Abstract
Background
Heart rate (HR) is a biomarker used to measure physiological function, health status and cardiovascular autonomic function. The purpose of this study was to determine sex- and age-specific reference values for cardiac autonomic function at rest, during maximal exercise and the recovery phase in prepubertal children.
Methods
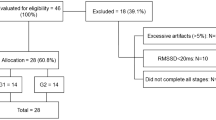
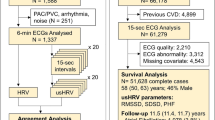
Five hundred and twelve healthy children 7–11 years of age performed a Léger test. A heart RR-interval monitor recorded the heart data and a specific software analysed the cardiac autonomic response through HR and HR variability (HRV). It analysed HR before the test (resting HR, RHR), during the test (HRpeak) and HR recovery (HRR) in the first minute (HRR1) and the fifth minute (HRR5). The values are mean ± SD.
Results
Collectively, 91.2% of girls and 92.3% of boys were within the recommended ranges regarding RHR. The average HRpeak was 199 ± 10.83 b.p.m. and 96.8% of girls and 95.3% of boys were within the minimum threshold value recommended (180 b.p.m.). Boys showed lower values of RHR than girls (p < 0.001) and larger values of HRR 1 and HRR5 (p < 0.001).
Conclusions
This study comprehensively provides a reference set of data for the most important HR variables that can be obtained during exercise testing in prepubertal children regarding age and sex and in a field setting.
Impact
-
This is the first study to provide reference values of autonomic cardiac function at rest, during maximal exercise and during the recovery period in prepubertal children aged 7–11 years.
-
Despite the early age of participants, cardiorespiratory fitness, RHR and HRR are different according to sex.
-
Aerobic performance and HRpeak have a negative correlation with body mass index and cardiometabolic risk.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ahn, S. & Fedewa, A. L. A meta-analysis of the relationship between children’s physical activity and mental Health. J. Pediatr. Psychol. 36, 385–397 (2011).
Martínez-Gómez, D. et al. Sedentary behavior, adiposity, and cardiovascular risk factors in adolescents. The AFINOS study. Rev. Esp. Cardiol. 63, 277–285 (2010).
Salmon, J., Tremblay, M. S., Marshall, S. J. & Hume, C. Health risks, correlates, and interventions to reduce sedentary behavior in young people. Am. J. Prev. Med. 41, 197–206 (2011).
Bongers-Karmaoui, M. N., Jaddoe, V. W. V., Roest, A. A. W. & Gaillard, R. The cardiovascular stress response as early life marker of cardiovascular health: applications in population-based pediatric studies—a narrative review. Pediatr. Cardiol. 41, 1739–1755 (2020).
Billman, G. E., Sacha, J., Werner, B., Jelen, P. J. & Gąsior, J. S. Editorial: heart rate variability and other autonomic markers in children and adolescents. Front. Physiol. 11, 1265 (2019).
Evans, C. A., Selvadurai, H., Baur, L. A. & Waters, K. A. Effects of obstructive sleep apnea and obesity on exercise function in children. Sleep 37, 1103–1110 (2014).
Metwalley, K. A., Hamed, S. A. & Farghaly, H. S. Cardiac autonomic function in children with type 1 diabetes. Eur. J. Pediatr. 177, 805–813 (2018).
Schuster, I. et al. Cardiac function during exercise in obese prepubertal boys: effect of degree of obesity. Obesity 17, 1878–1883 (2009).
Freeman, J. V., Dewey, F. E., Hadley, D. M., Myers, J. & Froelicher, V. F. Autonomic nervous system interaction with the cardiovascular system during exercise. Prog. Cardiovasc. Dis. 48, 342–362 (2006).
Plaza-Florido, A. et al. Heart rate is a better predictor of cardiorespiratory fitness than heart rate variability in overweight/obese children: the Activebrains project. Front. Physiol. 10, 510 (2019).
Fernandes, R. A. et al. Resting heart rate is associated with blood pressure in male children and adolescents. J. Pediatr. 158, 634–637 (2011).
Clausen, H., Theophilos, T., Jackno, K. & Babl, F. E. Paediatric arrhythmias in the emergency department. Emerg. Med. J. 29, 732–737 (2012).
Baruteau, A. E., Perry, J. C., Sanatani, S., Horie, M. & Dubin, A. M. Evaluation and management of bradycardia in neonates and children. Eur. J. Pediatr. 175, 151–161 (2016).
Alom, M. M. et al. Physical training induced resting bradycardia and its association with cardiac autonomic nervous activities. Mymensingh Med. J. 20, 665–670 (2011).
Obert, P. et al. Effect of aerobic training and detraining on left ventricular dimensions and diastolic function in prepubertal boys and girls. Int. J. Sports Med. 22, 90–96 (2001).
Rowland, T. W. in The Young Athlete (eds Helge, H. & Oded, B.-O.) Ch. 4, 39–49 (Oxford, Blackwell, 2008).
Triposkiadis, F. et al. Cardiac adaptation to intensive training in prepubertal swimmers. Eur. J. Clin. Invest. 32, 16–23 (2002).
Cataldo, A. et al. Assessment of autonomic function as marker of training status: the role of heart rate recovery after exercise. Eur. J. Sport Stud. 2, 89–97 (2014).
Brubaker, P. H. & Kitzman, D. W. Chronotropic incompetence: causes, consequences, and management. Circulation 123, 1010–1020 (2011).
Baba, R., Iwagaki, S., Tauchi, N. & Tsurusawa, M. Is the chronotropic index applicable to children and adolescents? Circ. J. 69, 471–474 (2005).
Simhaee, D. et al. Recovery heart rate: an indicator of cardiovascular risk among middle school children. Pediatr. Cardiol. 34, 1431–1437 (2013).
Ortega, F. B., Ruiz, J. R., Castillo, M. J. & Sjöström, M. Physical fitness in childhood and adolescence: a powerful marker of health. Int. J. Obes. 32, 1–11 (2008).
Akdur, H. et al. The evaluation of cardiovascular response to exercise in healthy Turkish children. Turk. J. Pediatr. 51, 472–477 (2009).
Gasior, J. S. et al. Normative values for heart rate variability parameters in school-aged children: simple approach considering differences in average heart rate. Front. Physiol. 24, 1495 (2018).
Veijalainen, A. et al. Associations of physical activity, sedentary time, and cardiorespiratory fitness with heart rate variability in 6- to 9-year-old children: the PANIC study. Eur. J. Appl. Physiol. 119, 2487–2498 (2019).
Oliveira, R. S., Barker, A. R., Wilkinson, K. M., Abbott, R. A. & Williams, C. A. Is cardiac autonomic function associated with cardiorespiratory fitness and physical activity in children and adolescents? A systematic review of cross-sectional studies. Int. J. Cardiol. 236, 113–122 (2017).
Faul, F., Erdfelder, E., Lang, A. & Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191 (2007).
Tanner, jM. Growth at adolescence. Eugen. Rev. 49, 37–38 (1957).
Chung, I. H., Park, S., Park, M. J. & Yoo, E. G. Waist-to-height ratio as an index for cardiometabolic risk in adolescents: results from the 1998−2008 KNHANES. Yonsei Med. J. 57, 658–663 (2016).
Léger, L. A., Mercier, D., Gadoury, C. & Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 6, 93–101 (1988).
Borg, G. A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 14, 377–381 (1982).
Parak, J. et al. Evaluation of the beat-to-beat detection accuracy of pulse on wearable optical heart rate monitor. In 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) 2015-November, 8099–8102 (IEEE, 2015).
Parak, J. & Korhonen, I. Accuracy of Firstbeat Bodyguard 2 Beat-to-Beat Heart Rate Monitor. White Paper 1–3 (2013).
European Society of Cardiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93, 1043–1065 (1996).
Sami, S., Mikko, S. & Antti, K. Advanced methods for processing bioelectrical signals artefact correction for heart beat iinterval data. Adv. Methods Process. Bioelectrical Signals 1–10 (2004). https://www.firstbeat.com/app/uploads/2015/10/saalasti_et_al_probisi_2004_congress.pdf
Routledge, F. S., Campbell, T. S., McFetridge-Durdle, J. A. & Bacon, S. L. Improvements in heart rate variability with exercise therapy. Can. J. Cardiol. 26, 303–312 (2010).
Bobkowski, W. et al. Measures of heart rate variability in 24-h ECGs depend on age but not gender of healthy children. Front. Physiol. 8, 311 (2017).
Cachadiña, E. S. et al. Heart rate variability is lower in patients with intermittent claudication: a preliminary study. Arch. Med. Deporte 35, 218–221 (2018).
von Scheidt, F. et al. Heart rate response during treadmill exercise test in children and adolescents with congenital heart disease. Front. Pediatr. 7, 65 (2019).
Easley, E. A. et al. Recovery responses to maximal exercise in healthy-weight children and children with obesity. Res. Q. Exerc. Sport 89, 38–46 (2018).
Guilkey, J. P., Overstreet, M. & Mahon, A. D. Heart rate recovery and parasympathetic modulation in boys and girls following maximal and submaximal exercise. Eur. J. Appl. Physiol. 115, 2125–2133 (2015).
Hager, A. Normal values for cardiopulmonary exercise testing in children. Eur. J. Prev. Cardiol. 18, 675 (2011).
Young, F. L. S. & Leicht, A. S. Short-term stability of resting heart rate variability: influence of position and gender. Appl. Physiol. Nutr. Metab. 36, 210–218 (2011).
Speer, K. E., Semple, S., Naumovski, N. & McKune, A. J. Measuring heart rate variability using commercially available devices in healthy children: a validity and reliability study. Eur. J. Investig. Health Psychol. Educ. 10, 390–404 (2020).
Buchheit, M. et al. Supramaximal training and postexercise parasympathetic reactivation in adolescents. Med. Sci. Sport. Exerc. 40, 362–371 (2008).
Bentley, R. F. et al. Heart rate variability and recovery following maximal exercise in endurance athletes and physically active individuals. Appl. Physiol. Nutr. Metab. 45, 1138–1144 (2020).
Hopkins, W. G., Marshall, S. W., Batterham, A. M. & Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 41, 3–13 (2009).
Sarganas, G., Schaffrath Rosario, A. & Neuhauser, H. K. Resting heart rate percentiles and associated factors in children and adolescents. J. Pediatr. 187, 174–181.e3 (2017).
Kwok, S. Y. et al. Resting heart rate in children and adolescents: association with blood pressure, exercise and obesity. Arch. Dis. Child. 98, 287–291 (2013).
Rabbia, F. et al. Assessing resting heart rate in adolescents: determinants and correlates. J. Hum. Hypertens. 16, 327–332 (2002).
Souza, N. Mde et al. Heart rate variability in obese children. J. Hum. Growth Dev. 22, 328–333 (2012).
Davy, K. P. & Hall, J. E. Obesity and hypertension: two epidemics or one?. Am. J. Physiol. Integr. Comp. Physiol. 286, R803–R813 (2004).
Ørntoft, C. et al. Physical fitness and body composition in 10-12-year-old Danish children in relation to leisure-time club-based sporting activities. Biomed. Res. Int. 27, 9807569 (2018).
Pieles, G. E. & Stuart, A. G. The adolescent athlete’s heart; A miniature adult or grown‐up child? Clin. Cardiol. 43, 852–862 (2020).
Larsen, M. N. et al. Cardiovascular adaptations after 10 months of intense school‐based physical training for 8‐ to 10‐year‐old children. Scand. J. Med. Sci. Sports 28, 33–41 (2018).
Krustrup, P. et al. Structural and functional cardiac adaptations to a 10‐week school‐based football intervention for 9–10‐year‐old children. Scand. J. Med. Sci. Sports 24, 4–9 (2014).
Buchheit, M., Platat, C., Oujaa, M. & Simon, C. Habitual physical activity, physical fitness and heart rate variability in preadolescents. Int. J. Sports Med. 28, 204–210 (2007).
Advanced Life Support Group. Advanced Paediatric Life Support: A Practical Approach to Emergencies (APLS) (Advanced Life Support Group, 2016).
Gelbart, M., Ziv-Baran, T., Williams, C. A., Yarom, Y. & Dubnov-Raz, G. Prediction of maximal heart rate in children and adolescents. Clin. J. Sport Med. 27, 139–144 (2017).
Fomin, Å. et al. Sex differences in response to maximal exercise stress test in trained adolescents. BMC Pediatr. 12, 127 (2012).
Verschuren, O., Maltais, D. B. & Takken, T. The 220-age equation does not predict maximum heart rate in children and adolescents. Dev. Med. Child Neurol. 53, 861–864 (2011).
Nikolaidis, P. et al. The effect of body mass index on acute cardiometabolic responses to graded exercise testing in children: a narrative review. Sports 6, 103 (2018).
Axley, J. D. & Werk, L. N. Relationship between abdominal adiposity and exercise tolerance in children with obesity. Pediatr. Phys. Ther. 28, 386–391 (2016).
Reybrouck, T., Weymans, M., Vinckx, J., Stijns, H. & Vanderschueren‐Lodeweyckx, M. Cardiorespiratory function during exercise in obese children. Acta Paediatr. 76, 342–348 (1987).
Participating, N. & Several, N. Exercise intolerance. ERS Handb. Paediatr. Respir. Med. 65, 65–69 (2013).
Van Brussel, M., Bongers, B. C., Hulzebos, E. H. J., Burghard, M. & Takken, T. A systematic approach to interpreting the cardiopulmonary exercise test in pediatrics. Pediatr. Exerc. Sci. 31, 194–203 (2019).
Singh, T. P., Rhodes, J. & Gauvreau, K. Determinants of heart rate recovery following exercise in children. Med. Sci. Sports Exerc. 40, 601–605 (2008).
Lintu, N. et al. Cardiovascular fitness and haemodynamic responses to maximal cycle ergometer exercise test in children 6-8 years of age. J. Sports Sci. 32, 652–659 (2014).
Guilkey, J. P., Dykstra, B., Erichsen, J. & Mahon, A. D. Heart rate response and variability following maximal exercise in overweight children. Pediatr. Exerc. Sci. 29, 341–349 (2017).
Dimkpa, U. Post-exercise heart rate recovery: an index of cardiovascular fitness. J. Exerc. Physiol. 12, 10–22 (2009).
Fernando, R. J., Ravichandran, K. & Vaz, M. Aerobic fitness, heart rate recovery and heart rate recovery time in indian school children. Indian J. Physiol. Pharmacol. 59, 407–413 (2015).
Jarrin, D. C. et al. Short-term heart rate variability in a population-based sample of 10-year-old children. Pediatr. Cardiol. 36, 41–48 (2015).
Cysarz, D. et al. Unexpected course of nonlinear cardiac interbeat interval dynamics during childhood and adolescence. PLoS ONE 6, e19400 (2011).
Gasior, J. S. et al. Interaction between heart rate variability and heart rate in pediatric population. Front. Physiol. 18, 385 (2015).
Eyre, E. L. J., Duncan, M. J., Birch, S. L. & Fisher, J. P. The influence of age and weight status on cardiac autonomic control in healthy children: a review. Auton. Neurosci. Basic Clin. 186, 8–21 (2014).
Leppänen, M. H. et al. Associations of cardiometabolic risk factors with heart rate variability in 6- to 8-year-old children: the PANIC Study. Pediatr. Diabetes 21, 251–258 (2020).
Gamelin, F. X. et al. Effect of high intensity intermittent training on heart rate variability in prepubescent children. Eur. J. Appl. Physiol. 105, 731–738 (2009).
Da Silva, C. C., Pereira, L. M., Cardoso, J. R., Moore, J. P. & Nakamura, F. Y. The effect of physical training on heart rate variability in healthy children: a systematic review with meta-analysis. Pediatr. Exerc. Sci. 26, 147–158 (2014).
Pereira, L. A. et al. Relationship between resting heart rate variability and intermittent endurance performance in novice soccer players. Res. Q. Exerc. Sport 90, 355–361 (2019).
Acknowledgements
This project would not have been possible without the participation of the numerous schools of Andalusia, to which we are very grateful. We also want to have a special mention and thank you to the parents and teachers of the children who have been involved in this study. We deeply appreciate their trust and support of this project.
Funding
This study does not have any external funding. This research received no external funding.
Author information
Authors and Affiliations
Contributions
P.A.L.-R., J.A.-V. and J.A.P.-M. designed the research; J.A.-V., J.S.-S., M.M.-R. and P.J.C.-G. conducted the research; P.J.C.-G, J.A.-V., M.M.-R. and J.S.-S. provided essential reagents or provided essential materials; P.A.L.-R., E.S.-C. and J.A.-V. analysed data or performed statistical analysis; P.A.L.-R., P.J.C.-G. and J.A.-V. wrote the paper; P.A.L-R., J.A.-V. and J.J.S.-S. had primary responsibility for the final content. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Parents voluntarily signed an informed consent for the participation of their children in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Latorre-Román, P.A., Floody, P.D., Martínez-Redondo, M. et al. Comprehensive cardiac evaluation to maximal exercise in a contemporary population of prepubertal children. Pediatr Res 92, 526–535 (2022). https://doi.org/10.1038/s41390-021-01809-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01809-8
This article is cited by
-
Influence of physical fitness and weight status on autonomic cardiac modulation in children
Pediatric Research (2023)