Abstract
Background
The population-level landscape of co-occurring birth defects among infants without a syndromic diagnosis is not well understood.
Methods
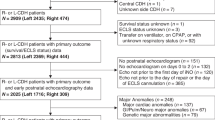
We analyzed data from 40,771 infants with two or more major birth defects in the Texas Birth Defects Registry (TBDR; 1999–2014). We calculated adjusted observed-to-expected (O/E) ratios for all two, three, four, and five-way combinations of 138 major defects.
Results
Among 530 patterns with the highest adjusted O/E ratios (top 5% of 10,595 patterns), 66% included only defects co-occurring within one organ system and 28% were suggestive of known patterns (e.g., midline developmental defects). Of the remaining patterns, the combination of defects with the highest O/E ratio (193.8) encompassed the diaphragm, spine, spleen, and heart defects. Fourteen patterns involved heart and spine defects with or without rib defects. Ten additional patterns primarily involved two hallmark components of VACTERL association (specifically, vertebral defects, anal atresia, cardiac defects, renal, or limb defects, but not tracheoesophageal fistula).
Conclusions
Our analyses provide a description of the birth defect co-occurrence patterns in a multi-ethnic, population-based sample, and revealed several patterns of interest. This work complements prior work that has suggested etiologic connections between select defects (e.g., diaphragmatic hernia and heart and spleen anomalies; heart and spine defects).
Impact
-
In this large-scale, population-based study of birth defect co-occurrence patterns, we found several birth defect combinations of potential interest that warrant further investigation: congenital diaphragmatic hernia, heart, spine, and spleen defects and scimitar syndrome with vertebral defects.
-
The majority of patterns of co-occurring defects observed more frequently than expected involved multiple defects within the same system and combinations suggestive of known associations.
-
Nearly all of the top patterns (beyond the same system and those suggestive of known associations) involved organ systems that are components of the VACTERL association, with heart, spine, and rib defect patterns being the most common.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Baird, P. A., Anderson, T. W., Newcombe, H. B. & Lowry, R. B. Genetic disorders in children and young adults: a population study. Am. J. Hum. Genet. 42, 677–693 (1988).
Kallen, B. Epidemiology of Human Reproduction (CRC Press, 1988).
Garne, E. et al. Paper 5: Surveillance of multiple congenital anomalies: implementation of a computer algorithm in European registers for classification of cases. Birth Defects Res. A Clin. Mol. Teratol. 91, S44–S50 (2011).
Calzolari, E. et al. Epidemiology of multiple congenital anomalies in Europe: a EUROCAT population-based registry study. Birth Defects Res. A Clin. Mol. Teratol. 100, 270–276 (2014).
Moorthie, S. et al. Estimating the birth prevalence and pregnancy outcomes of congenital malformations worldwide. J. Community Genet. 9, 387–396 (2018).
Shashi, V. et al. The utility of the traditional medical genetics diagnostic evaluation in the context of next-generation sequencing for undiagnosed genetic disorders. Genet. Med. 16, 176–182 (2014).
Evans, J. A. Multiple congenital anomalies: issues for birth defects surveillance. J. Registry Manag. 41, 7–12 (2014).
Agopian, A. J., Evans, J. A. & Lupo, P. J. Analytic methods for evaluating patterns of multiple congenital anomalies in birth defect registries. Birth Defects Res. 110, 5–11 (2018).
Benjamin, R. H. et al. Co-occurring defect analysis: a platform for analyzing birth defect co-occurrence in registries. Birth Defects Res. 111, 1356–1364 (2019).
Miller, E. Evaluation of the Texas Birth Defects Registry: an active surveillance system. Birth Defects Res. A Clin. Mol. Teratol. 76, 787–792 (2006).
National Center on Birth Defects and Developmental Disabilities, C. D. C. Appendix a: ICD-9 and CDC/BPA codes. Teratology 66, S218–S219 (2002).
Rasmussen, S. A. & Moore, C. A. Effective coding in birth defects surveillance. Teratology 64, S3–S7 (2001).
Rasmussen, S. A. et al. Guidelines for case classification for the National Birth Defects Prevention Study. Birth Defects Res. A Clin. Mol. Teratol. 67, 193–201 (2003).
Khoury, M. J., James, L. M. & Erickson, J. D. On the measurement and interpretation of birth defect associations in epidemiologic studies. Am. J. Med. Genet. 37, 229–236 (1990).
Jacobs, J. P. et al. The nomenclature, definition and classification of cardiac structures in the setting of heterotaxy. Cardiol. Young 17, 1–28 (2007).
Lopez, K. N., Marengo, L. K., Canfield, M. A., Belmont, J. W. & Dickerson, H. A. Racial disparities in heterotaxy syndrome. Birth Defects Res. A Clin. Mol. Teratol. 103, 941–950 (2015).
Scott, D. A. Genetics of congenital diaphragmatic hernia. Semin. Pediatr. Surg. 16, 88–93 (2007).
Stoll, C., Alembik, Y., Dott, B. & Roth, M. P. Associated malformations in cases with congenital diaphragmatic hernia. Genet. Couns. 19, 331–339 (2008).
Wynn, J., Yu, L. & Chung, W. K. Genetic causes of congenital diaphragmatic hernia. Semin. Fetal Neonatal Med. 19, 324–330 (2014).
Wat, M. J. et al. Genomic alterations that contribute to the development of isolated and non-isolated congenital diaphragmatic hernia. J. Med. Genet. 48, 299–307 (2011).
Qi, H. et al. De novo variants in congenital diaphragmatic hernia identify MYRF as a new syndrome and reveal genetic overlaps with other developmental disorders. PLoS Genet. 14, e1007822 (2018).
Rossetti, L. Z. et al. Review of the phenotypic spectrum associated with haploinsufficiency of MYRF. Am. J. Med. Genet. A 179, 1376–1382 (2019).
Farrell, S. A. et al. HLX is a candidate gene for a pattern of anomalies associated with congenital diaphragmatic hernia, short bowel, and asplenia. Am. J. Med. Genet. A 173, 3070–3074 (2017).
Gudjonsson, U. & Brown, J. W. Scimitar syndrome. Semin. Thorac. Cardiovasc. Surg. Pediatr. Card. Surg. Annu. 9, 56–62 (2006).
Masrani, A., McWilliams, S., Bhalla, S. & Woodard, P. K. Anatomical associations and radiological characteristics of scimitar syndrome on CT and MR. J. Cardiovasc. Comput. Tomogr. 12, 286–289 (2018).
Pierpont, M. E. et al. Genetic basis for congenital heart disease: revisited: a scientific statement from the American Heart Association. Circulation 138, e653–e711 (2018).
Basude, S. et al. Fetal hemivertebra: associations and perinatal outcome. Ultrasound Obstet. Gynecol. 45, 434–438 (2015).
Passias, P. G. et al. Incidence of congenital spinal abnormalities among pediatric patients and their association with scoliosis and systemic anomalies. J. Pediatr. Orthop. 39, e608–e613 (2019).
Lemire, G. T. et al. Retrospective analysis of fetal vertebral defects: associated anomalies, etiologies, and outcome. Am. J. Med. Genet. A 182, 664–672 (2020).
Wattanasirichaigoon, D., Prasad, C., Schneider, G., Evans, J. A. & Korf, B. R. Rib defects in patterns of multiple malformations: a retrospective review and phenotypic analysis of 47 cases. Am. J. Med. Genet. A 122A, 63–69 (2003).
Johal, J. et al. Hemivertebrae: a comprehensive review of embryology, imaging, classification, and management. Childs Nerv. Syst. 32, 2105–2109 (2016).
Chaturvedi, A., Klionsky, N. B., Nadarajah, U. & Meyers, S. P. Malformed vertebrae: a clinical and imaging review. Insights Imag. 9, 343–355 (2018).
Martínez-Frías, M. L. Segmentation anomalies of the vertebras and ribs: one expression of the primary developmental field. Am. J. Med. Genet. A 128A, 127–131 (2004).
Martínez-Frías, M. L. & Urioste, M. Segmentation anomalies of the vertebras and ribs: a developmental field defect: epidemiologic evidence. Am. J. Med. Genet. 49, 36–44 (1994).
Passias, P. G. et al. Cluster analysis describes constellations of cardiac anomalies presenting in spinal anomaly patients. Acta Neurochir. 160, 1613–1619 (2018).
Solomon, B. D. The etiology of VACTERL association: current knowledge and hypotheses. Am. J. Med. Genet. C Semin. Med. Genet. 178, 440–446 (2018).
Solomon, B. D. VACTERL/VATER association. Orphanet. J. Rare Dis. 6, 56 (2011).
Botto, L. D. et al. The spectrum of congenital anomalies of the VATER association: an international study. Am. J. Med. Genet. 71, 8–15 (1997).
Husain, M. et al. Phenotypic diversity of patients diagnosed with VACTERL association. Am. J. Med. Genet. A 176, 1830–1837 (2018).
van de Putte, R. et al. Spectrum of congenital anomalies among VACTERL cases: a EUROCAT population-based study. Pediatr. Res. 87, 541–549 (2020).
Boer, L. L., Morava, E., Klein, W. M., Schepens-Franke, A. N. & Oostra, R. J. Sirenomelia: a multi-systemic polytopic field defect with ongoing controversies. Birth Defects Res. 109, 791–804 (2017).
Reller, M. D., Strickland, M. J., Riehle-Colarusso, T., Mahle, W. T. & Correa, A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J. Pediatr. 153, 807–813 (2008).
Sanchez, M. L. N. et al. Birth defect co-occurrence patterns among infants with cleft lip and/or palate. Cleft Palate Craniofac. J. https://doi.org/10.1177/10556656211010060 (2021).
Tinker, S. C. et al. Challenges in studying modifiable risk factors for birth defects. Curr. Epidemiol. Rep. 2, 23–30 (2015).
Acknowledgements
This project was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R01 HD093660). Support for data collection was provided in part by the Maternal and Child Health Section, Texas Department of State Health Services, using Title V Maternal and Child Health Block Grant funds.
Author information
Authors and Affiliations
Contributions
R.H.B. contributed to study conception and design, data analysis and interpretation, drafted the article, and approved the final version; A.E.S. and D.A.S. contributed to study conception and design, data analysis and interpretation, article revisions, and approved the final version; M.L.N.S. and H.C. contributed to data analysis and interpretation, article revisions, and approved the final version; P.H.L. and M.A.C. contributed to study data acquisition, article revisions, and approved the final version; H.N., C.P.S., J.W.R., S.D.M., and M.D.S. contributed to study conception and design, article revisions, and approved the final version; P.J.L. and A.J.A. contributed to study conception and design, acquisition of data, analysis and interpretation, article revisions, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The Texas Birth Defects Registry has legislative authority to collect data without informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Benjamin, R.H., Scheuerle, A.E., Scott, D.A. et al. Birth defect co-occurrence patterns in the Texas Birth Defects Registry. Pediatr Res 91, 1278–1285 (2022). https://doi.org/10.1038/s41390-021-01629-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01629-w