Abstract
Background
Preterm infants are commonly supported with 4–8 cm H2O continuous positive airway pressures (CPAP), although higher CPAP levels may improve functional residual capacity (FRC).
Methods
Preterm rabbits delivered at 29/32 days (~26–28 weeks human) gestation received 0, 5, 8, 12, 15 cm H2O of CPAP or variable CPAP of 15 to 5 or 15 to 8 cm H2O (decreasing ~2 cm H2O/min) for up to 10 min after birth.
Results
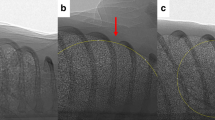
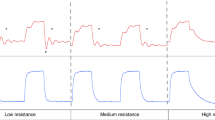
FRC was lower in the 0 (6.8 (1.0–11.2) mL/kg) and 5 (10.1 (1.1–16.8) mL/kg) compared to the 15 (18.8 (10.9–22.4) mL/kg) cm H2O groups (p = 0.003). Fewer kittens achieved FRC > 15 mL/kg in the 0 (20%), compared to 8 (36%), 12 (60%) and 15 (73%) cm H2O groups (p = 0.008). While breathing rates were not different (p = 0.096), apnoea tended to occur more often with CPAP < 8 cm H2O (p = 0.185). CPAP belly and lung bulging rates were similar whereas pneumothoraces were rare. Lowering CPAP from 15 to 5, but not 15 to 8 cm H2O, decreased FRC and breathing rates.
Conclusion
In all, 15 cm H2O of CPAP improved lung aeration and reduced apnoea, but did not increase the risk of lung over-expansion, pneumothorax or CPAP belly immediately after birth. FRC and breathing rates were maintained when CPAP was decreased to 8 cm H2O.
Impact
-
Although preterm infants are commonly supported with 4–8 cm H2O CPAP at birth, preclinical studies have shown that higher PEEP levels improve lung aeration.
-
In this study, CPAP levels of 15 cm H2O improved lung aeration and reduced apnoea in preterm rabbit kittens immediately after birth. In all, 15 cm H2O CPAP did not increase the risk of lung over-expansion (indicated by bulging between the ribs), pneumothorax, or CPAP belly.
-
These results can be used when designing future studies on CPAP strategies for preterm infants in the delivery room.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Morley, C. J. et al. Nasal CPAP or intubation at birth for very preterm infants. N. Engl. J. Med. 358, 700–708 (2008).
Finer, N. N. et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl. J. Med. 362, 1970–1979 (2010).
Trevisanuto, D. et al. Changes over time in delivery room management of extremely low birth weight infants in Italy. Resuscitation 85, 1072–1076 (2014).
Crawshaw, J. R. et al. Laryngeal closure impedes non-invasive ventilation at birth. Arch. Dis. Child. Fetal Neonatal Ed. 103, F112–F119 (2018).
Harding, R., Bocking, A. D. & Sigger, J. N. Upper airway resistances in fetal sheep: the influence of breathing activity. J. Appl. Physiol. 60, 160–165 (1986).
Renolleau, S., Letourneau, P., Niyonsenga, T., Praud, J. P. & Gagne, B. Thyroarytenoid muscle electrical activity during spontaneous apneas in preterm lambs. Am. J. Respir. Crit. Care Med, 159, 1396–1404 (1999).
Moreau-Bussiere, F. et al. Laryngeal response to nasal ventilation in nonsedated newborn lambs. J. Appl. Physiol. 102, 2149–2157 (2007).
van Vonderen, J. J., Hooper, S. B., Hummler, H. D., Lopriore, E. & te Pas, A. B. Effects of a sustained inflation in preterm infants at birth. J. Pediatr. 165, 903–908. e901 (2014).
Dekker, J. et al. Caffeine to improve breathing effort of preterm infants at birth: a randomized controlled trial. Pediatr. Res. 82, 290–296 (2017).
Dekker, J. et al. The effect of initial high vs. low FiO2 on breathing effort in preterm infants at birth: a randomized controlled trial. Front. Pediatr. 7, 504 (2019).
Dekker, J. et al. Repetitive versus standard tactile stimulation of preterm infants at birth—a randomized controlled trial. Resuscitation 127, 37–43 (2018).
Dekker, J. et al. Increasing respiratory effort with 100% oxygen during resuscitation of preterm rabbits at birth. Front. Pediatr. 7, 427 (2019).
Hooper, S. B., Te Pas, A. B. & Kitchen, M. J. Respiratory transition in the newborn: a three-phase process. Arch. Dis. Child Fetal Neonatal Ed. 101, F266–F271 (2016).
Hooper, S. B. et al. Imaging lung aeration and lung liquid clearance at birth. FASEB J. 21, 3329–3337 (2007).
Siew, M. L. et al. Inspiration regulates the rate and temporal pattern of lung liquid clearance and lung aeration at birth. J. Appl. Physiol. (1985) 106, 1888–1895 (2009).
Siew, M. L. et al. The role of lung inflation and sodium transport in airway liquid clearance during lung aeration in newborn rabbits. Pediatr. Res. 73, 443–449 (2013).
Miserocchi, G., Poskurica, B. H., & Del Fabbro, M. Pulmonary interstitial pressure in anesthetized paralyzed newborn rabbits. J. Appl. Physiol. (1985) 77, 2260–2268 (1994).
Siew, M. L. et al. Surfactant increases the uniformity of lung aeration at birth in ventilated preterm rabbits. Pediatr. Res. 70, 50–55 (2011).
Bland, R. D., McMillan, D. D., Bressack, M. A. & Dong, L. Clearance of liquid from lungs of newborn rabbits. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 49, 171–177 (1980).
Kuypers, K. et al. The effect of a face mask for respiratory support on breathing in preterm infants at birth. Resuscitation 144, 178–184 (2019).
O’Donnell, C. P., Kamlin, C. O., Davis, P. G. & Morley, C. J. Crying and breathing by extremely preterm infants immediately after birth. J. Pediatr. 156, 846–847 (2010).
te Pas, A. B. et al. Establishing functional residual capacity at birth: the effect of sustained inflation and positive end-expiratory pressure in a preterm rabbit model. Pediatr. Res. 65, 537–541 (2009).
Siew, M. L. et al. Positive end-expiratory pressure enhances development of a functional residual capacity in preterm rabbits ventilated from birth. J. Appl. Physiol. (1985) 106, 1487–1493 (2009).
te Pas, A. B. et al. Optimizing lung aeration at birth using a sustained inflation and positive pressure ventilation in preterm rabbits. Pediatr. Res. 80, 85–91 (2016).
Kitchen, M. J. et al. Changes in positive end-expiratory pressure alter the distribution of ventilation within the lung immediately after birth in newborn rabbits. PLoS ONE 9, e93391 (2014).
Mulrooney, N. et al. Surfactant and physiologic responses of preterm lambs to continuous positive airway pressure. Am. J. Respir. Crit. Care Med. 171, 488–493 (2005).
Tingay, D. G. et al. Effect of sustained inflation vs. stepwise PEEP strategy at birth on gas exchange and lung mechanics in preterm lambs. Pediatr. Res. 75, 288–294 (2014).
Miedema, M. et al. Effect of nasal continuous and biphasic positive airway pressure on lung volume in preterm infants. J. Pediatr. 162, 691–697 (2013).
Bhatia, R., Davis, P. G. & Tingay, D. G. Regional volume characteristics of the preterm infant receiving first intention continuous positive airway pressure. J. Pediatr. 187, 80–88 (2017). e82.
Richardson, C. P. & Jung, A. L. Effects of continuous positive airway pressure on pulmonary function and blood gases of infants with respiratory distress syndrome. Pediatr. Res. 12, 771–774 (1978).
Magnenant, E. et al. Dynamic behavior of respiratory system during nasal continuous positive airway pressure in spontaneously breathing premature newborn infants. Pediatr. Pulmonol. 37, 485–491 (2004).
te Pas, A. B. et al. Effect of sustained inflation length on establishing functional residual capacity at birth in ventilated premature rabbits. Pediatr. Res. 66, 295–300 (2009).
Kitchen, M. J. et al. A new design for high stability pressure-controlled ventilation for small animal lung imaging. J. Instrum. 5, 1–11 (2010).
Australian Resuscitation Council, N. Z. R. C. ANZCOR Guideline 13.4—Airway Management and Mask Ventilation of the Newborn Infant. https://resus.org.au/guidelines/ (2016).
Leong, A. F., Paganin, D. M., Hooper, S. B., Siew, M. L. & Kitchen, M. J. Measurement of absolute regional lung air volumes from near-field x-ray speckles. Opt. Express 21, 27905–27923 (2013).
te Pas, A. B. et al. Spontaneous breathing patterns of very preterm infants treated with continuous positive airway pressure at birth. Pediatr. Res. 64, 281–285 (2008).
Martherus, T. et al. High-CPAP does not impede cardiovascular changes at birth in preterm sheep. Front. Pediatr. 8, 584138 (2020).
Gluckman, P. D. & Johnston, B. M. Lesions in the upper lateral pons abolish the hypoxic depression of breathing in unanaesthetized fetal lambs in utero. J. Physiol. 382, 373–383 (1987).
Davey, M. G., Moss, T. J., McCrabb, G. J. & Harding, R. Prematurity alters hypoxic and hypercapnic ventilatory responses in developing lambs. Respir. Physiol. 105, 57–67 (1996).
van Henten, T. M. A. et al. Tactile stimulation in the delivery room: do we practice what we preach? Arch. Dis. Child Fetal Neonatal Ed. 104, F661–F662 (2019).
Schmolzer, G. M. et al. Assessment of tidal volume and gas leak during mask ventilation of preterm infants in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 95, F393–F397 (2010).
Kaufman, J., Schmolzer, G. M., Kamlin, C. O. & Davis, P. G. Mask ventilation of preterm infants in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 98, F405–F410 (2013).
Schilleman, K. et al. Evaluating manual inflations and breathing during mask ventilation in preterm infants at birth. J. Pediatr. 162, 457–463 (2013).
Dysart, K. C. Physiologic basis for nasal continuous positive airway pressure, heated and humidified high-flow nasal cannula, and nasal ventilation. Clin. Perinatol. 43, 621–631 (2016).
Sankaran, K., Leahy, F. N., Cates, D., MacCallum, M. & Rigatto, H. Effect of lung inflation on ventilation and various phases of the respiratory cycle in preterm infants. Biol. Neonate 40, 160–166 (1981).
Widdicombe, J. G. & Sellick, H. Vagal deflation and inflation reflexes mediated by lung irritant receptors. Q. J. Exp. Physiol. Cogn. Med. Sci. 55, 153–163 (1970).
Haddad, G. G. & Mellins, R. B. The role of airway receptors in the control of respiration in infants: a review. J. Pediatr. 91, 281–286 (1977).
Kuypers, K. et al. Reflexes that impact spontaneous breathing of preterm infants at birth: a narrative review. Arch. Dis. Child Fetal Neonatal Ed. 105, 675–679 (2020).
Probyn, M. E. et al. Positive end expiratory pressure during resuscitation of premature lambs rapidly improves blood gases without adversely affecting arterial pressure. Pediatr. Res. 56, 198–204 (2004).
Polglase, G. R. et al. Positive end-expiratory pressure differentially alters pulmonary hemodynamics and oxygenation in ventilated, very premature lambs. J. Appl Physiol. (1985) 99, 1453–1461 (2005).
Polglase, G. R. et al. Cardiovascular and pulmonary consequences of airway recruitment in preterm lambs. J. Appl Physiol. (1985) 106, 1347–1355 (2009).
Crossley, K. J. et al. Blood gases and pulmonary blood flow during resuscitation of very preterm lambs treated with antenatal betamethasone and/or Curosurf: effect of positive end-expiratory pressure. Pediatr. Res. 62, 37–42 (2007).
Petrillo, F. et al. Pulmonary recruitment strategy in preterm neonates <29 weeks of gestational age to reduce the need for intubation in the delivery room. Am. J. Perinatol. 36, S115–S119 (2019).
Templin, L. et al. A quality improvement initiative to reduce the need for mechanical ventilation in extremely low gestational age neonates. Am. J. Perinatol. 34, 759–764 (2017).
Kanaan, Z. et al. Feasibility of combining two individualized lung recruitment maneuvers at birth for very low gestational age infants: a retrospective cohort study. BMC Pediatr. 20, 144 (2020).
Martherus, T. et al. Comparison of two respiratory support strategies for stabilization of very preterm infants at birth: a matched-pairs analysis. Front. Pediatr. 7, 3 (2019).
Acknowledgements
The authors thank the support provided by the SPring-8 Japan Synchrotron Radiation Research Institute, which was provided by the SPring-8 Program Review Committee (2016A0132), and gratefully acknowledge the expert assistance of Kentaro Uesugi, Naoto Yagi, Masato Hoshino and Hiroyuki Iwamoto for assistance to conduct our experiments at SPring-8. This experiment was supported by the National Health and Medical Research Council (NHMRC) Program Grant (606789), NHMRC Research Fellowships (SH: APP1058537) and the Victorian Government’s Operational Infrastructure Support Program. A.B.t.P. is recipient of an NWO innovational research incentives scheme (VIDI 91716428). E.V.M. was supported by a Monash University Postdoctoral Fellowship (BPF17-0066) and a NHMRC Peter Doherty Biomedical Early Career Fellowship (APP1138049). M.J.K. is a recipient of ARC Future Fellowship (FT160100454). We acknowledge travel funding provided by the International Synchrotron Access Program (ISAP) managed by the Australian Synchrotron and funded by the Australian Government (AS/IA173/12909 and ISP12221).
Author information
Authors and Affiliations
Contributions
All authors included in this paper fulfil the criteria of authorship. T.M., K.J.C., E.V.M., A.B.t.P. and S.B.H. made substantial contributions to the design of the experiment. All authors were involved in performing the experiment and obtaining data. T.M., M.K.C., M.J.K., A.B.t.P. and S.B.H. were responsible for data analysis and interpretation. T.M., A.B.t.P. and S.B.H. drafted the first version of the manuscript, after which all authors provided feedback and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martherus, T., Croughan, M.K., Crossley, K.J. et al. Higher CPAP levels improve functional residual capacity at birth in preterm rabbits. Pediatr Res 91, 1686–1694 (2022). https://doi.org/10.1038/s41390-021-01647-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01647-8
This article is cited by
-
Optimising CPAP and oxygen levels to support spontaneous breathing in preterm rabbits
Pediatric Research (2025)