Abstract
Background
To develop a model for prediction of severe intracranial hemorrhage (ICH) or death based on variables from the first 12 h of age and to compare mortality and morbidities with and without exposure to early indomethacin.
Methods
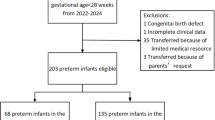
This retrospective cohort study included extreme preterm (220/7−266/7 weeks) infants born at National Institute of Child Health and Human Development Neonatal Research Network sites. Primary outcome was a composite of severe ICH and/or death.
Results
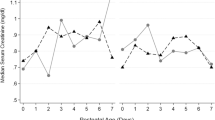
Of 4624 infants, 1827 received early indomethacin. Lower gestation, lack of antenatal steroids exposure, lower 1-min Apgar, male sex, and receipt of epinephrine were associated with severe ICH or death. Early indomethacin was associated with a lower risk of patent ductus arteriosus, bronchopulmonary dysplasia, and higher risk of spontaneous intestinal perforation.
Conclusions
A model for early prediction of severe ICH/death was developed and validated. Early indomethacin was associated with a lower risk of patent ductus arteriosus and bronchopulmonary dysplasia and a higher risk of spontaneous intestinal perforation.
Clinical trial registration
Not applicable.
Impact
-
Modern data on severe ICH and neonatal morbidities in relation to prophylactic indomethacin are scarce in the published literature.
-
Prophylactic indomethacin was associated with a lower risk of patent ductus arteriosus and bronchopulmonary dysplasia and a higher risk of intestinal perforation.
-
A risk estimator for severe intracranial hemorrhage/death was developed in a large cohort of extremely preterm infants.
-
The risk estimator developed based on a large cohort of patients provides an estimate of severe intracranial bleeding for an individual infant.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Sherlock, R. L., Anderson, P. J. & Doyle, L. W. Neurodevelopmental sequelae of intraventricular haemorrhage at 8 years of age in a regional cohort of ELBW/very preterm infants. Early Hum. Dev. 81, 909–916 (2005).
Luu, T. M. et al. Lasting effects of preterm birth and neonatal brain hemorrhage at 12 years of age. Pediatrics 123, 1037–1044 (2009).
Shankaran, S. et al. Maternal race, demography, and health care disparities impact risk for intraventricular hemorrhage in preterm neonates. J. Pediatr. 164, 1005–1011 e1003 (2014).
Ment, L. R. et al. Gene-environment interactions in severe intraventricular hemorrhage of preterm neonates. Pediatr. Res. 75, 241–250 (2014).
Salhab, W. A., Hynan, L. S. & Perlman, J. M. Partial or complete antenatal steroids treatment and neonatal outcome in extremely low birth weight infants < or =1000 g: is there a dose-dependent effect? J. Perinatol. 23, 668–672 (2003).
Luque, M. J. et al. A risk prediction model for severe intraventricular hemorrhage in very low birth weight infants and the effect of prophylactic indomethacin. J. Perinatol. 34, 43–48 (2014).
Ancel, P. Y. et al. Are maternal hypertension and small-for-gestational age risk factors for severe intraventricular hemorrhage and cystic periventricular leukomalacia? Results of the EPIPAGE cohort study. Am. J. Obstet. Gynecol. 193, 178–184 (2005).
Kaiser, J. R., Gauss, C. H., Pont, M. M. & Williams, D. K. Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J. Perinatol. 26, 279–285 (2006).
Linder, N. et al. Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case-control study. Pediatrics 111, e590–e595 (2003).
Heuchan, A. M., Evans, N., Henderson Smart, D. J. & Simpson, J. M. Perinatal risk factors for major intraventricular haemorrhage in the Australian and New Zealand Neonatal Network, 1995-97. Arch. Dis. Child. Fetal Neonatal Ed. 86, F86–F90 (2002).
Ryckman, K. K., Dagle, J. M., Kelsey, K., Momany, A. M. & Murray, J. C. Replication of genetic associations in the inflammation, complement, and coagulation pathways with intraventricular hemorrhage in LBW preterm neonates. Pediatr. Res. 70, 90–95 (2011).
Ment, L. R. et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics 93, 543–550 (1994).
Schmidt, B. et al. Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. N. Engl. J. Med. 344, 1966–1972 (2001).
Fowlie, P. W., Davis, P. G. & McGuire, W. Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants. Cochrane Database Syst. Rev. 2010, CD000174 (2010).
Ment, L. R. et al. Outcome of children in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics 105, 485–491 (2000).
Ment, L. R. et al. Neurodevelopmental outcome at 36 months’ corrected age of preterm infants in the Multicenter Indomethacin Intraventricular Hemorrhage Prevention Trial. Pediatrics 98, 714–718 (1996). 4 Pt 1.
Little, D. C. et al. Patent ductus arteriosus in micropreemies and full-term infants: the relative merits of surgical ligation versus indomethacin treatment. J. Pediatr. Surg. 38, 492–496 (2003).
El-Mashad, A. E., El-Mahdy, H., El Amrousy, D. & Elgendy, M. Comparative study of the efficacy and safety of paracetamol, ibuprofen, and indomethacin in closure of patent ductus arteriosus in preterm neonates. Eur. J. Pediatr. 176, 233–240 (2017).
Clyman, R. I., Saha, S., Jobe, A. & Oh, W. Indomethacin prophylaxis for preterm infants: the impact of 2 multicentered randomized controlled trials on clinical practice. J. Pediatr. 150, 46–50 e42 (2007).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Kadri, H., Mawla, A. A. & Kazah, J. The incidence, timing, and predisposing factors of germinal matrix and intraventricular hemorrhage (GMH/IVH) in preterm neonates. Childs Nerv. Syst. 22, 1086–1090 (2006).
Ment, L. R. et al. Intraventricular hemorrhage in the preterm neonate: timing and cerebral blood flow changes. J. Pediatr. 104, 419–425 (1984).
Hosmer, D. W. & Lameshow, S. Applied Logistic Regression. (Wiley, New York, 2013).
Singh, R. et al. A predictive model for SIVH risk in preterm infants and targeted indomethacin therapy for prevention. Sci. Rep. 3, 2539 (2013).
Chawla, S. et al. Outcomes of extremely low birth weight infants with varying doses and intervals of antenatal steroid exposure. J. Perinat. Med. 38, 419–423 (2010).
Chawla, S. et al. Association of neurodevelopmental outcomes and neonatal morbidities of extremely premature infants with differential exposure to antenatal steroids. JAMA Pediatr. 170, 1164–1172 (2016).
Schmidt, B. et al. Indomethacin prophylaxis, patent ductus arteriosus, and the risk of bronchopulmonary dysplasia: further analyses from the Trial of Indomethacin Prophylaxis in Preterms (TIPP). J. Pediatr. 148, 730–734 (2006).
Jensen, E. A. et al. Association between use of prophylactic indomethacin and the risk for bronchopulmonary dysplasia in extremely preterm infants. J. Pediatr. 186, 34–40 e32 (2017).
Nelin, T. D. et al. Outcomes following indomethacin prophylaxis in extremely preterm infants in an all-referral NICU. J. Perinatol. 37, 932–937 (2017).
Stavel, M. et al. Effect of prophylactic indomethacin administration and early feeding on spontaneous intestinal perforation in extremely low-birth-weight infants. J. Perinatol. 37, 188–193 (2017).
Alexander, G. R., Himes, J. H., Kaufman, R. B., Mor, J. & Kogan, M. A United States national reference for fetal growth. Obstet Gynecol. 87 163–168 (1996).
Walsh, M. C. et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 114, 1305–1311 (2004).
Funding
This study is supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA.
Author information
Authors and Affiliations
Consortia
Contributions
S.C.: Developed the protocol, created data collection form, reviewed analysis and drafted first version of the manuscript. G.N.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. A.R.L.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. D.C.: Reviewed the protocol, conducted the data analysis, and revised the manuscript critically. E.F.B.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. N.A.; Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. W.A.C.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. M.G.: Reviewed the protocol, conducted the data analysis, and revised the manuscript critically. A.D.: Reviewed the protocol, supervised the analysis, and revised the manuscript critically. J.L.T.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. H.H.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis, and revised the manuscript critically. S.S.: Contributed to the conception and design, reviewed the protocol, contributed to the analysis and revised the manuscript critically. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The Generic Database (GDB) data collection was approved by the institutional review board at each site, with waiver of consent granted at all except 3 sites, which required written or oral parental consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of members and their affiliations appears in the Supplementary Information.
Supplementary information
Rights and permissions
About this article
Cite this article
Chawla, S., Natarajan, G., Laptook, A.R. et al. Model for severe intracranial hemorrhage and role of early indomethacin in extreme preterm infants. Pediatr Res 92, 1648–1656 (2022). https://doi.org/10.1038/s41390-022-02012-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02012-z
This article is cited by
-
A FAR-Out approach for evaluating the impact of clinical practice changes on severe intracranial hemorrhage in preterm infants
Journal of Perinatology (2026)
-
Prophylactic indomethacin and the risk of serious pulmonary hemorrhages in preterm infants less than 28 weeks’ gestation
Journal of Perinatology (2024)
-
Prophylactic indomethacin, antenatal betamethasone, and the risk of intestinal perforation in infants <28 weeks’ gestation
Journal of Perinatology (2023)
-
A simple scoring system for prediction of IVH in very-low-birth-weight infants
Pediatric Research (2023)