Abstract
Background
Sepsis related acute lung injury (ALI) is established in adults but has not been investigated in premature infants. Herein, we used pulmonary severity score (PSS) trajectories and C-reactive protein (CRP) to examine the relation between sepsis and ALI in premature infants.
Methods
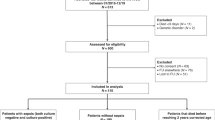
This retrospective study identified 211 sepsis and 123 rule out (RO) events in 443 infants born <31 weeks and <1500 grams. The PSS was calculated prior to, at the time of, and up to 1 week after each event. Initial and peak CRP values were collected for each event.
Results
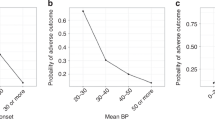
PSS significantly increased at 0 h from baseline (−72h) and remained increased at all subsequent time points (all p < 0.002) in sepsis events. Mean PSS in sepsis episodes were also higher compared to RO events at +24 h, +48 h, +72 h, and +168 h (all p < 0.004). A positive correlation was noted between peak CRP values in sepsis events and PSS at 0 h, +24 h, +48 h, and +72 h.
Conclusions
The temporal PSS trends and correlation with CRP levels observed in sepsis but not in RO events supports the hypothesis that neonatal sepsis is associated with ALI and contributes to the accumulating evidence that neonatal ARDS occurs.
Impact
-
To evaluate pulmonary severity scores and c-reactive protein values over time to establish an association between preterm neonatal sepsis and acute lung injury (ALI).
-
Though sepsis is well established as the most common indirect cause of ALI leading to acute respiratory distress syndrome (ARDS) in adults and pediatrics, this phenomenon remains undefined in neonates.
-
This study validates the proposal by the Neonatal ARDS Project that ARDS also occurs in neonates by demonstrating acute and sustained changes in markers of pulmonary injury temporally related to a diagnosis of neonatal sepsis in preterm infants.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Letouzey, M. et al. Cause of preterm birth and late-onset sepsis in very preterm infants: the EPIPAGE-2 cohort study. Pediatr. Res 90, 584–592 (2021).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD neonatal research network. Pediatrics 110, 285–291 (2002).
Rojas, M. A. et al. Changing trends in the epidemiology and pathogenesis of neonatal chronic lung disease. J. Pediatr. 126, 605–610 (1995).
Lahra, M. M., Beeby, P. J. & Jeffery, H. E. Intrauterine inflammation, neonatal sepsis, and chronic lung disease: a 13-year hospital cohort study. Pediatrics 123, 1314–1319 (2009).
Ohlin, A., Björkman, L., Serenius, F., Schollin, J. & Källén, K. Sepsis as a risk factor for neonatal morbidity in extremely preterm infants. Acta Paediatr. 104, 1070–1076 (2015).
Shah, J., Jefferies, A. L., Yoon, E. W., Lee, S. K. & Shah, P. S., Canadian Neonatal Network. Risk factors and outcomes of late-onset bacterial sepsis in preterm neonates born at <32 weeks’ gestation. Am. J. Perinatol. 32, 675–682 (2015).
Monahan, L. J. Acute respiratory distress syndrome. Curr. Probl. Pediatr. Adolesc. Health Care 43, 278–284 (2013).
Meyer, N. J., Gattinoni, L. & Calfee, C. S. Acute respiratory distress syndrome. Lancet 398, 622–637 (2021).
Matthay, M. A. et al. Acute respiratory distress syndrome. Nat. Rev. Dis. Prim. 5, 1–18 (2019).
Faix, R. G., Viscardi, R. M., DiPietro, M. A. & Nicks, J. J. Adult respiratory distress syndrome in full-term newborns. Pediatrics 83, 971–976, https://www.ncbi.nlm.nih.gov/pubmed/2657626 (1989).
Group TPALICC. Pediatric acute respiratory distress syndrome: consensus recommendations from the pediatric acute lung injury consensus conference. Pediatr. Crit. Care Med. 16, 428–439 (2015).
De Luca, D. et al. The Montreux definition of neonatal ARDS: biological and clinical background behind the description of a new entity. Lancet Respir. Med 5, 657–666 (2017).
Madan, A. et al. A pulmonary score for assessing the severity of neonatal chronic lung disease. Pediatrics 115, e450–e457 (2005).
Linafelter, A. et al. Extended course of prednisolone in infants with severe bronchopulmonary dysplasia. Early Hum. Dev. 136, 1–6 (2019).
Hornik, C. P. et al. Use of the complete blood cell count in late-onset neonatal sepsis. Pediatr. Infect. Dis. J. 31, 803–807 (2012).
Aydemir, C., Aydemir, H., Kokturk, F., Kulah, C. & Mungan, A. G. The cut-off levels of procalcitonin and C-reactive protein and the kinetics of mean platelet volume in preterm neonates with sepsis. BMC Pediatr. 18, 253 (2018).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Kumar, N., Akangire, G., Sullivan, B., Fairchild, K. & Sampath, V. Continuous vital sign analysis for predicting and preventing neonatal diseases in the twenty-first century: big data to the forefront. Pediatr. Res 87, 210–220 (2020).
Benaron, D. A. & Benitz, W. E. Maximizing the stability of oxygen delivered via nasal cannula. Arch. Pediatr. Adolesc. Med 148, 294–300 (1994).
STOP-ROP Multicenter Study Group. Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics 105, 295–310 (2000).
Walsh, M. et al. Oxygen delivery through nasal cannulae to preterm infants: can practice be improved. Pediatrics 116, 857–861 (2005).
Lüdecke, D., Waggoner, P. & Makowski, D. Insight: a unified interface to access information from model objects in R. J. Open Source Softw. 4, 1412 (2019).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. (Academic Press, New York 1988).
Pinheiro, J., Bates, D., DebRoy, S., Sarkar, D., R Core Team. nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1-152. September 2021. https://cran.r-project.org/package=nlme.
R Core Team. R: A language and environment for statistical computing. (R Foundation for Statistical Computing, Vienna, Austria, 2020). https://www.r-project.org/.
Fairchild, K. D. & O’Shea, T. M. Heart rate characteristics: physiomarkers for detection of late-onset neonatal sepsis. Clin. Perinatol. 37, 581–598 (2010).
Sullivan, B. A. & Fairchild, K. D. Predictive monitoring for sepsis and necrotizing enterocolitis to prevent shock. Semin Fetal Neonatal Med 20, 255–261 (2015).
Keim, G., Watson, R. S., Thomas, N. J. & Yehya, N. New morbidity and discharge disposition of pediatric acute respiratory distress syndrome survivors. Crit. Care Med 46, 1731–1738 (2018).
Stoll, B. J. et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 292, 2357–2365 (2004).
Hayes, R. et al. Neonatal sepsis definitions from randomised clinical trials. Pediatr Res. (2021). Online ahead of print. https://doi.org/10.1038/s41390-021-01749-3
INIS Collaborative Group. et al. Treatment of neonatal sepsis with intravenous immune globulin. N. Engl. J. Med 365, 1201–1211 (2011).
ELFIN trial investigators group. Enteral lactoferrin supplementation for very preterm infants: a randomised placebo-controlled trial. Lancet 393, 423–433 (2019).
Menden, H. L. et al. Nicotinamide adenine dinucleotide phosphate oxidase 2 regulates LPS-induced inflammation and alveolar remodeling in the developing lung. Am. J. Respir. Cell Mol. Biol. 55, 767–778 (2016).
Salimi, U., Dummula, K., Tucker, M. H. & Dela Cruz, C. S. Sampath, V. postnatal sepsis and bronchopulmonary dysplasia in premature infants: mechanistic insights into “New BPD. Am. J. Respir. Cell Mol. Biol. 66, 137–145 (2022).
Kawamura, M. & Nishida, H. The usefulness of serial C-reactive protein measurement in managing neonatal infection. Acta Paediatr. 84, 10–13 (1995).
Benitz, W. E., Han, M. Y., Madan, A. & Ramachandra, P. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics 102, E41 (1998).
Pourcyrous, M., Bada, H. S., Korones, S. B., Baselski, V. & Wong, S. P. Significance of serial C-reactive protein responses in neonatal infection and other disorders. Pediatrics 92, 431–435, https://www.ncbi.nlm.nih.gov/pubmed/8361798 (1993).
Author information
Authors and Affiliations
Contributions
M.H.T. conceptualized and designed the study, designed the data collection instruments, collected data, drafted the initial manuscript, and reviewed and revised the manuscript. H.W.Y. carried out data analyses and reviewed and revised the manuscript. D.O. collected data and reviewed and revised the manuscript. N.S. collected data and reviewed and revised the manuscript. N.K. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. V.S. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tucker, M.H., Yeh, HW., Oh, D. et al. Preterm sepsis is associated with acute lung injury as measured by pulmonary severity score. Pediatr Res 93, 1050–1056 (2023). https://doi.org/10.1038/s41390-022-02218-1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02218-1