Abstract
Neonates who present in high output heart failure secondary to vein of Galen aneurysmal malformation can be difficult to manage medically due to the complex physiology that results from the large shunt through the malformation. Though the cardiac function is often normal, right ventricular dilation, severe pulmonary hypertension, and systemic steal can result in inadequate organ perfusion and shock. This report recommends medical management for stabilization of neonates prior to definitive management with endovascular embolization.
Impact
-
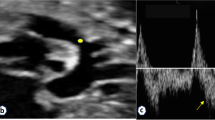
Vein of Galen aneurysmal malformation (VGAM) is a rare intracranial arteriovenous malformation, which can present in the neonatal period with high output heart failure.
-
Heart failure secondary to VGAM is often difficult to manage and is associated with high mortality and morbidity. Despite optimal medical management, many patients require urgent endovascular embolization for stabilization of their heart failure.
-
This report offers discrete recommendations that can be used by clinicians as guidelines for the medical management of heart failure in newborns with VGAM.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Raybaud, C. A., Strother, C. M. & Hald, J. K. Aneurysms of the vein of Galen: embryonic considerations and anatomical features relating to the pathogenesis of the malformation. Neuroradiology 31, 109–128 (1989).
Houser, O. W., Campbell, J. K., Campbell, R. J. & Sundt, T. M. Jr. Arteriovenous malformation affecting the transverse dural venous sinus−an acquired lesion. Mayo Clin. Proc. 54, 651–661 (1979).
Duran, D. et al. Mutations in chromatin modifier and ephrin signaling genes in vein of Galen malformation. Neuron 101, 429.e4–443.e4 (2019).
Revencu, N. et al. Rasa1 mutations and associated phenotypes in 68 families with capillary malformation-arteriovenous malformation. Hum. Mutat. 34, 1632–1641 (2013).
Frawley, G. P., Dargaville, P. A., Mitchell, P. J., Tress, B. M. & Loughnan, P. Clinical course and medical management of neonates with severe cardiac failure related to vein of Galen malformation. Arch. Dis. Child. Fetal Neonatal Ed. 87, F144–F149 (2002).
Cumming, G. R. Circulation in neonates with intracranial arteriovenous fistula and cardiac failure. Am. J. Cardiol. 45, 1019–1024 (1980).
Cordova, E. G. et al. Vein of Galen malformation. Neoreviews 21, e678–e686 (2020).
Lasjaunias, P. L. et al. The management of vein of Galen aneurysmal malformations. Neurosurgery 59, S184–S194 (2006).
Patel, N., Mills, J. F., Cheung, M. M. & Loughnan, P. M. Systemic haemodynamics in infants with vein of Galen malformation: assessment and basis for therapy. J. Perinatol. 27, 460–463 (2007).
Chevret, L. et al. Severe cardiac failure in newborns with vgam. prognosis significance of hemodynamic parameters in neonates presenting with severe heart failure owing to vein of Galen arteriovenous malformation. Intensive Care Med. 28, 1126–1130 (2002).
Dahdah, N. S., Alesseh, H., Dahms, B. & Saker, F. Severe pulmonary hypertensive vascular disease in two newborns with aneurysmal vein of Galen. Pediatr. Cardiol. 22, 538–541 (2001).
Giorgi, L. et al. Management and outcomes of neonatal arteriovenous brain malformations with cardiac failure: a 17 years’ experience in a tertiary referral center. J. Pediatr. 218, 85.e2–91.e2 (2020).
Taffin, H. et al. Long-term outcome of vein of Galen malformation. Dev. Med. Child Neurol. 62, 729–734 (2020).
McElhinney, D. B., Halbach, V. V., Silverman, N. H., Dowd, C. F. & Hanley, F. L. Congenital cardiac anomalies with vein of Galen malformations in infants. Arch. Dis. Child. 78, 548–551 (1998).
Hansen, D. et al. Pediatric knowledge update: approach to the management of vein of Galen aneurysmal malformations in neonates. Surg. Neurol. Int. 7, S317–S321 (2016).
Fullerton, H. J., Aminoff, A. R., Ferriero, D. M., Gupta, N. & Dowd, C. F. Neurodevelopmental outcome after endovascular treatment of vein of Galen malformations. Neurology 61, 1386–1390 (2003).
Paladini, D. et al. Vein of Galen aneurysmal malformation (VGAM) in the fetus: retrospective analysis of perinatal prognostic indicators in a two-center series of 49 cases. Ultrasound Obstet. Gynecol. 50, 192–199 (2017).
Arko, L., Lambrych, M., Montaser, A., Zurakowski, D. & Orbach, D. B. Fetal and neonatal MRI predictors of aggressive early clinical course in vein of Galen malformation. Am. J. Neuroradiol. 41, 1105–1111 (2020).
Saliou, G. et al. Pseudofeeders on fetal magnetic resonance imaging predict outcome in vein of Galen malformations. Ann. Neurol. 81, 278–286 (2017).
Jhaveri, S., Berenstein, A., Srivastava, S., Shigematsu, T. & Geiger, M. K. High output cardiovascular physiology and outcomes in fetal diagnosis of vein of Galen malformation. Pediatr. Cardiol. 42, 1416–1424 (2021).
Kulik, T. J. Pulmonary blood flow and pulmonary hypertension: is the pulmonary circulation flowophobic or flowophilic? Pulm. Circ. 2, 327–339 (2012).
Kumar, S., Sud, N., Fonseca, F. V., Hou, Y. & Black, S. M. Shear stress stimulates nitric oxide signaling in pulmonary arterial endothelial cells via a reduction in catalase activity: role of protein kinase C delta. Am. J. Physiol. Lung Cell. Mol. Physiol. 298, L105–L116 (2010).
Ogasa, T. et al. Flow-mediated release of nitric oxide in isolated, perfused rabbit lungs. J. Appl. Physiol. 91, 363–370 (2001).
van Grondelle, A. et al. Altering hydrodynamic variables influences PGI2 production by isolated lungs and endothelial cells. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 57, 388–395 (1984).
Kluckow, M. & Evans, N. Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch. Dis. Child. Fetal Neonatal Ed. 82, F182–F187 (2000).
Vaksmann, G. et al. Evaluation of vein of Galen arteriovenous malformation in newborns by two dimensional ultrasound, pulsed and colour Doppler method. Eur. J. Pediatr. 148, 510–512 (1989).
Thankavel, P. P. & Ramaciotti, C. Early echocardiographic predictor of heart failure in cerebral arteriovenous malformations. Cardiol. Young 26, 1008–1012 (2016).
Ciricillo, S. F. et al. Serial ultrasonographic evaluation of neonatal vein of Galen malformations to assess the efficacy of interventional neuroradiological procedures. Neurosurgery 27, 544–548 (1990).
Heuchan, A. M. & Bhattacharyha, J. Superior vena cava flow and management of neonates with vein of Galen malformation. Arch. Dis. Child. Fetal Neonatal Ed. 97, F344–F347 (2012).
De Rosa, G. et al. Outcome of neonates with vein of galen malformation presenting with severe heart failure: a case series. Am. J. Perinatol. 36, 169–175 (2019).
Seri, I. Cardiovascular, renal, and endocrine actions of dopamine in neonates and children. J. Pediatr. 126, 333–344 (1995).
Seri, I. & Evans, J. Controversies in the diagnosis and management of hypotension in the newborn infant. Curr. Opin. Pediatr. 13, 116–123 (2001).
Subhedar, N. V. Treatment of hypotension in newborns. Semin. Neonatol. 8, 413–423 (2003).
Joynt, C. & Cheung, P. Y. Treating hypotension in preterm neonates with vasoactive medications. Front. Pediatr. 6, 86 (2018).
Bristow, M. R. et al. Decreased catecholamine sensitivity and beta-adrenergic-receptor density in failing human hearts. N. Engl. J. Med. 307, 205–211 (1982).
Chatterjee, K. & De Marco, T. Role of nonglycosidic inotropic agents: indications, ethics, and limitations. Med. Clin. North Am. 87, 391–418 (2003).
Wehling, M. Specific, nongenomic actions of steroid hormones. Annu. Rev. Physiol. 59, 365–393 (1997).
Noori, S. & Seri, I. Neonatal blood pressure support: the use of inotropes, lusitropes, and other vasopressor agents. Clin. Perinatol. 39, 221–238 (2012).
Barrington, K. J., Finer, N. N. & Chan, W. K. A blind, randomized comparison of the circulatory effects of dopamine and epinephrine infusions in the newborn piglet during normoxia and hypoxia. Crit. Care Med. 23, 740–748 (1995).
Cheung, P. Y. & Barrington, K. J. The effects of dopamine and epinephrine on hemodynamics and oxygen metabolism in hypoxic anesthetized piglets. Crit. Care 5, 158–166 (2001).
Liet, J. M. et al. Dopamine effects on pulmonary artery pressure in hypotensive preterm infants with patent ductus arteriosus. J. Pediatr. 140, 373–375 (2002).
Hunt, R. W., Evans, N., Rieger, I. & Kluckow, M. Low superior vena cava flow and neurodevelopment at 3 years in very preterm infants. J. Pediatr. 145, 588–592 (2004).
Overgaard, C. B. & Dzavik, V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation 118, 1047–1056 (2008).
Shaffner. Roger’s Textbook of Pediatric Intensive Care 5th edn 279–283 and 1175–1177 (Wolters Kluwer, 2016).
Robel-Tillig, E., Knupfer, M., Pulzer, F. & Vogtmann, C. Cardiovascular impact of dobutamine in neonates with myocardial dysfunction. Early Hum. Dev. 83, 307–312 (2007).
Martinez, A. M., Padbury, J. F. & Thio, S. Dobutamine pharmacokinetics and cardiovascular responses in critically ill neonates. Pediatrics 89, 47–51 (1992).
Ferrara, J. J. et al. Effects of dopamine and dobutamine on regional blood flow distribution in the neonatal piglet. Ann. Surg. 221, 531–540 (1995).
Ruffolo, R. R. Jr. The pharmacology of dobutamine. Am. J. Med. Sci. 294, 244–248 (1987).
Klitzner, T. S., Shapir, Y., Ravin, R. & Friedman, W. F. The biphasic effect of amrinone on tension development in newborn mammalian myocardium. Pediatr. Res. 27, 144–147 (1990).
Binah, O., Legato, M. J., Danilo, P. Jr. & Rosen, M. R. Developmental changes in the cardiac effects of amrinone in the dog. Circ. Res. 52, 747–752 (1983).
Artman, M., Kithas, P. A., Wike, J. S. & Strada, S. J. Inotropic responses change during postnatal maturation in rabbit. Am. J. Physiol. 255, H335–H342 (1988).
Akita, T., Joyner, R. W., Lu, C., Kumar, R. & Hartzell, H. C. Developmental changes in modulation of calcium currents of rabbit ventricular cells by phosphodiesterase inhibitors. Circulation 90, 469–478 (1994).
Bianchi, M. O., Cheung, P. Y., Phillipos, E., Aranha-Netto, A. & Joynt, C. The effect of milrinone on splanchnic and cerebral perfusion in infants with congenital heart disease prior to surgery: an observational study. Shock 44, 115–120 (2015).
Hoffman, T. M. et al. Prophylactic Intravenous Use of Milrinone after Cardiac Operation in Pediatrics (Primacorp) Study. Prophylactic intravenous use of milrinone after cardiac operation in pediatrics. Am. Heart J. 143, 15–21 (2002).
Monrad, E. S. et al. Effects of milrinone on coronary hemodynamics and myocardial energetics in patients with congestive heart failure. Circulation 71, 972–979 (1985).
Samiee-Zafarghandy, S. et al. Safety of milrinone use in neonatal intensive care units. Early Hum. Dev. 91, 31–35 (2015).
Giaccone, A. et al. Milrinone pharmacokinetics and pharmacodynamics in neonates with persistent pulmonary hypertension of the newborn. Am. J. Perinatol. 34, 749–758 (2017).
Treschan, T. A. & Peters, J. The vasopressin system: physiology and clinical strategies. Anesthesiology 105, 599–612 (2006).
Cowley, A. W. Jr. & Liard, J. F. Vasopressin and arterial pressure regulation. Special Lecture. Hypertension 11, I25–I32 (1988).
Tamaki, T. et al. Vasodilation induced by vasopressin V2 receptor stimulation in afferent arterioles. Kidney Int. 49, 722–729 (1996).
Walker, B. R., Haynes, J. Jr., Wang, H. L. & Voelkel, N. F. Vasopressin-induced pulmonary vasodilation in rats. Am. J. Physiol. 257, H415–H422 (1989).
Bidegain, M. et al. Vasopressin for refractory hypotension in extremely low birth weight infants. J. Pediatr. 157, 502–504 (2010).
Masarwa, R. et al. Role of vasopressin and terlipressin in refractory shock compared to conventional therapy in the neonatal and pediatric population: a systematic review, meta-analysis, and trial sequential analysis. Crit. Care 21, 1 (2017).
Rios, D. R., Moffett, B. S. & Kaiser, J. R. Trends in pharmacotherapy for neonatal hypotension. J. Pediatr. 165, 697.e1–701.e1 (2014).
Pellicer, A. et al. Cardiovascular support for low birth weight infants and cerebral hemodynamics: a randomized, blinded, clinical trial. Pediatrics 115, 1501–1512 (2005).
Weiss, S. L. et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatr. Crit. Care Med. 21, e52–e106 (2020).
Moffett, B. S. & Price, J. F. National prescribing trends for heart failure medications in children. Congenit. Heart Dis. 10, 78–85 (2015).
Mebazaa, A. et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the survive randomized trial. JAMA 297, 1883–1891 (2007).
Mathew, R. et al. Milrinone as compared with dobutamine in the treatment of cardiogenic shock. N. Engl. J. Med. 385, 516–525 (2021).
Pirracchio, R. et al. The effectiveness of inodilators in reducing short term mortality among patient with severe cardiogenic shock: a propensity-based analysis. PLoS ONE 8, e71659 (2013).
Ashida, Y., Miyahara, H., Sawada, H., Mitani, Y. & Maruyama, K. Anesthetic management of a neonate with vein of Galen aneurysmal malformations and severe pulmonary hypertension. Paediatr. Anaesth. 15, 525–528 (2005).
Karam, O., da Cruz, E. & Rimensberger, P. C. VGAM induced high-flow congestive heart failure responsive to Pge1 infusion. Int. J. Cardiol. 132, e60–e62 (2009).
Fanconi, S., Burger, R., Ghelfi, D., Uehlinger, J. & Arbenz, U. Hemodynamic effects of sodium bicarbonate in critically ill neonates. Intensive Care Med. 19, 65–69 (1993).
McSweeney, N. et al. Management and outcome of vein of Galen malformation. Arch. Dis. Child. 95, 903–909 (2010).
Geibprasert, S., Krings, T., Armstrong, D., Terbrugge, K. G. & Raybaud, C. A. Predicting factors for the follow-up outcome and management decisions in vein of Galen aneurysmal malformations. Childs Nerv. Syst. 26, 35–46 (2010).
Funding
R. Savani holds the William Buchanan Chair in Pediatrics and L.C. is supported by NIH Grant 1R01NS102617. No financial support was received for the development of this review.
Author information
Authors and Affiliations
Contributions
M.J.C. and D.A. contributed to the concept of the paper, wrote the initial and revised drafts of this manuscript, and approved the final manuscript as submitted. R. Sillero, R. Savani, and L.C. contributed to the conceptualization of the paper, reviewed and revised the manuscript, and approved the final manuscript as submitted. P.D. and L.M. reviewed the manuscript, made corrections and edits, and approved the manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
R. Savani is on the Scientific Advisory Council of Mallinckrodt Pharmaceuticals, which had no role in the development of this review. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cory, M.J., Durand, P., Sillero, R. et al. Vein of Galen aneurysmal malformation: rationalizing medical management of neonatal heart failure. Pediatr Res 93, 39–48 (2023). https://doi.org/10.1038/s41390-022-02064-1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02064-1
This article is cited by
-
Subgaleal hemorrhage in neonates: a comprehensive review and summary recommendations
Journal of Perinatology (2025)
-
Vein of Galen aneurysmal malformations: retrospective evaluation of endovascular treatment outcomes
Child's Nervous System (2025)
-
Endovascular treatment of vein of Galen aneurysmal malformation: hospital-based case series in two tertiary centers
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2024)
-
Vein of Galen aneurysmal malformation: does size affect outcome?
Neuroradiology (2024)
-
Vein of galen malformations: for patients and caregivers
Neurosurgical Review (2024)