Abstract
Background
Congenital heart diseases are the most prevalent congenital malformations and cause greater morbi-mortality in newborns and infants. The aim of this study was to analyze the social determinants in families with children with the severity of congenital heart disease.
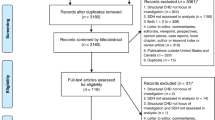
Methods
Analytical cross-sectional study in 140 families of children with congenital heart disease to whom a structured survey was applied addressing topics related to family structure, health, economic conditions, exposure factors, and other social conditions relevant to the study, during 1 year.
Results
In all, 53.7% of the studied population belonged to low socioeconomic levels. No association was found between the severity of the heart disease and the presence of pathological antecedents in the parents. The families resided in urban areas. Also, 28.3% of the mothers had four or fewer prenatal controls during pregnancy. Only 22% of heart diseases were diagnosed during pregnancy. It was found that exposure to cigarette and wood smoke during pregnancy, in addition to low socioeconomic status, was associated with greater severity of heart disease (RACHS-1 and STS-Score), when evaluated by pathophysiological groups (cyanotic/non-cyanotic/single ventricle).
Conclusions
Exposure to cigarette smoke, wood smoke during pregnancy, and low socioeconomic status turned out to be social determinants associated with the severity of heart disease analyzed by pathophysiological groups.
Impact
-
The social component has not been well characterized as a cause of congenital heart disease, especially in countries like ours, where the existence of gaps and social inequities have a high impact.
-
The findings of this study could have an impact on public health to the extent that policies are implemented to reduce exposure to cigarettes, especially during pregnancy.
-
Knowledge of these changes and their measurement in this type of pathology could open the door to the creation of policies aimed at their prevention, focusing on the local risk factors found, which can impact the disease.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. The data can be requested from the following email address dorisquintero@fcv.org, given that internally in the institution where the project was developed, permission must be requested from the research ethics committee for the delivery of data.
References
Agha, M. M., Glazier, R. H., Moineddin, R., Moore, A. M. & Guttmann, A. Socioeconomic status and prevalence of congenital heart defects: does universal access to health care system eliminate the gap? Birth Defects Res. 91, 1011–1018 (2011).
Wong, P. et al. Early life environment and social determinants of cardiac health in children with congenital heart disease. Pediatr. Child Health 23, 92–95 (2018).
Hoffman, J. I. The global burden of congenital heart disease. Cardiovasc. J. Afr. 24, 141 (2013).
Trevisan, P. et al. Cardiopatias congênitas e cromossomopatias detectadas por meio do cariótipo. Rev. Paul. Pediatr. 32, 262–271 (2014).
Van der Linde, D. et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J. Am. Coll. Cardiol. 58, 2241–2247 (2011).
Mejía, L. Los Determinantes Sociales de la Salud: base teórica de la salud pública. Rev. Fac. Nac. Salud Pública 31, 28–36 (2013).
Álvarez, L. S. Los determinantes sociales de la salud: más allá de los factores de riesgo. Rev. Gerenc. Polit. Salud 8, 69–79 (2009).
Yang, J. et al. Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am. J. Epidemiol. 167, 145–154 (2008).
Carmichael, S. L., Ma, C. & Shaw, G. M. Socioeconomic measures, orofacial clefts, and conotruncal heart defects in California. Birth Defects Res. A Clin. Mol. Teratol. 85, 850–857 (2009).
Departamento Administrativo Nacional de Estadística. Frequently Asked Questions document. https://www.dane.gov.co/files/geoestadistica/Preguntas_frecuentes_estratificacion.pdf (2020).
Jenkins, K. J. et al. Consensus-based method for risk adjustment for congenital heart surgery. J. Thorac. Cardiovasc. Surg. 123, 110–118 (2002).
Gaynor, J. W. et al. International Congenital Heart Surgery justment in Congenital Heart Surgery (RACHS-1). Nomenclature Heart Surgery Committees of the Society of Thoracic Surgeons. European Association for Cardio-Thoracic Surgery. Congenital Heart Surgery Nomenclature and Database Project: update and proposed data harvest. Ann. Thorac. Surg. 73, 1016–1018 (2002).
Pace, N. D. et al. Sociodemographic factors and survival of infants with congenital heart defects. Pediatrics 142, e20180302 (2018).
Nembhard, W. N. et al. Racial/ethnic disparities in risk of early childhood mortality among children with congenital heart defects. Pediatrics 127, e1128–e1138 (2011).
Perry, M. F., Mulcahy, H. & DeFranco, E. A. Influence of periconception smoking behavior on birth defect risk. Am. J. Obstet. Gynecol. 220, 588.e1–588.e7 (2019).
Hackshaw, A., Rodeck, C. & Boniface, S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum. Reprod. Update 17, 589–604 (2011).
Baldacci, S. et al. Environmental and individual exposure and the risk of congenital anomalies: a review of recent epidemiological evidence. Epidemol. Prev. 42(3-4 Suppl 1), 1–34 (2018).
Malik, S. et al. Maternal smoking and congenital heart defects. Pediatrics 121, e810–e816 (2008).
Zhang, D. et al. Is maternal smoking during pregnancy associated with an increased risk of congenital heart defects among offspring? A systematic review and meta-analysis of observational studies. J. Matern Neonatal Med. 30, 645–57 (2017).
Karatza, A. A. et al. Periconceptional tobacco smoking and Xisolated congenital heart defects in the neonatal period. Int. J. Cardiol. 148, 295–299 (2011).
Fine, P. M., Cass, G. R. & Simoneit, B. R. T. Chemical characterization of fine particle emissions from fireplace combustion of woods grown in the Northeastern United States. Environ. Sci. Technol. 35, 2665–2675 (2001).
Bruce, N., Pérez-Padilla R. & Albalak, R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull. World Health Organ. 78, 1078–1092 (2000).
Cordier, S. et al. Risk of congenital anomalies in the vicinity of municipal solid waste incinerators. Occup. Environ. Med. 61, 8–15 (2004).
Cordier, S. et al. Maternal residence near municipal waste incinerators and the risk of urinary tract birth defects. Occup. Environ. Med. 67, 493–499 (2010).
Vinceti, M. et al. Adverse pregnancy outcomes in a population exposed to the emissions of a municipal waste incinerator. Sci. Total Environ. 407, 116–21 (2008).
Vinceti, M. et al. Risk of congenital anomalies around a municipal solid waste incinerator: a GIS-based case-control study. Int. J. Health Geogr. 8, 8 (2009).
Corsini, E., Marinovich, M. & Vecchi, R. Ultrafine particles from residential biomass combustion: a review on experimental data and toxicological response. Int. J. Mol. Sci. 20, 4992 (2019).
Soto-Moreno, J. A. & Ballester-Díez, F. Contaminación del aire de interiores en hogares en situación de pobreza extrema en Colombia. Rev. Salud Pública 15, 80–89 (2013).
Sánchez-Triana, E. Ahmed, K. & Awe, Y. Prioridades Ambientales para la Reducción de la Pobreza en Colombia: Un Análisis Ambiental del País para Colombia. Direcciones para el Desarrollo-Medio Ambiente y Desarrollo Sustentable 38610 (Banco Mundial-Mayol Ediciones, 2007).
Acknowledgements
To the parents and caregivers who participated in the study and to the Fundación Cardiovascular de Colombia for their support in this research.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: M.J.F.-M., E.T.-P., J.A.F.-R., D.C.Q.-L., E.M.G.-D. Drafting the article or revising it critically for important intellectual content. C.X.F.-R., J.M.C.-M., M.J.F.-M., D.C.Q.-L., E.M.G.-D. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was reviewed and approved by the Research Ethics Committee (CEI) of the Fundación Cardiovascular de Colombia (Record No. 372). All participating parents or caregivers gave their informed consent. All participating parents or caregivers gave their informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Forero-Manzano, M.J., Triana-Palencia, E., Figueroa-Rueda, J.A. et al. Association of social determinants with the severity of congenital heart disease. Pediatr Res 93, 1391–1398 (2023). https://doi.org/10.1038/s41390-022-02205-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02205-6
This article is cited by
-
Social inequities hurt babies’ hearts: a commentary on Forero-Manzano, MJ, et al.
Pediatric Research (2023)
-
Applying Interventions to Address the Social Determinants of Health and Reduce Health Disparities in Congenital Heart Disease Patients
Current Cardiovascular Risk Reports (2022)