Abstract
Background
Our aim was to compare pediatric infective endocarditis (IE) with the clinical profile and outcomes of IE in adults.
Methods
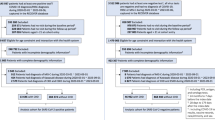
Prospective multicenter registry in 31 Spanish hospitals including all patients with a diagnosis of IE from 2008 to 2020.
Results
A total of 5590 patients were included, 49 were <18 years (0.1%). Congenital heart disease (CHD) was present in 31 children and adolescents (63.2%). Right-sided location was more common in children/adolescents than in adults (46.9% vs. 6.3%, P < 0.001). Pediatric pulmonary IE was more frequent in patients with CHD (48.4%) than in those without (5.6%), P = 0.004. Staphylococcus aureus etiology tended to be more common in pediatric patients (32.7%) than in adults (22.3%), P = 0.082. Heart failure was less common in pediatric patients than in adults, due to the lower rate of heart failure in children/adolescents with CHD (9.6%) with respect to those without CHD (44.4%), P = 0.005. Inhospital mortality was high in both children, and adolescents and adults (16.3% vs. 25.9%; P = 0.126).
Conclusions
Most IE cases in children and adolescents are seen in patients with CHD that have a more common right-sided location and a lower prevalence of heart failure than patients without CHD. IE in children and adolescents without CHD has a more similar profile to IE in adults.
Impact
-
Infective endocarditis (IE) in children and adolescents is often seen in patients with congenital heart disease (CHD).
-
Right-sided location is the most common in patients with CHD and heart failure is less common as a complication compared with patients without CHD.
-
Infective endocarditis (IE) in children/adolescents without CHD has a more similar profile to IE in adults.
-
In children/adolescents without CHD, locations were similar to adults, including a predominance of left-sided IE.
-
Acute heart failure was the most frequent complication, seen mainly in adults, and in children/adolescents without CHD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Baddour, L. M. et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 132, 1435–1486 (2015).
Habib, G. et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur. Heart J. 40, 3222–3232 (2019).
Shah, A. S. V. et al. Incidence, microbiology, and outcomes in patients hospitalized with infective endocarditis. Circulation 141, 2067–2077 (2020).
Baltimore, R. S. et al. Infective endocarditis in childhood: 2015 update. Circulation 132, 1487–1515 (2015).
Zimmerman, M. S. et al. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc. Health 4, 185–200 (2020).
Sakai Bizmark, R., Chang, R.-K. R., Tsugawa, Y., Zangwill, K. M. & Kawachi, I. Impact of AHA’s 2007 guideline change on incidence of infective endocarditis in infants and children. Am. Heart J. 189, 110–119 (2017).
Ferrieri, P. et al. Unique features of infective endocarditis in childhood. Circulation 105, 2115–2126 (2002).
Gupta, S., Sakhuja, A., McGrath, E. & Asmar, B. Trends, microbiology, and outcomes of infective endocarditis in children during 2000-2010 in the United States. Congenit. Heart Dis. 12, 196–201 (2017).
Johnson, J. A., Boyce, T. G., Cetta, F., Steckelberg, J. M. & Johnson, J. N. Infective endocarditis in the pediatric patient: a 60-year single-institution review. Mayo Clin. Proc. 87, 629–635 (2012).
Martin, J. M., Neches, W. H. & Wald, E. R. Infective endocarditis: 35 years of experience at a children’s hospital. Clin. Infect. Dis. 24, 669–675 (1997).
Ahmadi, A. & Daryushi, H. Infective endocarditis in children: a 5 year experience from Al-Zahra Hospital, Isfahan, Iran. Adv. Biomed. Res 3, 228 (2014).
Tseng, W.-C. et al. Changing spectrum of infective endocarditis in children: a 30 years experiences from a tertiary care center in Taiwan. Pediatr. Infect. Dis. J. 33, 467–471 (2014).
Day, M. D., Gauvreau, K., Shulman, S. & Newburger, J. W. Characteristics of children hospitalized with infective endocarditis. Circulation 119, 865–870 (2009).
Habib, G. et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 36, 3075–3128 (2015).
Armiñanzas, C. et al. Role of age and comorbidities in mortality of patients with infective endocarditis. Eur. J. Intern. Med. 64, 63–71 (2019).
Vicent, L. et al. Prognostic implications of a negative echocardiography in patients with infective endocarditis. Eur. J. Intern. Med. 52, 40–48 (2018).
Vicent, L., Saldivar, H. G., Muñoz, P., Bouza, E. & Martínez-Sellés, M. The role of echocardiography as a risk-stratification tool in infective endocarditis. Eur. J. Intern. Med. 53, e23–e24 (2018).
Joffre, J. et al. Epidemiology of infective endocarditis in French intensive care units over the 1997-2014 period - from CUB-Réa Network. Crit. Care 23, 143 (2019).
Cahill, T. J. & Prendergast, B. D. Infective endocarditis. Lancet 387, 882–893 (2016).
Mahony, M. et al. Infective endocarditis in children in Queensland, Australia: epidemiology, clinical features and outcome. Pediatr. Infect. Dis. J. 40, 617–622 (2021).
Luca, A.-C. et al. Difficulties in diagnosis and therapy of infective endocarditis in children and adolescents-cohort study. Healthcare 9, 760 (2021).
Cao, G.-F. & Bi, Q. Pediatric infective endocarditis and stroke: a 13-year single-center review. Pediatr. Neurol. 90, 56–60 (2019).
Lin, Y.-T., Hsieh, K.-S., Chen, Y.-S., Huang, I.-F. & Cheng, M.-F. Infective endocarditis in children without underlying heart disease. J. Microbiol. Immunol. Infect. 46, 121–128 (2013).
Selton-Suty, C. et al. Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin. Infect. Dis. 54, 1230–1239 (2012).
Shamszad, P., Khan, M. S., Rossano, J. W. & Fraser, C. D. J. Early surgical therapy of infective endocarditis in children: a 15-year experience. J. Thorac. Cardiovasc. Surg. 146, 506–511 (2013).
Morpeth, S. et al. Non-HACEK gram-negative bacillus endocarditis. Ann. Intern. Med. 147, 829–835 (2007).
Diekema, D. J. et al. Epidemiology and outcome of nosocomial and community-onset bloodstream infection. J. Clin. Microbiol. 41, 3655–3660 (2003).
Faraji, R. et al. The diagnosis of microorganism involved in infective endocarditis (IE) by polymerase chain reaction (PCR) and real-time PCR: a systematic review. Kaohsiung J. Med. Sci. 34, 71–78 (2018).
Sun, L.-C. et al. Risk factors for infective endocarditis in children with congenital heart diseases—a nationwide population-based case control study. Int. J. Cardiol. 248, 126–130 (2017).
Prieto-Arévalo, R. et al. Pulmonary infective endocarditis. J. Am. Coll. Cardiol. 73, 2782–2784 (2019).
Egbe, A. C., Vallabhajosyula, S., Akintoye, E. & Connolly, H. M. Trends and outcomes of infective endocarditis in adults with tetralogy of fallot: a review of the National Inpatient Sample Database. Can. J. Cardiol. 35, 721–726 (2019).
Kelchtermans, J. et al. Clinical characteristics of infective endocarditis in children. Pediatr. Infect. Dis. J. 38, 453–458 (2019).
Esposito, S. et al. Infective endocarditis in children in Italy from 2000 to 2015. Expert Rev. Antiinfect. Ther. 14, 353–358 (2016).
Dixon, G. & Christov, G. Infective endocarditis in children: an update. Curr. Opin. Infect. Dis. 30, 257–267 (2017).
Thom, K. et al. Incidence of infective endocarditis and its thromboembolic complications in a pediatric population over 30years. Int. J. Cardiol. 252, 74–79 (2018).
Shmueli, H. et al. Right‐sided infective endocarditis 2020: challenges and updates in diagnosis and treatment. J. Am. Heart Assoc. 9, e017293 (2020).
Jortveit, J. et al. Endocarditis in children and adolescents with congenital heart defects: a Norwegian nationwide register-based cohort study. Arch. Dis. Child 103, 670–674 (2018).
Tutarel, O. et al. Infective endocarditis in adults with congenital heart disease remains a lethal disease. Heart 104, 161 (2018).
Mylotte, D. et al. Incidence, predictors, and mortality of infective endocarditis in adults with congenital heart disease without prosthetic valves. Am. J. Cardiol. 120, 2278–2283 (2017).
Li, W. & Somerville, J. Infective endocarditis in the grown-up congenital heart (GUCH) population. Eur. Heart J. 19, 166–173 (1998).
Habib, G. et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur. Heart J. 30, 2369–2413 (2009).
Funding
Unrelated to the study, Lourdes Vicent receives research funding from the Instituto de Salud Carlos III, Spain (CM20/00104).
Author information
Authors and Affiliations
Consortia
Contributions
L.V., M.A.G., P.M., M.M.-A., M.V., M.C.F., M.C.-B., A.d.A., M.Á.R.-E., J.M.M., A.J.G.-A., D.d.C.C., E.G.-V., and M.M.-S. contributed to the design and implementation of the research, to the analysis of the results, and to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
All patients provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vicent, L., Goenaga, M.A., Muñoz, P. et al. Infective endocarditis in children and adolescents: a different profile with clinical implications. Pediatr Res 92, 1400–1406 (2022). https://doi.org/10.1038/s41390-022-01959-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-01959-3
This article is cited by
-
The prognostic role of vegetation size in pediatric infective endocarditis: a retrospective study using decision curve and dose-response analysis
BMC Infectious Diseases (2025)
-
Clinical features of intracardiac thrombotic complication in patients with severe Mycoplasma pneumoniae pneumonia
Italian Journal of Pediatrics (2025)
-
Right-sided infective endocarditis or thrombus? Report of two cases diagnosed by transthoracic echocardiography
Journal of Cardiothoracic Surgery (2024)
-
Infective Endocarditis at a Referral Children’s Hospital During 19-Year Period: Trends and Outcomes
Pediatric Cardiology (2024)
-
Global, regional, and national burden of cardiovascular diseases in youths and young adults aged 15–39 years in 204 countries/territories, 1990–2019: a systematic analysis of Global Burden of Disease Study 2019
BMC Medicine (2023)