Abstract
Background and aims
The investigation of inflammatory background of hypertension (HTN) concentrates mainly on patients with primary HTN. The aim of the study was to analyze the role of new parameters of inflammation—lymphocyte to monocyte ratio (LMR), neutrophil to lymphocyte ratio (NLR), and platelet to lymphocyte ratio (PLR), in the population of children with primary (pHTN) and secondary renal hypertension (rHTN).
Material and methods
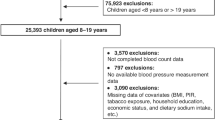
The study group consisted of 70 children with pHTN, 46 patients with rHTN, and 30 age-matched normotensive controls. The retrospective analysis focused on the evaluation of LMR, NLR, and PLR values in relation to blood pressure (BP) parameters from in-office and ambulatory BP monitoring measurements. Twenty-four hours, daytime, and nighttime periods were evaluated. Blood pressure variability (BPV) was defined by standard deviation and coefficient of variation of analyzed values.
Results
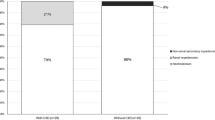
LMR and NLR values in HTN patients differed significantly vs. controls. Dippers with pHTN demonstrated significant correlations between LMR, NLR, PLR, and markers of BPV, in 24 h and daytime diastolic BP and mean arterial pressure. In dippers with rHTN such correlations concerned only LMR.
Conclusions
LMR may become a promising marker of BPV, useful in children with primary and secondary hypertension.
Impact
-
Lymphocyte to monocyte ratio is a novel marker of blood pressure variability, connected to target-organ damage, in children with primary and secondary renal hypertension.
-
Our study analyzes for the first time the connections between blood cell count-driven inflammatory markers (lymphocyte to monocyte, neutrophil to lymphocyte, and platelet to lymphocyte ratios) and parameters of blood pressure variability, and compares those ratios in children with primary and secondary hypertension.
-
The increasing incidence of hypertension among children urges the search for simple methods of assessment of its complications. LMR may be of added value in the analysis of the inflammatory background of hypertension.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Song, P. et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. 173, 1154–1163 (2019).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117, 3171–3180 (2008).
Sarganas, G., Schaffrath, R. A., Niessner, C., Woll, A. & Neuhauser, H. K. Tracking of blood pressure in children and adolescents in Germany in the context of risk factors for hypertension. Int J. Hypertens. 2018, 8429891 (2018).
Theodore, R. F. et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension 66, 1108–1115 (2015).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920 (2016).
Rao, G. Diagnosis, epidemiology, and management of hypertension in children. Pediatrics 138, e20153616 (2016).
Flyn, J. T. et al. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension 63, 1116–1135 (2014).
Wenzel, U. O., Ehmke, H. & Bode, M. Immune mechanisms in arterial hypertension. Recent advances. Cell Tissue Res. 385, 393–404 (2021).
Balta, S. et al. The relation between atherosclerosis and the neutrophil-lymphocyte ratio. Clin. Appl Thromb. Hemost. 22, 405–411 (2016).
Balta, S. & Ozturk, C. The platelet-lymphocyte ratio: a simple, inexpensive and rapid prognostic marker for cardiovascular events. Platelets 26, 680–681 (2015).
Kurtul, A. & Ornek, E. Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology 70, 802–818 (2019).
Zamora, C., Cantó, E. & Vidal, S. The dual role of platelets in the cardiovascular risk of chronic inflammation. Front Immunol. 12, 625181 (2021).
Sunbul, M. et al. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension. Clin. Exp. Hypertens. 36, 217–221 (2014).
Kılıçaslan, B. et al. The relationship between neutrophil to lymphocyte ratio and blood pressure variability in hypertensive and normotensive subjecs. Turk. Kardiyol. Dern. Ars. 43, 18–24 (2015).
Liu, X. et al. Blood neutrophil to lymphocyte ratio as a predictor of hypertension. Am. J. Hypertens. 28, 1339–1346 (2015).
Hou, M. et al. Neutrophil to lymphocyte ratio is increased and associated with left ventricular diastolic function in newly diagnosed essential hypertension children. Front Pediatr. 9, 576005 (2021).
Litwin, M. et al. Inflammatory activation in children with primary hypertension. Pediatr. Nephrol. 25, 1711–1718 (2010).
Skrzypczyk, P. et al. Complete blood count-derived inflammatory markers in adolescents with primary arterial hypertension: a preliminary report. Cent. Eur. J. Immunol. 43, 434–441 (2018).
Hutterer, G. C. et al. Pretreatment lymphocyte-monocyte ratio as a potential prognostic factor in a cohort of patients with upper tract urothelial carcinoma. J. Clin. Pathol. 68, 351–355 (2015).
Balta, S., Demırer, Z., Aparci, M., Yildirim, A. O. & Ozturk, C. The lymphocyte-monocyte ratio in clinical practice. J. Clin. Pathol. 69, 88–89 (2016).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Boubouchairopoulou, N., Ntineri, A., Kollias, A., Destounis, A., & Stergiou, G. S. Blood pressure variability assessed by office, home, and ambulatory measurements: comparison, agreement, and determinants. Hypertens Res. 44, 1617–1624. https://doi.org/10.1038/s41440-021-00736-9 (2021).
Araos, P., Figueroa, S. & Amador, C. A. The role of neutrophils in hypertension. Int J. Mol. Sci. 21, 8536 (2020).
Belen, E., Sungur, A., Sungur, M. A. & Erdoğan, G. Increased neutrophil to lymphocyte ratio in patients with resistant hypertension. J. Clin. Hypertens. (Greenwich) 17, 532–537 (2015).
Karaman, M. et al. The comparative effects of valsartan and amlodipine on vWf levels and N/L ratio in patients with newly diagnosed hypertension. Clin. Exp. Hypertens. 35, 516–522 (2013).
Cetin, N. & Tufan, A. K. Platelet activation and inflammation in hypertensive children with non-dipper and dipper status. Int J. Kidney Dis. 13, 105–112 (2019).
Wenzel, P. Monocytes as immune targets in arterial hypertension. Br. J. Pharmacol. 176, 1966–1977 (2019).
Rothmeier, A. S. et al. Caspase-1-mediated pathway promotes generation of thromboinflammatory microparticles. J. Clin. Invest 125, 1471–1484 (2015).
Gu, L. et al. Prognostic role of lymphocyte to monocyte ratio for patients with cancer: evidence from a systematic review and meta-analysis. Oncotarget 7, 31926–31942 (2016).
Garcia-Rojo, D. et al. Prognostic value of lymphocyte-to-monocyte ratio previously determined to surgery in patients with non-metastatic renal cel carcinoma. Medicine 100, e24152 (2021).
Author information
Authors and Affiliations
Contributions
Conceptualization: K.M., A.B.-G., P.M.; investigation: K.M., A.B.-G., P.M., M.G., S.G.; resources: P.M., M.G., S.G.; formal analysis: K.M., P.M., M.G.; writing—original draft: K.M., A.B.-G., P.M.; writing—review and editing: K.M., D.Z.; visualization: K.M., P.M., M.G.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures were performed in accordance with the 1964 Helsinki Declaration and its further amendments. Retrospective informed consent was obtained from all available subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Musiał, K., Bargenda-Lange, A., Mazurkiewicz, P. et al. Lymphocyte to monocyte ratio and blood pressure variability in childhood hypertension—a pilot study. Pediatr Res 93, 137–142 (2023). https://doi.org/10.1038/s41390-022-02056-1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02056-1
This article is cited by
-
Association between systemic inflammation markers and blood pressure among children and adolescents: National Health and Nutrition Examination Survey
Pediatric Research (2025)
-
Systemic inflammation markers and the prevalence of hypertension: A NHANES cross-sectional study
Hypertension Research (2023)