Abstract
Background
In phenylketonuria, treatment and subsequent lowering of phenylalanine levels usually occur within the first month of life. This study investigated whether different indicators of metabolic control during the neonatal period were associated with IQ during late childhood/early adolescence.
Methods
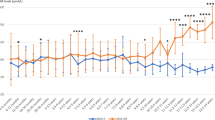
Overall phenylalanine concentration during the first month of life (total “area under the curve”), proportion of phenylalanine concentrations above upper target level (360 μmol/L) and proportion below lower target level (120 μmol/L) during this period, diagnostic phenylalanine levels, number of days until phenylalanine levels were <360 μmol/L, and lifetime and concurrent phenylalanine levels were correlated with IQ scores of 64 PKU patients (mean age 10.8 years, SD 2.9).
Results
Overall phenylalanine concentration and proportion of phenylalanine concentrations >360 μmol/L during the first month of life negatively correlated with IQ in late childhood/early adolescence. Separately, phenylalanine concentrations during different periods within the first month of life (0–10 days, 11–20 days, 21–30 days) were negatively correlated with later IQ as well, but correlation strengths did not differ significantly. No further significant associations were found.
Conclusions
In phenylketonuria, achievement of target-range phenylalanine levels during the neonatal period is important for cognition later in life, also when compared to other indicators of metabolic control.
Impact
-
In phenylketonuria, it remains unclear during which age periods or developmental stages metabolic control is most important for later cognitive outcomes.
-
Phenylalanine levels during the neonatal period were clearly and negatively related to later IQ, whereas no significant associations were observed for other indices of metabolic control. This emphasizes the relative importance of this period for cognitive development in phenylketonuria.
-
No further distinctions were observed in strength of associations with later IQ between different indicators of metabolic control during the neonatal period. Thus, achievement of good metabolic control within 1 month after birth appears “safe” with respect to later cognitive outcomes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Blau, N., Van Spronsen, F. J. & Levy, H. L. Phenylketonuria. Lancet 376, 1417–1427 (2010).
Van Spronsen, F. J. Phenylketonuria: a 21st century perspective. Nat. Rev. Endocrinol. 6, 509–514 (2010).
Kure, S. et al. Tetrahydrobiopterin-responsive phenylalanine hydroxylase deficiency. J. Pediatr. 135, 375–378 (1999).
De Groot, M. J., Hoeksma, M., Blau, N., Reijngoud, D. J. & Van Spronsen, F. J. Pathogenesis of cognitive dysfunction in phenylketonuria: review of hypotheses. Mol. Genet. Metab. 99, S86–S89 (2010).
Longo, N. et al. Single-dose, subcutaneous recombinant phenylalanine ammonia lyase conjugated with polyethylene glycol in adult patients with phenylketonuria: an open-label, multicentre, phase 1 dose-escalation trial. Lancet 384, 37–44 (2014).
Harding, C. O. et al. Pegvaliase for the treatment of phenylketonuria: A pivotal, double-blind randomized discontinuation Phase 3 clinical trial. Mol. Genet. Metab. 124, 20–26 (2018).
Goldfinger, M. et al. Partial rescue of neuropathology in the murine model of PKU following administration of recombinant phenylalanine ammonia lyase (pegvaliase). Mol. Genet. Metab. 122, 33–35 (2017).
Enns, G. M. et al. Suboptimal outcomes in patients with PKU treated early with diet alone: revisiting the evidence. Mol. Genet. Metab. 101, 99–109 (2010).
Moyle, J. J., Fox, A. M., Arthur, M., Bynevelt, M. & Burnett, J. R. Meta-analysis of neuropsychological symptoms of adolescents and adults with PKU. Neuropsychol. Rev. 17, 91–101 (2007).
Albrecht, J., Garbade, S. F. & Burgard, P. Neuropsychological speed tests and blood phenylalanine levels in patients with phenylketonuria: a meta-analysis. Neurosci. Biobehav. Rev. 33, 414–421 (2009).
Huijbregts, S. C., De Sonneville, L. M., Van Spronsen, F. J., Licht, R. & Sergeant, J. A. The neuropsychological profile of early and continuously treated phenylketonuria: orienting, vigilance, and maintenance versus manipulation-functions of working memory. Neurosci. Biobehav. Rev. 26, 697–712 (2002).
Waisbren, S. E. et al. Phenylalanine blood levels and clinical outcomes in phenylketonuria: a systematic literature review and meta-analysis. Mol. Genet. Metab. 92, 63–70 (2007).
Weglage, J. et al. Neurocognitive functioning in adults with phenylketonuria: results of a long term study. Mol. Genet. Metab. 110, S44–S48 (2013).
Jahja, R. et al. Long-term follow-up of cognition and mental health in adult phenylketonuria: a PKU-COBESO study. Behav. Genet. 47, 486–497 (2017).
Van Spronsen, F. J. et al. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 5, 743–756 (2017).
Vockley, J. et al. Phenylalanine hydroxylase deficiency: diagnosis and management guideline. Genet. Med. 16, 188–200 (2014).
Jahja, R., Huijbregts, S. C., De Sonneville, L. M., Van der Meere, J. J. & Van Spronsen, F. J. Neurocognitive evidence for revision of treatment targets and guidelines for phenylketonuria. J. Pediatr. 164, 895–899 (2014).
Viau, K. S. et al. Correlation of age-specific phenylalanine levels with intellectual outcome in patients with phenylketonuria. J. Inherit. Metab. Dis. 34, 963–971 (2011).
Huijbregts, S. C. J. et al. Sustained attention and inhibition of cognitive interference in treated phenylketonuria: associations with concurrent and lifetime phenylalanine concentrations. Neuropsychologia 40, 7–15 (2002).
Posner, M. I. & Rothbart, M. K. Temperament and brain networks of attention. Philos. Trans. R. Soc. Lond. B Biol. Sci. 373, 20170254 (2018).
Somerville, L. H. & Casey, B. J. Developmental neurobiology of cognitive control and motivational systems. Curr. Opin. Neurbiol. 20, 236–241 (2010).
Burgard, P., Rey, F., Rupp, A., Abadie, V. & Rey, J. Neuropsychologic functions of early treated patients with phenylketonuria, on and off diet: results of a cross-national and cross-sectional study. Pediatr. Res. 41, 368–374 (1997).
Van der Schot, L. W., Doesburg, W. H. & Sengers, R. C. The phenylalanine response curve in relation to growth and mental development in the first year of life. Acta Paediatr. 407, 68–69 (1994).
Smith, I., Beasley, M. G. & Ades, A. E. Intelligence and quality of dietary treatment in phenylketonuria. Arch. Dis. Child. 65, 472–478 (1990).
Jahja, R. et al. Mental health and social functioning in early treated phenylketonuria: the PKU-COBESO study. Mol. Genet. Metab. 110, S57–S61 (2013).
Feldmann, R., Denecke, J., Grenzebach, M. & Weglage, J. Frontal lobe-dependent functions in treated phenylketonuria: blood phenylalanine concentrations and long-term deficits in adolescents and young adults. J. Inherit. Metab. Dis. 28, 445–455 (2005).
Weglage, J. et al. Behavioural and emotional problems in early-treated adolescents with phenylketonuria in comparison with diabetic patients and healthy controls. J. Inherit. Metab. Dis. 23, 487–496 (2000).
Kort, W. et al. Wechsler Intelligence Scale for Children-III-NL (Pearson Clinical and Talent Assessment, 2005).
Petermann, F. F. & Petermann, U. (eds.) HAWIK-IV 3rd edn (Huber, 2010).
McCabe, E. R., McCabe, L., Mosher, G. A., Allen, R. J. & Berman, J. L. Newborn screening for phenylketonuria: predictive validity as a function of age. Pediatrics 72, 390–398 (1983).
RStudio. RStudio: integrated development environment for R (version 1.1.453). http://www.rstudio.org (2012).
Eid, M., Gollwitzer, M. & Schmitt, M. Statistik und Forschungsmethoden Lehrbuch (Beltz, 2011).
Lenhard, W. & Lenhard, A. Hypothesis Tests for Comparing Correlations (Psychometrica, 2014).
Christ, S. E., Huijbregts, S. C., De Sonneville, L. M. & White, D. A. Executive function in early-treated phenylketonuria: profile and underlying mechanisms. Mol. Genet. Metab. 99, S22–S32 (2010).
Huijbregts, S. C., Gassio, R. & Campistol, J. Executive functioning in context: Relevance for treatment and monitoring of phenylketonuria. Mol. Genet. Metab. 110, S25–S30 (2013).
DeRoche, K. & Welsh, M. Twenty-five years of research on neurocognitive outcomes in early-treated phenylketonuria: intelligence and executive function. Dev. Neuropsychol. 33, 474–504 (2008).
Cleary, M. et al. Fluctuations in phenylalanine concentrations in phenylketonuria: A review of possible relationships with outcomes. Mol. Genet. Metab. 110, 418–423 (2013).
Zeman, J. et al. Intellectual and school performance in adolescents with phenylketonuria according to their dietary compliance. The Czech-Slovak Collaborative Study. Eur. J. Pediatr. 155, S56–S58 (1996).
Gonzalez, M. J. et al. Neurological complications and behavioral problems in patients with phenylketonuria in a Follow-up Unit. Mol. Genet. Metab. 104, S73–S79 (2011).
Van Vliet, D. et al. Infants with Tyrosinemia Type 1: should phenylalanine be supplemented? JIMD Rep. 18, 117–124 (2015).
Van Vliet, K. et al. Emotional and behavioral problems, quality of life and metabolic control in NTBC-treated Tyrosinemia type 1 patients. Orphanet J. Rare Dis. 14, 285 (2019).
Author information
Authors and Affiliations
Contributions
G.B.L., S.C.J.H., F.R., J.G., M.B. and F.J.v.S. contributed to conception and design of the study and the analysis and interpretation of data. G.B.L., F.R., R.F., R.J. and U.O. contributed to acquisition of data. All authors contributed to drafting the article or revising it critically for intellectual content.
Corresponding author
Ethics declarations
Competing interests
S.C.J.H. has participated in strategic advisory boards and received grants and honoraria as a consultant and/or speaker from Biomarin, Merck- Serono, Homology Medicines, and Nutricia. R.J. has received honoraria as a speaker and consultant from Merck- Serono and Biomarin. F.J.v.S. has received research grants, advisory board fees, and speaker’s honoraria from Nutricia Research, Merck-Serono, Biomarin, Codexis, Alexion, Vitaflo, MendeliKABS, Promethera, SOBI, APR, and ARLA Foods Int. G.B.L., F.R., R.F., J.W., U.O. and J.G.M.B. declared that they do not have potential conflicts of interest.
Ethics approval and consent to participate
Participants and/or parents gave written informed consent to participate in the study and for using their data in this report.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liemburg, G.B., Huijbregts, S.C.J., Rutsch, F. et al. Metabolic control during the neonatal period in phenylketonuria: associations with childhood IQ. Pediatr Res 91, 874–878 (2022). https://doi.org/10.1038/s41390-021-01728-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01728-8
This article is cited by
-
Decoding rare inherited metabolic disorders: advancing precision in screening and diagnosis
Orphanet Journal of Rare Diseases (2026)
-
The relationship between adult phenylketonuria and the cardiovascular system - insights into mechanisms and risks
Orphanet Journal of Rare Diseases (2025)
-
Intelligence quotient scores among early-treated phenylketonuria patients: results from a systematic literature review
Orphanet Journal of Rare Diseases (2025)
-
Neuropsychological profile of French adults with early-treated phenylketonuria: a multicenter study
Journal of Neurology (2025)
-
Genetic etiology and clinical challenges of phenylketonuria
Human Genomics (2022)