cells. Glycobiology 27, 99–109 (2017).
Karpman, D. et al. Apoptosis of renal cortical cells in the hemolytic-uremic-syndrome: in vivo and in vitro studies. Infect. Immun. 66, 636–644 (1998).
Pistone Creydt, V., Silberstein, C., Zotta, E. & Ibarra, C. Cytotoxic effect of Shiga toxin-2 holotoxin and its B subunit on human renal tubular epithelial cells. Microbes Infect. 8, 410–419 (2006).
Silberstein, C., Pistone Creydt, V., Gerhardt, E., Nuñez, P. & Ibarra, C. Inhibition of water absorption in human proximal tubular epithelial cells in response to Shiga toxin-2. Pediatr. Nephrol. 23, 1981–1990 (2008).
Márquez, L. B. et al. Effects of Escherichia coli subtilase cytotoxin and shiga toxin 2 on primary cultures of human renal tubular epithelial cells. PLoS ONE 9, e87022 (2014).
Silberstein, C., Copeland, D. P., Chiang, W. L., Repetto, H. A. & Ibarra, C. A glucosylceramide synthase inhibitor prevents the cytotoxic effects of Shiga toxin-2 on human renal tubular epithelial cells. J. Epith. Biol. Pharmacol. 1, 71–75 (2008).
Amaral, M. M. et al. Action of Shiga toxin type-2 and subtilase cytotoxin on human microvascular endothelial cells. PLoS ONE 8, e70431 (2013).
Silberstein, C. et al. A glucosylceramide synthase inhibitor protects rats against the cytotoxic effects of Shiga toxin-2. Pediatr. Res. 69, 390–394 (2011).
Cox, T. M. et al. Eliglustat compared with imiglucerase in patients with Gaucher’s disease type 1 stabilised on enzyme replacement therapy: a phase 3, randomised, open-label, non-inferiority trial. Lancet 385, 2355–2362 (2015).
McEachern, K. A., Fung, J. & Komarnitsky, S. A specific and potent inhibitor of glucosylceramide synthase for substrate inhibition therapy of Gaucher disease. Mol. Genet. Metab. 91, 259–267 (2007).
Márquez, L. B., Araoz, A., Repetto, H. A., Ibarra, F. R. & Silberstein, C. Effects of Shiga toxin 2 on cellular regeneration mechanisms in primary and three-dimensional cultures of human renal tubular epithelial cells. Microb. Pathog. 99, 87–94 (2016).
Girard, M. C. et al. Prevention of renal damage caused by Shiga toxin type 2: action of Miglustat on human endothelial and epithelial cells. Toxicon 105, 27–33 (2015).
Bligh, E. G. & Dyer, W. J. A rapid method of total lipid extraction and purification. Can. J. Biochem. Physiol. 37, 911–917 (1959).
Keepers, T. R., Psotka, M. A., Gross, L. K. & Obrig, T. G. A murine model of HUS: Shiga toxin with lipopolysaccharide mimics the renal damage and physiologic response of human disease. J. Am. Soc. Nephrol. 17, 3404–3414 (2006).
Clayton, F. et al. Lipopolysaccharide upregulates renal Shiga toxin receptors in a primate model of hemolytic uremic syndrome. Am. J. Nephrol. 25, 536–540 (2005).
Lee, L., Abe, A. & Shayman, J. A. Improved inhibitors of glucosylceramide synthase. J. Biol. Chem. 274, 14662–14669 (1999).
Kolter, T., Proia, R. L. & Sandhoff, K. Combinatorial ganglioside biosynthesis. J. Biol. Chem. 277, 25859–25862 (2002).
Shayman, J. A. & Larsen, S. D. The development and use of small molecule inhibitors of glycosphingolipid metabolism for lysosomal storage diseases. J. Lipid Res. 55, 1215–1225 (2014).
Abe, A. et al. Reduction of globotriaosylceramide in Fabry disease mice by substrate deprivation. J. Clin. Invest. 105, 1563–1571 (2000).
Yew, N. S. et al. Increased hepatic insulin action in diet-induced obese mice following inhibition of glucosylceramide synthase. PLoS ONE 5, e11239 (2010).
Trachtman, H. et al. Effect of an oral Shiga toxin-binding agent on diarrhea-associated hemolytic uremic syndrome in children: a randomized controlled trial. JAMA 290, 1337–1344 (2003).
Okuda, T. et al. Targeted disruption of Gb3/CD77 synthase gene resulted in the complete deletion of globo-series glycosphingolipids and loss of sensitivity to verotoxins. J. Biol. Chem. 281, 10230–10235 (2006).
Hanashima, T. et al. Effect of Gb3 in lipid rafts in resistance to Shiga-like toxin of mutant Vero cells. Microb. Pathog. 45, 124–133 (2008).
Rogers, T. J. & Paton, J. C. Therapeutic strategies for Shiga toxin-producing Escherichia coli infections. Expert Rev. Anti Infect. Ther. 7, 683–686 (2009).
Russo, L. M., Melton-Celsa, A. R., Smith, M. A., Smith, M. J. & O’Brien, A. D. Oral intoxication of mice with Shiga toxin type 2a (Stx2a) and protection by anti-Stx2a monoclonal antibody 11E10. Infect. Immun. 82, 1213–1221 (2014).
Torres, A. G. et al. Recent advances in Shiga toxin-producing Escherichia coli research in Latin America. Microorganisms 6, 100 (2018).
Acknowledgements
We are grateful to the Pediatric Surgery team at the “Sección de Cirugía Pediátrica, Hospital General de Pediatría Pedro de Elizalde”, Buenos Aires, Argentina for providing kidney samples. We thank Natalia Beltramone, Flavia Sacerdoti, and Juan José Casal (IFIBIO-Houssay) for the technical assistance. This work was supported by grants to C.S. from the University of Buenos Aires (UBACYT20020160100078BA) and to C.I., M.M.A., and C.S. from the National Scientific and Technical Research Council (CONICET: PUE 0041).
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. D.S.S., L.K.F.S., and C.S.: substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; A.B., C.I., M.M.A., and C.S.: drafting the article or revising it critically for important intellectual content; all authors approved the final manuscript version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Written informed consent from the next of kin or guardians on behalf of the children was obtained for use of kidney samples for research. The Ethics Committee of the Hospital General de Niños Pedro de Elizalde approved the use of human renal tissues for the development of primary cell cultures for research purposes.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sánchez, D.S., Fischer Sigel, L.K., Balestracci, A. et al. Eliglustat prevents Shiga toxin 2 cytotoxic effects in human renal tubular epithelial cells. Pediatr Res 91, 1121–1129 (2022). https://doi.org/10.1038/s41390-021-01622-3
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01622-3
This article is cited by
-
Monocytes serve as Shiga toxin carriers during the development of hemolytic uremic syndrome
Cellular & Molecular Biology Letters (2025)
-
Model-informed repurposing of eliglustat for treatment and prophylaxis of Shiga toxin-producing Escherichia coli hemolytic-uremic syndrome (STEC-HUS) in children
Pediatric Nephrology (2025)