Abstract
Background
Anemia is associated with decreased tissue oxygenation in preterm infants and may contribute to developing necrotizing enterocolitis (NEC). We aimed to investigate whether hemoglobin level is associated with intestinal injury, by comparing anemic infants 10 days prior to red blood cell (RBC) transfusion with non-anemic controls.
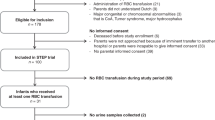
Methods
A nested case–control study in which we matched anemic preterms (gestational age (GA) < 32 weeks) with non-anemic controls (1:1), based on GA, birth weight (BW), and postnatal age. We measured urinary intestinal fatty acid-binding protein, I-FABP, marker for intestinal injury, twice weekly. Simultaneously, we assessed splanchnic oxygen saturation (rsSO2) and rsSO2 variability.
Results
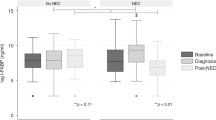
Thirty-six cases and 36 controls were included (median GA 27.6 weeks, BW 1020 grams). Median I-FABP level was higher in cases from 6 days to 24-h before transfusion (median ranging: 4749–8064 pg/ml versus 2194–3751 pg/ml). RsSO2 and rsSO2 variability were lower in cases than controls shortly before transfusion. Hemoglobin levels correlated negatively with rsSO2 and rsSO2 variability in cases, and negatively with I-FABP in cases and controls together.
Conclusions
Urinary I-FABP levels were higher in anemic infants before RBC transfusion than in non-anemic matched controls, suggesting intestinal injury associated with anemia. This may predispose to NEC in some anemic preterm infants.
Impact
-
Anemia is a common comorbidity in preterm infants and may lead to impaired splanchnic oxygen saturation and intestinal tissue hypoxia, a proposed mechanism for NEC.
-
Lower hemoglobin level is associated with higher urinary I-FABP levels, a marker for intestinal injury, both in anemic preterm infants and in cases and controls together.
-
Lower splanchnic oxygen saturation and reduction of its variability are associated with higher urinary I-FABP levels in anemic preterm infants before their first RBC transfusion.
-
These results support the hypothesis that anemia in very preterm infants results in intestinal cell injury, which may precede NEC development in some.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Aher, S., Malwatkar, K. & Kadam, S. Neonatal anemia. Semin. Fetal Neonatal Med. 13, 239–247 (2008).
Colombatti, R., Sainati, L. & Trevisanuto, D. Anemia and transfusion in the neonate. Semin. Fetal Neonatal Med. 21, 2–9 (2016).
Blank, J. P. et al. The role of RBC transfusion in the premature infant. Am. J. Dis. Child. 138, 831–833 (1984).
Van Hoften, J. C. R., Verhagen, E. A., Keating, P., ter Horst, H. J. & Bos, A. F. Cerebral tissue oxygen saturation and extraction in preterm infants before and after blood transfusion. Arch. Dis. Child. Fetal Neonatal Ed. 95, F352–F358 (2010).
Keir, A. K. et al. Temporal changes in blood product usage in preterm neonates born at less than 30 weeks’ gestation in Canada. Transfusion 55, 1340–1346 (2015).
Singh, R. et al. Association of necrotizing enterocolitis with anemia and packed red blood cell transfusions in preterm infants. J. Perinatol. 31, 176–182 (2011).
Patel, R. M. et al. Association of red blood cell transfusions, anemia, and necrotizing enterocolitis in very low-birth-weight infants. JAMA 315, 889–897 (2016).
Ozcan, B., Aydemir, O., Isik, D. U., Bas, A. Y. & Demirel, N. Severe anemia is associated with intestinal injury in preterm neonates. Am. J. Perinatol. 37, 603–606 (2020).
Arthur, C. M. et al. Anemia induces gut inflammation and injury in an animal model of preterm infants. Transfusion 59, 1233–1245 (2019).
MohanKumar, K. et al. Severe neonatal anemia increases intestinal permeability by disrupting epithelial adherens junctions. Am. J. Physiol. Gastrointest. Liver Physiol. 318, G705–G716 (2020).
Christensen, R. D. et al. Is “transfusion-associated necrotizing enterocolitis” an authentic pathogenetic entity? Transfusion 50, 1106–1112 (2010).
Josephson, C. D. et al. Do red cell transfusions increase the risk of necrotizing enterocolitis in premature infants? J. Pediatr. 157, 972–978 (2010).
Paul, D. A. et al. Increased odds of necrotizing enterocolitis after transfusion of red blood cells in premature infants. Pediatrics 127, 635–641 (2011).
Blau, J. et al. Transfusion-related acute gut injury: necrotizing enterocolitis in very low birth weight neonates after packed red blood cell transfusion. J. Pediatr. 158, 403–409 (2011).
Mohamed, A. & Shah, P. S. Transfusion associated necrotizing enterocolitis: a meta-analysis of observational data. Pediatrics 129, 529–540 (2012).
La Gamma, E. F. & Blau, J. Transfusion-related acute gut injury: feeding, flora, flow, and barrier defense. Semin. Perinatol. 36, 294–305 (2012).
Stritzke, A. I., Smyth, J., Synnes, A., Lee, S. K. & Shah, P. S. Transfusion-associated necrotizing enterocolitis in neonates. Arch. Dis. Child. Fetal Neonatal Ed. 98, F10–F14 (2013).
Cunningham, K. E., Okolo, F. C., Baker, R., Mollen, K. P. & Good, M. Red blood cell transfusion in premature infants leads to worse necrotizing enterocolitis outcomes. J. Surg. Res. 213, 158–165 (2017).
Kirpalani, H. & Zupancic, J. A. Do transfusions cause necrotizing enterocolitis? The complementary role of randomized trials and observational studies. Semin. Perinatol. 36, 269–276 (2012).
Wallenstein, M. B. et al. Red blood cell transfusion is not associated with necrotizing enterocolitis: a review of consecutive transfusions in a tertiary neonatal intensive care unit. J. Pediatr. 165, 678–682 (2014).
Sharma, R. et al. Packed red blood cell transfusion is not associated with increased risk of necrotizing enterocolitis in premature infants. J. Perinatol. 34, 858–862 (2014).
Hyung, N. et al. The relationship of red blood cell transfusion to intestinal mucosal injury in premature infants. J. Pediatr. Surg. 52, 1152–1155 (2017).
Le, V. T., Klebanoff, M. A., Talavera, M. M. & Slaughter, J. L. Transient effects of transfusion and feeding advances (volumetric and caloric) on necrotizing enterocolitis development: a case-crossover study. PLoS ONE 12, e0179724 (2017).
Hay, S., Zupancic, J. A. F., Flannery, D. D., Kirpalani, H. & Dukhovny, D. Should we believe in transfusion-associated enterocolitis? Applying a GRADE to the literature. Semin. Perinatol. 41, 80–91 (2017).
AlFaleh, K. et al. Association of packed red blood cell transfusion and necrotizing enterocolitis in very low birth weight infants. J. Neonatal Perinat. Med. 7, 193–198 (2014).
Sood, B. G., Rambhatla, A., Thomas, R. & Chen, X. Decreased hazard of necrotizing enterocolitis in preterm neonates receiving red cell transfusions. J. Matern. Fetal Neonatal Med. 29, 737–744 (2016).
Mintzer, J. P. & Moore, J. E. Regional tissue oxygenation monitoring in the neonatal intensive care unit: evidence for clinical strategies and future directions. Pediatr. Res. 86, 296–304 (2019).
Schat, T. E. et al. The relation between splanchnic ischaemia and intestinal damage in necrotizing enterocolitis. Arch. Dis. Child. Fetal Neonatal Ed. 101, F533–F539 (2016).
Schurink, M. et al. Intestinal fatty acid-binding protein in neonates with imminent necrotizing enterocolitis. Neonatology 106, 49–54 (2014).
Schurink, M. et al. Intestinal fatty acid-binding protein as a diagnostic marker for complicated and uncomplicated necrotizing enterocolitis: a prospective cohort study. PLoS ONE 10, e0121336 (2015).
Von Lindern, J. S., Brand, A. & Lopriore, E. Revision of the guideline ‘Blood transfusion’: for the newborn. Ned. Tijdschr. Geneeskd. 156, A4795 (2012).
Naulaers, G. et al. Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology 92, 120–126 (2007).
Mintzer, J. P., Parvez, B., Chelala, M., Alpan, G. & LaGamma, E. F. Quiescent variability of cerebral, renal, and splanchnic regional tissue oxygenation in very low birth weight neonates. J. Neonatal Perinat. Med. 7, 199–206 (2014).
Diez, S. et al. Clinical characteristics of necrotizing enterocolitis in preterm patients with and without persistent ductus arteriosus and in patients with congenital heart disease. Front. Pediatr. 8, 257 (2020).
Cavalcanti, L. S. et al. Serial Doppler velocimetry of mesenteric and portal flow in very-low-birth-weight preterm neonates with and without patent ductus arteriosus. Pediatr. Radiol. 50, 1107–1114 (2020).
Reisinger, K. W. et al. Intestinal fatty acid-binding protein: a possible marker for gut maturation. Pediatr. Res. 76, 261–268 (2014).
Elnady, H. G. et al. Prediction of gut wall integrity loss in viral gastroenteritis by non-invasive marker. Open Access Maced. J. Med. Sci. 3, 37–45 (2015).
Kuik, S. J. et al. Predicting intestinal recovery after necrotizing enterocolitis in preterm infants. Pediatr. Res. 87, 903–909 (2020).
Heida, F. H. et al. A necrotizing enterocolitis-associated gut microbiotia is present in the meconium: results of a prospective study. Clin. Infect. Dis. 62, 863–870 (2016).
Schat, T. E. et al. Early cerebral and intestinal oxygenation in the risk assessment of necrotizing enterocolitis in preterm infants. Early Hum. Dev. 131, 75–80 (2019).
Martini, S. & Corvaglia, L. Splanchnic NIRS monitoring in neonatal care: rationale, current applications and future perspectives. J. Perinatol. 38, 431–443 (2018).
Koehler, R. C., Traystman, R. J. & Jones, M. D. Jr. Regional blood flow and O2 transport during hypoxic and CO hypoxia in neonatal and adult sheep. Am. J. Physiol. 248, H118–H124 (1985).
El-Dib, M., Narang, S., Lee, E., Massaro, A. N. & Aly, H. Red blood cell transfusion, feeding, and necrotizing enterocolitis in preterm infants. J. Perinatol. 31, 183–187 (2011).
Fairchild, K. D. Predictive monitoring for early detection of sepsis in neonatal ICU patients. Curr. Opin. Pediatr. 25, 172–179 (2013).
Javorka, K. et al. Heart rate variability in newborns. Physiol. Res. 66, S203–S214 (2017).
Cortez, J. et al. Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J. Matern. Fetal Neonatal Med. 24, 574–582 (2011).
Schat, T. E. et al. Near-infrared spectroscopy to predict the course of necrotizing enterocolitis. PLoS ONE 11, e0154710 (2016).
Kalteren, W. S. et al. Red blood cell transfusions affect intestinal and cerebral oxygenation differently in preterm infants with and without subsequent necrotizing enterocolitis. Am. J. Perinatol. 35, 1031–1037 (2018).
Van der Heide, M., Hulscher, J. B. F., Bos, A. F. & Kooi, E. M. W. Near-infrared spectroscopy as a diagnostic tool for necrotizing enterocolitis in preterm infants. Pediatr. Res. 90, 148–155 (2021).
Franz, A. R. et al. Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight infants: the ETTNO randomized clinical trial. JAMA 324, 560–570 (2020).
Kirpalani, H. et al. Higher or lower hemoglobin transfusion thresholds for preterm infants. N. Engl. J. Med. 383, 2639–2651 (2020).
Heida, F. H. et al. Intestinal fatty acid-binding protein levels in necrotizing enterocolitis correlate with extent of necrotic bowel: results from a multicenter study. J. Pediatr. Surg. 50, 1115–1118 (2015).
Kokesova, A. et al. The intestinal fatty acid-binding protein as a marker for intestinal damage in gastroschisis. PLoS ONE 14, e0210797 (2019).
Acknowledgements
We greatly acknowledge the patients and their parents for participating in the POCKET-study and/or STEP-trial. Furthermore, we acknowledge the nurses, medical staff, and students of the NICU at the Beatrix Children’s Hospital in Groningen for helping to collect data. We also thank Ms. A.J. Olthuis, Ms. D.H. Baptist, and Ms. H.A. Bouma for their help with patient inclusion and data collection. This study was part of the research program of the Graduate School of Medical Sciences, Research Institute SHARE, University of Groningen.
Funding
Ms. W.S. Kalteren received a grant from the Tekke Huizinga Fonds, Groningen, the Netherlands. Ms. W.S. Kalteren also received financial support from the Junior Scientific Master Class of the University of Groningen. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
W.S.K. conceptualized and designed the study, collected data, carried out and interpreted the analyses, drafted the initial manuscript, and critically reviewed and revised the manuscript for important intellectual content. A.F.B. conceptualized and designed the study, supervised and interpreted the analyses, and critically reviewed and revised the manuscript for important intellectual content. W.v.O. performed laboratory analyses, and critically reviewed, and revised the manuscript for important intellectual content. J.B.F.H. conceptualized and designed the study, and critically reviewed, and revised the manuscript for important intellectual content. E.M.W.K. conceptualized and designed the study, coordinated and supervised data collection, supervised and interpreted the analyses, and critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
All parents or guardians of neonates provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kalteren, W.S., Bos, A.F., van Oeveren, W. et al. Neonatal anemia relates to intestinal injury in preterm infants. Pediatr Res 91, 1452–1458 (2022). https://doi.org/10.1038/s41390-021-01903-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01903-x
This article is cited by
-
A predictive model for prognosis in infants with surgical necrotizing enterocolitis
Italian Journal of Pediatrics (2025)
-
Immune landscape in liver of neonatal mice with phlebotomy-induced anemia
Pediatric Research (2025)
-
Neonatal somatic oxygenation and perfusion assessment using near-infrared spectroscopy
Pediatric Research (2024)
-
Gene expression in the intestine of newborn piglets after hypoxia-reoxygenation
Pediatric Research (2023)
-
Anemia, blood transfusions, and necrotizing enterocolitis in premature infants
Pediatric Research (2022)