Abstract
Background
Premature adrenarche is a condition of childhood adrenal androgen excess (AAE) in the absence of gonadotropin-dependent puberty, and has been linked to insulin resistance and progression to metabolic syndrome. Microbial dysbiosis is associated with progression of inflammatory states and chronic diseases. Here, we aimed to examine the salivary microbiomes of children with AAE and assess the relationship with adrenal androgens and metabolic parameters.
Methods
In a prospective cross-sectional study of children with AAE and healthy controls, adrenal and metabolic parameters were characterized and salivary microbiome was profiled using V3–V4 16S rDNA gene amplicon sequencing.
Results
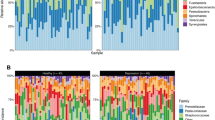
There was increased α-diversity in AAE (5 M, 15 F) compared to controls (3 M, 8 F), with positive correlation of 11OHA4, 11KA4, testosterone, androstenedione, DHEA, and DHEAS. Subanalyses showed increased α-diversity in both overweight/obese AAE and normal weight AAE compared to normal weight controls. Genus Peptostreptococcus, Veillonella, and Streptococcus salivarius were increased in normal weight AAE. Genus Prevotella, Abiotrophia, and Neisseria were increased in overweight/obese AAE.
Conclusion
These pilot data demonstrate differences in salivary microbiome profiles of children with and without AAE. Further studies are needed to assess the causal relationships between adrenal androgens, metabolic dysfunction, and salivary microbiome composition.
Impact
-
This study is the first to report the salivary microbiome of prepubertal children with adrenal androgen excess (AAE).
-
α-Diversity is increased in the salivary microbiome of children with AAE independent of weight status, and in this study cohort several serum androgens are positively associated with α-diversity.
-
Several taxa that have been associated with periodontal disease and inflammation are found to be significantly increased in AAE.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Witchel, S. F., Pinto, B., Burghard, A. C. & Oberfield, S. E. Update on adrenarche. Curr. Opin. Pediatr. 32, 574–581 (2020).
Turcu, A. F. & Auchus, R. J. Clinical significance of 11-oxygenated androgens. Curr. Opin. Endocrinol. Diabetes Obes. 24, 252–259 (2017).
Rege, J. et al. 11-Ketotestosterone is the dominant circulating bioactive androgen during normal and premature adrenarche. J. Clin. Endocrinol. Metab. 103, 4589–4598 (2018).
Wise-Oringer, B. K. et al. The unique tole of 11-oxygenated C19 steroids in both premature adrenarche and premature pubarche. Horm. Res Paediatr. 2, 1–10 (2021).
Voutilainen, R. & Jääskeläinen, J. Premature adrenarche: etiology, clinical findings, and consequences. J. Steroid Biochem. Mol. Biol. 145, 226–236 (2015).
Ribeiro, F. A. et al. Metabolic and hormonal assessment of adolescent and young adult women with prior premature adrenarche. Clinics (Sao Paulo) 74, e836 (2019).
Kaya, G. et al. Body mass index at the presentation of premature adrenarche is associated with components of metabolic syndrome at puberty. Eur. J. Pediatr. 177, 1593–1601 (2018).
Silfen, M. E. et al. Elevated free IGF-I levels in prepubertal Hispanic girls with premature adrenarche: relationship with hyperandrogenism and insulin sensitivity. J. Clin. Endocrinol. Metab. 87, 398–403 (2002).
Ibanez, L. et al. Hyperinsulinemia in postpubertal girls with a history of premature pubarche and functional ovarian hyperandrogenism. J. Clin. Endocrinol. Metab. 8, 1237–1243 (1996).
Bäckhed, F. et al. The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl Acad. Sci. USA 101, 15718–15723 (2004).
Lee, C. J., Sears, C. L. & Maruthur, N. Gut microbiome and its role in obesity and insulin resistance. Ann. NY Acad. Sci. 1461, 37–52 (2020).
Turnbaugh, P. J. et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444, 1027–1031 (2006).
Guo, Y. et al. Association between polycystic ovary syndrome and gut microbiota. PLoS ONE 11, e0153196 (2016).
Kelley, S. T., Skarra, D. V., Rivera, A. J. & Thackray, V. G. The gut microbiome is altered in a letrozole-induced mouse model of polycystic ovary syndrome. PLoS ONE 11, e0146509 (2016).
Yurtdaş, G. & Akdevelioğlu, Y. A new approach to polycystic ovary syndrome: the gut microbiota. J. Am. Coll. Nutr. 39, 371–382 (2020).
Insenser, M. et al. Gut microbiota and the polycystic ovary syndrome: influence of sex, sex hormones, and obesity. J. Clin. Endocrinol. Metab. 103, 2552–2562 (2018).
Tetel, M. J., de Vries, G. J., Melcangi, R. C., Panzica, G. & O’Mahony, S. M. Steroids, stress and the gut microbiome-brain axis. J. Neuroendocrinol. 30, https://doi.org/10.1111/jne.12548 (2018).
Sherman, S. B. et al. Prenatal androgen exposure causes hypertension and gut microbiota dysbiosis. Gut Microbes 9, 400–421 (2018).
Gulan, T., Yeernuer, T., Sui, S. & Mayinuer, N. A rat model of maternal polycystic ovary syndrome shows that exposure to androgens in utero results in dysbiosis of the intestinal microbiota and metabolic disorders of the newborn rat. Med Sci. Monit. 25, 9377–9391 (2019).
Barroso, A. et al. Neonatal exposure to androgens dynamically alters gut microbiota architecture. J. Endocrinol. 247, 69–85 (2020).
Mammadova, G., Ozkul, C., Yilmaz Isikhan, S., Acikgoz, A. & Yildiz, B. O. Characterization of gut microbiota in polycystic ovary syndrome: findings from a lean population. Eur. J. Clin. Invest. 51, e13417 (2021).
Jobira, B. et al. Obese adolescents with PCOS have altered biodiversity and relative abundance in gastrointestinal microbiota. J. Clin. Endocrinol. Metab. 105, e2134–e2144 (2020).
Torres, P. J. et al. Gut microbial diversity in women with polycystic ovary syndrome correlates with hyperandrogenism. J. Clin. Endocrinol. Metab. 103, 1502–1511 (2018).
Liu, R. et al. Dysbiosis of gut microbiota associated with clinical parameters in polycystic ovary syndrome. Front. Microbiol. 8, 324 (2017).
Vrieze, A. et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143, 913–6.e7 (2012). Erratum in: Gastroenterology. 144, 250 (2013).
Zeng, B. Structural and functional profiles of the gut microbial community in polycystic ovary syndrome with insulin resistance (IR-PCOS): a pilot study. Res. Microbiol. 170, 43–52 (2019).
He, F. F. & Li, Y. M. Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J. Ovarian Res. 13, 73 (2020).
Belstrøm, D. The salivary microbiota in health and disease. J. Oral. Microbiol. 12, 1723975 (2020).
Xiao, J., Fiscella, K. A. & Gill, S. R. Oral microbiome: possible harbinger for children’s health. Int J. Oral. Sci. 12, 12 (2020).
Mameli, C. et al. Taste perception and oral microbiota are associated with obesity in children and adolescents. PLoS ONE 14, e0221656 (2019).
Wu, Y., Chi, X., Zhang, Q., Chen, F. & Deng, X. Characterization of the salivary microbiome in people with obesity. PeerJ 16, e4458 (2018).
Triosi, J. et al. Metabolomic salivary signature of pediatric obesity related liver disease and metabolic syndrome. Nutrients 11, 274 (2019).
Janem, W. F. et al. Salivary inflammatory markers and microbiome in normoglycemic lean and obese children compared to obese children with type 2 diabetes. PLoS ONE 12, e0172647 (2017).
Lindheim, L. et al. The salivary microbiome in polycystic ovary syndrome (PCOS) and its association with disease-related parameters: a pilot study. Front Microbiol 7, 1270 (2016).
Akcalı, A. et al. Association between polycystic ovary syndrome, oral microbiota and systemic antibody responses. PLoS ONE 9, e108074 (2014).
Pappa, E., Kousvelari, E. & Vastardis, H. Saliva in the “omics” era: a promising tool in paediatrics. Oral. Dis. 25, 16–25 (2019).
Chou, J. H., Roumiantsev, S. & Singh, R. PediTools electronic growth chart calculators: applications in clinical care, research, and quality improvement. J. Med. Internet Res. 22, e16204 (2020).
Shypailo, R. J. Age-Based Pediatric Blood Pressure Reference Charts. Baylor College of Medicine, Children’s Nutrition Research Center, Body Composition Laboratory, Houston, TX. https://www.bcm.edu/bodycomplab/BPappZjs/BPvAgeAPPz.html (2019).
Fernández, J. R., Redden, D. T., Pietrobelli, A. & Allison, D. B. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J. Pediatr. 145, 439–444 (2004).
Wright, C., O’Day, P., Alyamani, M., Sharifi, N. & Auchus, R. J. Abiraterone acetate treatment lowers 11-oxygenated androgens. Eur. J. Endocrinol. 182, 413–421 (2020).
de Ferranti, S. D. et al. Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation 110, 2494–2497 (2004).
Callahan, B. J. et al. DADA2: high-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
DeSantis, T. Z. et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl Environ. Microbiol. 72, 5069–5072 (2006).
McMurdie, P. J. & Phyloseq, H. S. An R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE 8, e61217 (2013).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Westfall P. H. & Young S. S. Resampling-Based Multiple Testing: Examples and Methods for P-Value Adjustment (Wiley, 1993).
Turnbaugh, P. J. et al. A core gut microbiome in obese and lean twins. Nature 457, 480–484 (2009).
Le Chatelier, E. et al. Richness of human gut microbiome correlates with metabolic markers. Nature 500, 541–546 (2013).
Riggio, M. P., Lennon, A. & Smith, A. Detection of peptostreptococcus micros DNA in clinical samples by PCR. J. Med. Microbiol. 50, 249–254 (2001).
Zhou, J. et al. Exploration of human salivary microbiomes—insights into the novel characteristics of microbial community structure in caries and caries-free subjects. PLoS ONE 11, e0147039 (2016).
Gross, E. L. et al. Beyond Streptococcus mutans: dental caries onset linked to multiple species by 16S rRNA community analysis. PLoS ONE 7, e47722 (2012).
Alauzet, C., Marchandin, H. & Lozniewski, A. New insights into Prevotella diversity and medical microbiology. Future Microbiol. 5, 1695–1718 (2010).
Larsen, J. M. The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology 151, 363–374 (2017).
Zhu, C. et al. The predictive potentiality of salivary microbiome for the recurrence of early childhood caries. Front, Cell Infect. Microbiol. 8, 423 (2018).
Porwal, S., Tewari, S., Sharma, R. K., Singhal, S. R. & Narula, S. C. Periodontal status and high-sensitivity C-reactive protein levels in polycystic ovary syndrome with and without medical treatment. J. Periodontol. 85, 1380–1389 (2014).
Rahiminejad, M. E. et al. Comparison of prevalence of periodontal disease in women with polycystic ovary syndrome and healthy controls. Dent. Res J. (Isfahan) 12, 507–512 (2015).
Acknowledgements
We thank the members of the Division of Pediatric Endocrinology, Diabetes and Metabolism at Columbia University Irving Medical Center (New York, NY) for their referral of eligible subjects, and the subjects and their families for agreeing to participate. We thank the members of the Microbiome & Pathogen Genomics Collaborative Center for technical support. We thank Rachel Tao, B.A., for her initial help with patient recruitment and coordination of study visits. We also thank Ismael Castaneda, R.N. and the staff of the Clinical Research Resource at Columbia Irving Institute for Clinical and Translational Research (UL1TR001873) for their valuable help in conducting the study visits. With gratitude we acknowledge Esoterix Laboratory and the Columbia Biomarkers Core Laboratory for performing laboratory measurements for this study. This work was supported in part by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases Grant 5T32DK065522-14 (to B.K.W.-O. and S.E.O.) and by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR001873. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
B.K.W.-O., A.C.B., H.P., R.J.A., S.E.O., and A.-C.U. made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. B.K.W.-O., A.C.B., H.P., S.E.O., and A.-C.U. were involved in drafting the article or revising it critically for important intellectual content. R.J.A., S.E.O., and A.-C.U. provided final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Informed consent was obtained for all study subjects prior to enrollment. For patients less than 7 years of age, informed consent was obtained from the parent or legal guardian. For patients 7 years or older, informed consent and assent were obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wise-Oringer, B.K., Burghard, A.C., Park, H. et al. Salivary microbiome differences in prepubertal children with and without adrenal androgen excess. Pediatr Res 91, 1797–1803 (2022). https://doi.org/10.1038/s41390-021-01661-w
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01661-w
This article is cited by
-
Causal Link between Gut Microbiota and Infertility: A Two-sample Bidirectional Mendelian Randomization Study
Current Medical Science (2024)