Abstract
Background
Elevated body mass index (BMI) has been associated with cardiac changes, such as higher epicardial adipose tissue (EAT) thickness. This fat has been identified as a predictive factor of cardiovascular diseases during adulthood. However, few studies have tested the association of multiple cardiovascular risk factors (high weight or blood pressure) with EAT in adolescents and children. Therefore, the main objective of this current research was to determine the impact of BMI, overweight, obesity, and blood pressure on EAT thickness in children.
Methods
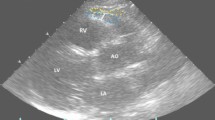
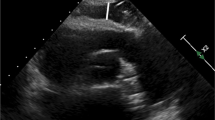
A descriptive cross-sectional study focused on elementary and high school students aged 6–16 years was carried out by utilizing diverse measurements and instruments, such as echocardiography.
Results
EAT thickness (N = 228) was linked to sex (more predominant in boys 2.3 ± 0.6; p = 0.044), obesity (2.3 ± 0.6; p < 0.001), and hypertension (2.6 ± 0.6; p = 0.036). The logistic regression indicated that age, sex, and BMI seemed to be more relevant factors in EAT thickness in children (adjusted R square = 0.22; p < 0.001).
Conclusions
This paper examined the associations of sex, age, and cardiovascular risk factors (arthrometric measures and blood pressure) with EAT thickness, indicating that it is necessary to assess whether the findings are associated with future events.
Impact
-
Excessive weight gain and blood pressure in the early stages of life have been associated with adipose tissue. This increase in weight and blood pressure has been attributed to alterations in the epicardial adipose tissue linked to anthropometric markers in adults, but no related study has been implemented in Spanish children.
-
This study revealed how higher epicardial adipose tissue is linked to body mass index, other anthropometric parameters, and blood pressure in Spanish children. These measurements are related to high epicardial adipose tissue thickness, which in early stages does not imply pathology but increases the risk of developing cardiovascular diseases.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets analyzed during the current study are not publicly available due to the inclusion of personal details, identification numbers from the health care system, and further data for future research. Still, they are available from the corresponding author on reasonable request
References
Atzendorf, J., Apfelbacher, C., de Matos, E. G., Kraus, L. & Piontek, D. Patterns of multiple lifestyle risk factors and their link to mental health in the German adult population: a cross-sectional study. BMJ Open 8, e022184 (2018).
Hoare, E. et al. Lifestyle behavioural risk factors and emotional functioning among schoolchildren: The Healthy Growth Study. Eur. Psychiatry 61, 79–84 (2019).
Marck, C. H. et al. Health outcomes and adherence to a healthy lifestyle after a multimodal intervention in people with multiple sclerosis: three year follow-up. PLoS ONE 13, e0197759 (2018).
von Katzler, R. et al. Lifestyle behaviour and prevalence of cardiovascular risk factors - a pilot study comparing Kiribati and European seafarers. BMC Public Health 19, 855 (2019).
Sharma, S., Shivpuri, A. & Shivpuri, A. Childhood obesity: review of a growing problem. Int. J. Clin. Pediatr. Dent. 5, 237–241 (2012).
Brambilla, P., Pozzobon, G. & Pietrobelli, A. Physical activity as the main therapeutic tool for metabolic syndrome in childhood. Int. J. Obes. 35, 16–28 (2011).
Iacobellis, G. et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes. Res. 11, 304–310 (2003).
Talman, A. H. et al. Epicardial adipose tissue: far more than a fat depot. Cardiovasc. Diagn. Ther. 4, 416–429 (2014).
Rodicio, M. M. et al. Early cardiac abnormalities in obese children and their relationship with adiposity. Nutrition 46, 83–89 (2018).
López-Bermejo, A., Prats-Puig, A., Osiniri, I., Martínez-Calcerrada, J.-M. & Bassols, J. Perirenal and epicardial fat and their association with carotid intima-media thickness in children. Ann. Pediatr. Endocrinol. Metab. 24, 220–225 (2019).
Chumlea, W. M. C., Schubert, C. M., Towne, B., Siervogel, R. M. & Sun, S. S. Left ventricular mass, abdominal circumference and age: The Fels Longitudinal Study. J. Nutr. Health Aging 13, 821 (2019).
Krishnan, R., Becker, R. J., Beighley, L. M. & López-Candales, A. Impact of body mass index on markers of left ventricular thickness and mass calculation: results of a pilot analysis. Echocardiography 22, 203–210 (2005).
Villasante Fricke, A. C. & Iacobellis, G. Epicardial adipose tissue: clinical biomarker of cardio-metabolic risk. Int. J. Mol. Sci. 20, 5989 (2019).
Christensen, R. H., von Scholten, B. J., Lehrskov, L. L., Rossing, P. & Jørgensen, P. G. Epicardial adipose tissue: an emerging biomarker of cardiovascular complications in type 2 diabetes? Ther. Adv. Endocrinol. Metab. 11, 2042018820928824 (2020).
Bertaso, A. G., Bertol, D., Duncan, B. B. & Foppa, M. Epicardial fat: definition, measurements and systematic review of main outcomes. Arq. Bras. Cardiol. 101, e18–e28 (2013).
Toemen, L. et al. Pericardial adipose tissue, cardiac structures, and cardiovascular risk factors in school-age children. Eur. Heart J. Cardiovasc. Imaging 22, 307–313 (2021).
Patro Golab, B., Voerman, E., van der Lugt, A., Santos, S. & Jaddoe, V. W. V. Subcutaneous fat mass in infancy and abdominal, pericardial and liver fat assessed by magnetic resonance imaging at the age of 10 years. Int. J. Obes. 43, 392–401 (2019).
Cabrera-Rego, J. O. et al. Epicardial fat thickness correlates with carotid intima-media thickness, arterial stiffness, and cardiac geometry in children and adolescents. Pediatr. Cardiol. 35, 450–456 (2014).
Kim, S. J. et al. Correlation between epicardial fat thickness by echocardiography and other parameters in obese adolescents. Korean Circ. J. 42, 471–478 (2012).
Cavalcante, J. L. et al. Association of epicardial fat, hypertension, subclinical coronary artery disease, and metabolic syndrome with left ventricular diastolic dysfunction. Am. J. Cardiol. 110, 1793–1798 (2012).
Sinha, S. K. et al. Epicardial adipose tissue thickness and its association with the presence and severity of coronary artery disease in clinical setting: a cross-sectional observational study. J. Clin. Med. Res. 8, 410–419 (2016).
Markopoulou, P., Papanikolaou, E., Analytis, A., Zoumakis, E. & Siahanidou, T. Preterm birth as a risk factor for metabolic syndrome and cardiovascular disease in adult life: a systematic review and meta-analysis. J. Pediatr. 210, 69.e5–80.e5 (2019).
Shin, J.-H. Is the measurement of epicardial fat in obese adolescents valuable? Korean Circ. J. 42, 447 (2012).
Mazur, A., Ostański, M., Telega, G. & Malecka-Tendera, E. Is epicardial fat tissue a marker of metabolic syndrome in obese children? Atherosclerosis 211, 596–600 (2010).
Ahmed, A. M., Ragab, S. H., Ismail, N. A., Awad, M. A. & Kandil, M. E. Echocardiographic assessment of epicardial adipose tissue in obese children and its relation to clinical parameters of metabolic syndrome. J. Saudi Heart Assoc. 25, 108 (2013).
Srikanthan, K., Feyh, A., Visweshwar, H., Shapiro, J. I. & Sodhi, K. Systematic review of metabolic syndrome biomarkers: a panel for early detection, management, and risk stratification in the West Virginian population. Int. J. Med. Sci. 13, 25–38 (2016).
Reyes, Y. et al. Espesor del tejido adiposo epicárdico en niños y adolescentes con factores de riesgo cardiometabólico. Endocrinol. Nutr. 63, 70–78 (2016).
Norton, K. I. in Kinanthropometry and Exercise Physiology (eds Norton, K. & Eston, R.) 68–137 (Routledge, 2018).
Melo Salor, J. Tabla de valores de IMC para sobrepeso y obesidad infantojuvenil de 5 a 19 años según estándares de la OMS. Source: WHO Growth Reference 5-19 years, 2007, https://www.sspa.juntadeandalucia.es/servicioandaluzdesalud/sites/default/files/sincfiles/wsas-media-mediafile_sasdocumento/2019/TablaRapidaIMC_OMS_PIOBIN.pdf (2007).
Zvonar, M., Štefan, L. & Kasović, M. Percentile curves for body-mass index, waist circumference, waist-to-height ratio and waist-to-height ratio(Exp) in Croatian adolescents. Int. J. Environ. Res. Public Health 16, 1920 (2019).
Lozano-Berges, G. et al. Accurate prediction equation to assess body fat in male and female adolescent football players. Int. J. Sport Nutr. Exerc. Metab. 29, 297–302 (2019).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920 (2016).
Smulyan, H. The computerized ECG: friend and foe. Am. J. Med. 132, 153–160 (2019).
García, G. C. & Secchi, J. D. Test course navette de 20 metros con etapas de un minuto. Una idea original que perdura hace 30 años. Apunts Med. l’Esport 49, 93–103 (2014).
Farajian, P. et al. Very high childhood obesity prevalence and low adherence rates to the Mediterranean diet in Greek children: the GRECO study. Atherosclerosis 217, 525–530 (2011).
Pérez-Ríos, M. et al. Excess weight and abdominal obesity in Galician children and adolescents. Ann. Pediatr. 89, 302–308 (2018).
Serra-Majem, L. et al. Obesidad infantil y juvenil en España. Resultados del Estudio enKid (1998-2000). Med. Clín. 121, 725–732 (2003).
Schröder, H. et al. Prevalence of abdominal obesity in Spanish children and adolescents. Do we need waist circumference measurements in pediatric practice? PLoS ONE 9, e87549 (2014).
Aranceta-Bartrina, J., Gianzo-Citores, M. & Perez-Rodrigo, C. Prevalence of overweight, obesity and abdominal obesity in the spanish population aged 3 to 24 years. The Enpe Study. Rev. Espanola Cardiol. 73, 290–299 (2020).
Serra-Majem, L., Bartrina, J. A., Perez-Rodrigo, C., Ribas-Barba, L. & Delgado-Rubio, A. Prevalence and deteminants of obesity in Spanish children and young people. Br. J. Nutr. 96, S67–S72 (2006).
Garcia, L. M. T., da Silva, K. S., Del Duca, G. F., da Costa, F. F. & Nahas, M. V. Sedentary behaviors, leisure-time physical inactivity, and chronic diseases in Brazilian workers: a cross sectional study. J. Phys. Act. Health 11, 1622–1634 (2014).
Rose, T. et al. A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J. Adolesc. Health 61, 669–677 (2017).
Valerio, G. et al. Childhood obesity classification systems and cardiometabolic risk factors: a comparison of the Italian, World Health Organization and International Obesity Task Force references. Ital. J. Pediatr. 43, 19 (2017).
van Hoek, E., Koopman, L. P., Feskens, E. J. M. & Janse, A. J. Assessment of epicardial adipose tissue in young obese children. Child Adolesc. Obes. 2, 96–107 (2019).
Cho, D. H. et al. Association between epicardial adipose tissue, high-sensitivity C-reactive protein and myocardial dysfunction in middle-aged men with suspected metabolic syndrome. Cardiovasc. Diabetol. 17, 9 (2018).
Güneş, H., Güneş, H. & Temiz, F. The relationship between epicardial adipose tissue and insulin resistance in obese children. Arq. Bras. Cardiol. 114, 675–682 (2020).
Radgoudarzi, M., Pazouki, A., Fahmfam, Z. & Soheilipour, F. Evaluation of changes in cardiac dimensions and functional parameters and their association with anthropometric parameters and laboratory indices in obese adolescents. Med. Sci. 24, 1520–1527 (2020).
Bedir, A., Mehmet, B. & Cevriye, A. Relationship of epicardial adipose tissue thickness with early indicators of atherosclerosis and cardiac functional changes in obese adolescents with metabolic syndrome. J. Clin. Res. Pediatr. Endocrinol. 5, 156–163 (2013).
Acknowledgements
We would like to thank the parents and children who decided to participate in this research.
Funding
This research did not receive any funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, I.M.B.S., F.J.F.P., and M.D.M.R.; methodology, I.M.B.S., F.J.F.P., and M.D.M.R.; validation, I.M.B.S., FJ.F.P., and P.A.-M.; formal analysis, P.A.-M., M.R.O., I.M.B.S., and M.D.M.R.; investigation, I.M.B.S., C.H.A.-D., J.F.C.; resources, I.M.B.S., C.H.A.-D., J.F.C., FJ.F.P., and M.D.M.R.; writing—original draft preparation, P.A.-M., FJ.F.P., and I.M.B.S.; writing—review and editing, P.A.-M., M.R.O., FJ.F.P., and I.M.B.S.; supervision, FJ.F.P. and M.D.M.R. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This research follows the Helsinki Code and Biomedicine Principles and obtained the Approval from Andalusian Ethical Committee, also known as PEIBA, specifically at the Regional Committee at the Reina Sofia’s Hospital number 2353. Informed consent was obtained by the parents or legal guardians, the student himself, and the principal researcher.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Blancas Sánchez, I.M., Aristizábal-Duque, C.H., Fernández Cabeza, J. et al. Role of obesity and blood pressure in epicardial adipose tissue thickness in children. Pediatr Res 92, 1681–1688 (2022). https://doi.org/10.1038/s41390-022-02022-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02022-x