Abstract
Background
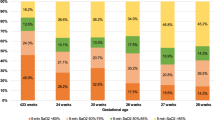
An oxygen saturation (SpO2) histogram classification system has been shown to enable quantification of SpO2 instability into five types, based on histogram distribution and time spent at SpO2 ≤ 80%. We aimed to investigate this classification system as a tool to describe response to doxapram treatment in infants with severe apnea of prematurity.
Methods
This retrospective study included 61 very-low-birth-weight infants who received doxapram. SpO2 histograms were generated over the 24-h before and after doxapram start. Therapy response was defined as a decrease of ≥1 histogram types after therapy start.
Results
The median (IQR) histogram type decreased from 4 (3–4) before to 3 (2–3) after therapy start (p < 0.001). The median (IQR) FiO2 remained constant before (27% [24–35%]) and after (26% [22–35%]) therapy. Thirty-six infants (59%) responded to therapy within 24 h. In 34/36 (94%) of the responders, invasive mechanical ventilation (IMV) was not required during the first 72 h of therapy, compared to 15/25 (60%) of non-responders (p = 0.002). Positive and negative predictive values of the 24-h response for no IMV requirement within 72 h were 0.46 and 0.94, respectively.
Conclusions
Classification of SpO2 histograms provides an objective bedside measure to assess response to doxapram therapy and can serve as a tool to detect changes in oxygenation status around respiratory interventions.
Impact
-
The SpO2 histogram classification system provides a tool for quantifying response to doxapram therapy.
-
The classification system allowed estimation of the probability of invasive mechanical ventilation requirement, already within a few hours of treatment.
-
The SpO2 histogram classification system allows an objective bedside assessment of the oxygenation status of the preterm infant, making it possible to assess the changes in oxygenation status in response to respiratory interventions.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Di Fiore, J. M. et al. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J. Pediatr. 157, 69–73 (2010).
Imanishi, Y. et al. Effect of fluctuation of oxygenation on the development of severe retinopathy of prematurity in extremely preterm infants. J. Perinatol. 40, 515–521 (2020).
Poets, C. F. et al. Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. JAMA 314, 595–603 (2015).
Di Fiore, J. M. et al. Patterns of oxygenation, mortality, and growth status in the surfactant positive pressure and oxygen trial cohort. J. Pediatr. 186, 49.e1–56.e1 (2017).
Pillekamp, F. et al. Factors influencing apnea and bradycardia of prematurity - implications for neurodevelopment. Neonatology 91, 155–161 (2007).
Sivanandan, S. et al. Target oxygen saturation among preterm neonates on supplemental oxygen therapy: a quality improvement study. Indian Pediatr. 55, 793–796 (2018).
Gentle, S., El-Ferzli, G., Winter, L., Salas, A. A. & Philips Iii, J. B. Oxygen saturation histogram monitoring to reduce death or retinopathy of prematurity: a quality improvement initiative. J. Perinatol. 40, 163–169 (2020).
Srivatsa, B., Malcolm, K., Clark, R. H. & Kupke, K. G. Effect of a novel oxygen saturation targeting strategy on mortality, retinopathy of prematurity, and bronchopulmonary dysplasia in neonates born extremely preterm. J. Pediatr. 234, 33.e3–37.e3 (2021).
Gentle, S. J., Ambalavanan, N. & Carlo, W. A. Oxygen saturation histograms predict nasal continuous positive airway pressure-weaning success in preterm infants. Pediatr. Res. 88, 637–641 (2020).
Borenstein-Levin, L., Konikoff, L. & Solimano, A. Clinical quantification of SpO2 instability using a new histogram classification system: a clinical study. Pediatr. Res. 87, 716–720 (2020).
Miller-Barmak, A. et al. Oxygenation instability assessed by oxygen saturation histograms during supine vs prone position in very low birthweight infants receiving noninvasive respiratory support. J. Pediatr. 226, 123–128 (2020).
Flint, R. et al. Retrospective study shows that doxapram therapy avoided the need for endotracheal intubation in most premature neonates. Acta Paediatr. 106, 733–739 (2017).
Poppe, J. A. et al. Use of continuous physiological monitor data to evaluate doxapram therapy in preterm infants. Neonatology 117, 438–445 (2020).
Di Fiore, J. M. et al. Prematurity and postnatal alterations in intermittent hypoxaemia. Arch. Dis. Child. Fetal Neonatal Ed. 106, 557–559 (2021).
Southall, D. P. et al. Undetected episodes of prolonged apnea and severe bradycardia in preterm infants. Pediatrics 72, 541–551 (1983).
Brockmann, P. E. et al. Under-recognition of alarms in a neonatal intensive care unit. Arch. Dis. Child. Fetal Neonatal Ed. 98, F524–F527 (2013).
van Zanten, H. A. et al. The risk for hyperoxaemia after apnoea, bradycardia and hypoxaemia in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 99, F269–F273 (2014).
Goel, N., Chakraborty, M., Watkins, W. J. & Banerjee, S. Predicting extubation outcomes-a model incorporating heart rate characteristics index. J. Pediatr. 195, 53–58 (2018).
Chakraborty, M., Watkins, W. J., Tansey, K., King, W. E. & Banerjee, S. Predicting extubation outcomes using the heart rate characteristics index in preterm infants: a cohort study. Eur. Respir. J. 56, 1901755 (2020).
Shalish, W. et al. Patterns of reintubation in extremely preterm infants: a longitudinal cohort study. Pediatr. Res. 83, 969–975 (2018).
Manley, B. J., Doyle, L. W., Owen, L. S. & Davis, P. G. Extubating extremely preterm infants: predictors of success and outcomes following failure. J. Pediatr. 173, 45–49 (2016).
Chawla, S. et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J. Pediatr. 189, 113.e2–119.e2 (2017).
Poppe, J. A. et al. Precision dosing of doxapram in preterm infants using continuous pharmacodynamic data and model-based pharmacokinetics: an illustrative case series. Front. Pharmacol. 11, 665 (2020).
Poets, C. F. Interventions for apnoea of prematurity: a personal view. Acta Paediatr. 99, 172–177 (2010).
Vliegenthart, R. J. S., van Kaam, A. H., Aarnoudse-Moens, C. S. H., van Wassenaer, A. G. & Onland, W. Duration of mechanical ventilation and neurodevelopment in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 104, F631–F635 (2019).
Poets, C. F. & Lorenz, L. Prevention of bronchopulmonary dysplasia in extremely low gestational age neonates: current evidence. Arch. Dis. Child. Fetal Neonatal Ed. 103, F285–F291 (2018).
Funding
This study was supported by the Sophia Foundation (grant number: S18-27).
Author information
Authors and Affiliations
Contributions
L.B.L. and J.A.P. drafted the first version of this article. The authors substantially contributed to conception and design (L.B.L., J.A.P., S.H.P.S., W.v.W., A.K.), contributed to acquisition of data (J.A.P., I.K.M.R., W.v.W., H.R.T.), and to the analysis and interpretation of data (L.B.L., J.A.P., S.H.P.S., O.H.). All authors revised the article critically for important intellectual content and gave their final approval of the version to be published. The local ethics review board granted a waiver from approval according to the Medical Research Involving Human Subjects Act (WMO) in the Netherlands (MEC-2018-1106).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borenstein-Levin, L., Poppe, J.A., van Weteringen, W. et al. Oxygen saturation histogram classification system to evaluate response to doxapram treatment in preterm infants. Pediatr Res 93, 932–937 (2023). https://doi.org/10.1038/s41390-022-02158-w
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02158-w