Abstract
Background
Children with Down syndrome are at risk for significant pulmonary co-morbidities, including recurrent respiratory infections, dysphagia, obstructive sleep apnea, and pulmonary vascular disease. Because the gold standard metric of lung function, spirometry, may not be feasible in children with intellectual disabilities, we sought to assess the feasibility of both airwave oscillometry and spirometry in children with Down syndrome.
Methods
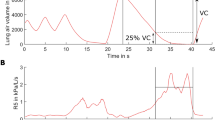
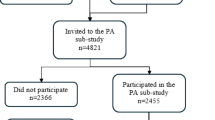
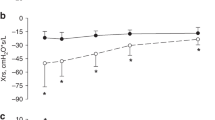
Thirty-four children with Down syndrome aged 5–17 years were recruited. Participants performed airwave oscillometry and spirometry before and 10 min after albuterol. Outcomes include success rates, airway resistance and reactance pre- and post-bronchodilator, and bronchodilator response.
Results
Participants were median age 9.2 years (interquartile range 7.2, 12.0) and 47% male. Airwave oscillometry was successful in 26 participants (76.5%) and 4 (11.8%) were successful with spirometry. No abnormalities in airway resistance were detected, and 16/26 (61.5%) had decreased reactance. A positive bronchodilator response by oscillometry was observed in 5/23 (21.7%) of those with successful pre- and post-bronchodilator testing.
Conclusions
Measures of pulmonary function were successfully obtained using airwave oscillometry in children with Down syndrome, which supports its use in this high-risk population.
Impact
-
Children with Down syndrome are at risk for significant pulmonary co-morbidities, but the gold standard metric of lung function, spirometry, may not be feasible in children with intellectual disabilities. This may limit the population’s enrollment in clinical trials and in standardized clinical care.
-
In this prospective study of lung function in children with Down syndrome, airwave oscillometry was successful in 76% of participants but spirometry was successful in only 12%.
-
This study reinforces that measures of pulmonary function can be obtained successfully using airwave oscillometry in children with Down syndrome, which supports its use in this high-risk population.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Colvin, K. L. & Yeager, M. E. What people with Down syndrome can teach us about cardiopulmonary disease. Eur. Respir. Rev. 26, 160098 (2017).
McDowell, K. M. & Craven, D. I. Pulmonary complications of Down syndrome during childhood. J. Pediatr. 158, 319–325 (2011).
Pandit, C. & Fitzgerald, D. A. Respiratory problems in children with Down syndrome. J. Paediatr. Child Health 48, E147–E152 (2012).
Khalili, M. A. & Elkins, M. R. Aerobic exercise improves lung function in children with intellectual disability: a randomised trial. Aust. J. Physiother. 55, 171–175 (2009).
El Kafy, E. M. & Helal, O. F. Effect of rowing on pulmonary functions in children with Down syndrome. Pediatr. Phys. Ther. 26, 437–445 (2014).
Pastore, E. et al. Clinical and cardiorespiratory assessment in children with Down syndrome without congenital heart disease. Arch. Pediatr. Adolesc. Med. 154, 408–410 (2000).
Dichter, C. C., Darbee, J. C., Effgen, S. K. & Palisano, R. J. Assessment of pulmonary function and physical fitness in children with Down syndrome. Pediatr. Phys. Ther. 5, 3–8 (1993).
Salgueirinho, C., Venâncio, J., Martin-Nogueras, A. M. & Ribeiro, F. Pulmonary function in young adults with Down syndrome: a cross-sectional study. Int. Med. Rev. Down Syndr. 20, 17–20 (2015).
Laibsirinon, S., Jarusurin, N., Kokoi, C. & Manakiatichai, T. Pulmonary function and chest expansion in Thai boys with Down syndrome. Thammasat Med. J. 12, 269–275 (2012).
Komarow, H. D. et al. A study of the use of impulse oscillometry in the evaluation of children with asthma: analysis of lung parameters, order effect, and utility compared with spirometry. Pediatr. Pulmonol. 47, 18–26 (2012).
Fernandez-Plata, R. et al. Quality of pulmonary function tests in participants with Down syndrome. Arch. Bronconeumol. 55, 513–518 (2019).
Harris, P. A. et al. Research Electronic Data Capture (Redcap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
Beydon, N. et al. An official American Thoracic Society/European Respiratory Society Statement: pulmonary function testing in preschool children. Am. J. Respir. Crit. Care Med. 175, 1304–1345 (2007).
King, G. G. et al. Technical standards for respiratory oscillometry. Eur. Respir. J. 55, 1900753 (2020).
Nowowiejska, B. et al. Transient reference values for impulse oscillometry for children aged 3–18 years. Pediatr. Pulmonol. 43, 1193–1197 (2008).
Culver, B. H. et al. Recommendations for a standardized pulmonary function report. An Official American Thoracic Society Technical Statement. Am. J. Respir. Crit. Care Med. 196, 1463–1472 (2017).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343 (2012).
Pellegrino, R. et al. Interpretative strategies for lung function tests. Eur. Respir. J. 26, 948–968 (2005).
Asher, M. I. et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur. Respir. J. 8, 483–491 (1995).
Bertrand, P., Navarro, H., Caussade, S., Holmgren, N. & Sanchez, I. Airway anomalies in children with Down syndrome: endoscopic findings. Pediatr. Pulmonol. 36, 137–141 (2003).
De Lausnay, M. et al. The prevalence of lower airway anomalies in children with Down syndrome compared to controls. Pediatr. Pulmonol. 55, 1259–1263 (2020).
Fockens, M. M., Holscher, M., Limpens, J. & Dikkers, F. G. Tracheal anomalies associated with Down syndrome: a systematic review. Pediatr. Pulmonol. 56, 814–822 (2021).
Malmberg, L. P. et al. Lung function measured by the oscillometric method in prematurely born children with chronic lung disease. Eur. Respir. J. 16, 598–603 (2000).
Brostrom, E. B., Thunqvist, P., Adenfelt, G., Borling, E. & Katz-Salamon, M. Obstructive lung disease in children with mild to severe Bpd. Respir. Med. 104, 362–370 (2010).
Sol, I. S. et al. Assessment of within-breath impulse oscillometry parameters in children with asthma. Pediatr. Pulmonol. 54, 117–124 (2019).
Fielding, D. I. et al. Expiratory reactance abnormalities in patients with expiratory dynamic airway collapse: a new application of impulse oscillometry. ERJ Open Res. 4, 00080–2018 (2018).
Kuo, C. R., Jabbal, S. & Lipworth, B. I say Ios you say Aos: comparative bias in respiratory impedance measurements. Lung 197, 473–481 (2019).
Weijerman, M. E., Brand, P. L., van Furth, M. A., Broers, C. J. & Gemke, R. J. Recurrent wheeze in children with Down syndrome: is it asthma? Acta Paediatr. 100, e194–e197 (2011).
Acknowledgements
This publication is supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535, allowing the use of REDCap for data storage and R21 HL151261-01 (to E.D.B.). Contents are the authors’ sole responsibility and do not necessarily represent official NIH views. We would also like to thank the Global Down Syndrome Foundation and the Anna and John J. Sie Foundation for their financial support of research conducted at the Sie Center for Down Syndrome at Children’s Hospital Colorado.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
E.D.B. is a consultant of EvoEndoscopy (formerly TripleEndoscopy Inc.) and is listed as a co-inventor on patents related to endoscopy. E.D.B. also receives funding from the Cystic Fibrosis Foundation and NIH, and is a consultant for Boehringer Ingelheim, not related to this project. The remaining authors declare no competing interests.
Consent statement
Informed consent was obtained from the parent or legal guardian before study procedures and assent was obtained from children aged 7 years or older, if developmentally able.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vielkind, M.L., Hamlington, K.L., Wolter-Warmerdam, K. et al. Airwave oscillometry to measure lung function in children with Down syndrome. Pediatr Res 91, 1775–1780 (2022). https://doi.org/10.1038/s41390-021-01664-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01664-7
This article is cited by
-
Association Between the Skeletal Muscle Mass Index and Physical Function in Adolescents with Intellectual and Developmental Disabilities
Advances in Neurodevelopmental Disorders (2025)