Abstract
Background
Preterm birth is associated with higher risks of suboptimal neurodevelopment and cardiometabolic disease later in life. Altered maternal–fetal lipid supply could play a role in such risks. Our hypothesis was that very preterm infants born with very low birth weight (VLBW) have altered lipidome and apolipoprotein profiles, compared with term infants.
Methods
Seven mothers of VLBW infants born at <32 GA and 8 full-term mother–infant dyads were included. Cholesterol and triglycerides in lipoproteins were determined in maternal plasma and in the two blood vessels of the umbilical cord (vein (UV) and artery (UA)) following FPLC isolation. Apolipoprotein concentrations in lipoproteins and plasma lipidomic analysis were performed by LC-MS/MS.
Results
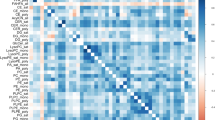
We found higher cholesterol and VLDL-cholesterol in UV and UA and lower apolipoprotein A-I in HDL2 in UV in preterm neonates. Phosphatidylcholine (PC) containing saturated and monounsaturated fatty acids and specific sphingomyelin species were increased in UV and UA, whereas PC containing docosahexaenoic acid (DHA) was reduced in UV of VLBW neonates.
Conclusions
Lower DHA-PC suggests a lower DHA bioavailability and may contribute to the impaired neurodevelopment. Altered HDL-2, VLDL, and sphingomyelin profile reflect an atherogenic risk and increased metabolic risk at adulthood in infants born prematurely.
Impact
-
Lower ApoA-I in HDL2, and increased specific sphingomyelin and phosphatidylcholine containing saturated and monounsaturated fatty acid could explain the accumulation of cholesterol in umbilical vein in VLBW preterm neonates.
-
Decreased phosphatidylcholine containing DHA suggest a reduced DHA availability for brain development in VLBW preterm infants.
-
Characterization of alterations in fetal lipid plasma and lipoprotein profiles may help to explain at least in part the causes of the elevated cardiovascular risk known in people born prematurely and may suggest that a targeted nutritional strategy based on the composition of fatty acids carried by phosphatidylcholine may be promising in infants born very early.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
All data generated or analyzed during this study are included in this published article.
References
Rush, R. W. et al. Contribution of preterm delivery to perinatal mortality. Br. Med. J. 2, 965–968 (1976).
Martin, J. A., Hamilton, B. E., Osterman, M. J. K., Driscoll, A. K. & Drake, P. Births: final data for 2016. Natl Vital Stat. Rep. 67, 1–55 (2018).
Robinson, D. T. & Martin, C. R. Fatty acid requirements for the preterm infant. Semin. Fetal Neonatal Med. 22, 8–14 (2017).
Murray, E. et al. Differential effect of intrauterine growth restriction on childhood neurodevelopment: a systematic review. BJOG 122, 1062–1072 (2015).
Contu, L. & Hawkes, C. A. A review of the impact of maternal obesity on the cognitive function and mental health of the offspring. Int. J. Mol. Sci. 18, 1093 (2017).
Godfrey, K. M. & Barker, D. J. Fetal nutrition and adult disease. Am. J. Clin. Nutr. 71, 1344S–1352S (2000).
Nagano, N. et al. Early postnatal changes of lipoprotein subclass profile in late preterm infants. Clin. Chim. Acta 413, 109–112 (2012).
Ryuta Yonezawa, T. O. et al. Very low-density lipoprotein in the cord blood of preterm neonates. Metabolism 58, 704–707 (2009).
Tea, I. et al. 1H-NMR-based metabolic profiling of maternal and umbilical cord blood indicates altered materno-foetal nutrient exchange in preterm infants. PLoS ONE 7, e29947 (2012).
Pardo, I. M., Geloneze, B., Tambascia, M. A. & Barros-Filho, A. A. Atherogenic lipid profile of Brazilian near-term newborns. Braz. J. Med Biol. Res. 38, 755–760 (2005).
Posod, A. et al. Apolipoprotein profiles in very preterm and term-born preschool children. J. Am. Heart Assoc. 8, e011199 (2019).
Foreman-van Drongelen, M., M., al, M. D., van Houwelingen, A. C., Blanco, C. E. & Hornstra, G. Comparison between the essential fatty acid status of preterm and full-term infants, measured in umbilical vessel walls. Early Hum. Dev. 42, 241–251 (1995).
Arsic, A. et al. Different fatty acid composition of serum phospholipids of small and appropriate for gestational age preterm infants and of milk from their mothers. Hippokratia 16, 230–235 (2012).
Katragadda, T., Mahabala, R. S., Shetty, S. & Baliga, S. Comparison of cord blood lipid profile in preterm small for gestational age and appropriate for gestational age newborns. J. Clin. Diagn. Res. 11, SC05–SC07 (2017).
Kuster, A. et al. Cord blood glutathione depletion in preterm infants: correlation with maternal cysteine depletion. PLoS ONE 6, e27626 (2011).
Barfield, W. D. Public health implications of very preterm birth. Clin. Perinatol. 45, 565–577 (2018).
Chétiveaux, M. et al. The differential apoA-I enrichment of preb1 and aHDL is detectable by gel filtration separation. J. Lipid Res. 43, 1986–1993 (2002).
Croyal, M. et al. Multiplexed peptide analysis for kinetic measurements of major human apolipoproteins by LC/MS/MS. J. Lipid Res. 57, 509–515 (2016).
Blanchard, V. et al. A high-throughput mass spectrometry-based assay for large-scale profiling of circulating human apolipoproteins. J. Lipid Res. 61, 1128–1139 (2020).
Ferchaud-Roucher, V. et al. Plasma lipidome analysis by liquid chromatography-high resolution mass spectrometry and ion mobility of hypertriglyceridemic patients on extended-release nicotinic acid: a pilot study. Cardiovasc. Drugs Ther. 31, 269–279 (2017).
Croyal, M. et al. Fenofibrate decreases plasma ceramide in type 2 diabetes patients:a novel marker of CVD? Diabetes Metab. 44, 143–149 (2018).
Bligh, E. G. & Dyer, W. J. A rapid method of total lipid extraction and purification. Can. J. Biochem. Physiol. 37, 911–917 (1959).
Gallart-Ayala, H. et al. Versatile lipid profiling by liquid chromatography-high resolution mass spectrometry using all ion fragmentation and polarity switching. Preliminary application for serum samples phenotyping related to canine mammary cancer. Anal. Chim. Acta 796, 75–83 (2013).
Storey, J. D. A direct approach to false discovery rates. J. R. Stat. Soc. Ser. B Stat. Methodol. 64, 479–498 (2002).
Ouguerram, K. et al. Apolipoprotein B100 metabolism in autosomal-dominant hypercholesterolemia related to mutations in PCSK9. Arterioscler Thromb. Vasc. Biol. 24, 1448–1453 (2004).
Chiang, A. N. et al. Alterations of serum lipid levels and their biological relevances during and after pregnancy. Life Sci. 56, 2367–2375 (1995).
Diaz, M. et al. Cord blood lipoprotein-cholesterol: relationship birth weight and gestational age of newborns. Metabolism 38, 435–438 (1989).
Pecks, U. et al. Cholesterol acceptor capacity is preserved by different mechanisms in preterm and term fetuses. Biochim. Biophys. Acta 1841, 251–258 (2014).
Napoli, C. et al. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J. Clin. Investig. 100, 2680–2690 (1997).
Johnson, H. J. Jr., Simpson, E. R., Carr, B. R., MacDonald, P. C. & Parker, R. C. Jr. The levels of plasma cholesterol in the human fetus throughout gestation. Pediatr. Res. 16, 682–683 (1982).
Dolphin, P. J., Breckenridge, W. C., Dolphin, M. A. & Tan, M. H. The lipoproteins of human umbilical cord blood apolipoprotein and lipid levels. Atherosclerosis 51, 109–122 (1984).
Lane, D. M. & McConathy, W. J. Changes in the serum lipids and apolipoproteins in the first four weeks of life. Pediatr. Res. 20, 332–337 (1986).
Sreckovic, I. et al. Distinct composition of human fetal HDL attenuates its anti-oxidative capacity. Biochim. Biophys. Acta 1831, 737–746 (2013).
Parker, C. R. Jr. et al. Apolipoprotein A-1 in umbilical cord blood of newborn infants: relation to gestational age and high-density lipoprotein cholesterol. Pediatr. Res. 23, 348–351 (1988).
Hellgren, G., Engstrom, E., Smith, L. E., Lofqvist, C. & Hellstrom, A. Effect of preterm birth on postnatal apolipoprotein and adipocytokine profiles. Neonatology 108, 16–22 (2015).
McQueen, M. J. et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet 372, 224–233 (2008).
Feng, X., Gao, X., Yao, Z. & Xu, Y. Low apoA-I is associated with insulin resistance in patients with impaired glucose tolerance: a cross-sectional study. Lipids Health Dis. 16, 69 (2017).
Hofman, P. L. et al. Premature birth and later insulin resistance. N. Engl. J. Med. 351, 2179–2186 (2004).
Hamosh, M. Lipid metabolism in premature infants. Biol. Neonate 52(Suppl 1), 50–64 (1987).
Del Gaudio, I., Sasset, L., Lorenzo, A. D. & Wadsack, C. Sphingolipid signature of human feto-placental vasculature in preeclampsia. Int. J. Mol. Sci. 21, 1019 (2020).
Bolin, D. J. & Jonas, A. Sphingomyelin inhibits the lecithin-cholesterol acyltransferase reaction with reconstituted high density lipoproteins by decreasing enzyme binding. J. Biol. Chem. 271, 19152–19158 (1996).
Subbaiah, P. V., Horvath, P. & Achar, S. B. Regulation of the activity and fatty acid specificity of lecithin-cholesterol acyltransferase by sphingomyelin and its metabolites, ceramide and ceramide phosphate. Biochemistry 45, 5029–5038 (2006).
Dutta-Roy, A. K. Transport mechanisms for long-chain polyunsaturated fatty acids in the human placenta. Am. J. Clin. Nutr. 71, 315S–322S (2000).
Rogers, L. K., Valentine, C. J. & Keim, S. A. DHA supplementation: current implications in pregnancy and childhood. Pharmacol. Res. 70, 13–19 (2013).
Huppi, P. S. et al. Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann. Neurol. 43, 224–235 (1998).
Volpe, J. J. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 8, 110–124 (2009).
Bernhard, W. et al. Transport of long-chain polyunsaturated fatty acids in preterm infant plasma is dominated by phosphatidylcholine. Eur. J. Nutr. 57, 2105–2112 (2018).
Ferchaud-Roucher, V. et al. A potential role for lysophosphatidylcholine in the delivery of long chain polyunsaturated fatty acids to the fetal circulation. Biochim Biophys. Acta Mol. Cell Biol. Lipids 1864, 394–402 (2019).
Powell, T. L. et al. Sex-specific responses in placental fatty acid oxidation, esterification and transfer capacity to maternal obesity. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 1866, 158861 (2021).
Martinez, M. Tissue levels of polyunsaturated fatty acids during early human development. J. Pediatr. 120, S129–S138 (1992).
Clandinin, M. T., Chappell, J. E., Heim, T., Swyer, P. R. & Chance, G. W. Fatty acid utilization in perinatal de novo synthesis of tissues. Early Hum. Dev. 5, 355–366 (1981).
Nagano, N. et al. Delta-6 desaturase activity during the first year of life in preterm infants. Prostaglandins Leukotrienes Essent. Fat. Acids 115, 8–11 (2016).
Calder, P. C. Polyunsaturated fatty acids, inflammatory processes and inflammatory bowel diseases. Mol. Nutr. Food Res. 52, 885–897 (2008).
Aung, M. T. et al. Prediction and associations of preterm birth and its subtypes with eicosanoid enzymatic pathways and inflammatory markers. Sci. Rep. 9, 17049 (2019).
Henriksson, P., Hamberg, M. & Diczfalusy, U. Formation of 15-HETE as a major hydroxyeicosatetraenoic acid in the atherosclerotic vessel wall. Biochim. Biophys. Acta 834, 272–274 (1985).
Lundqvist, A. et al. The arachidonate 15-lipoxygenase enzyme product 15-HETE is present in heart tissue from patients with ischemic heart disease and enhances clot formation. PLoS ONE 11, e0161629 (2016).
Boquien, C. Y. et al. Breast milk protein content at week 3 after birth and neurodevelopmental outcome in preterm infants fed fortified breast milk. Eur. J. Nutr. 60, 3959–3969 (2021).
Acknowledgements
The authors are grateful to the staff of the Mère-Enfant Clinical Investigation Centre of University Hospital in Nantes for their invaluable help in the management of the blood collection. The authors thank Caroline Mallier for her technical assistance. Lipidomic analysis and apolipoprotein quantification were performed in the Mass Spectrometry Core Facility of CRNH Ouest, Biogenouest Corsaire and SFR F. Bonamy UMS 016 at the University of Nantes.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
A.K. designed the study protocol and provided the human samples. M.C. quantified apolipoprotein in the lipoprotein fractions. D.D. and K.O. supervised the experiments. V.F.-R. conducted the lipidomic analysis, analyzed the results, supervised the experiments, and wrote the manuscript. T.M. supervised the statistical analyses. All authors discussed the results, edited the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
A written informed consent was obtained from every woman included in this clinical pilot study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Küster, A., Croyal, M., Moyon, T. et al. Characterization of lipoproteins and associated lipidome in very preterm infants: a pilot study. Pediatr Res 93, 938–947 (2023). https://doi.org/10.1038/s41390-022-02159-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02159-9