Abstract
Background
Despite clear benefit of improved outcomes in adults, the impact of infectious diseases (ID) consultation for Staphylococcus aureus bacteremia in children remains understudied.
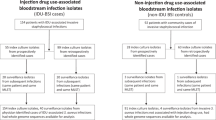
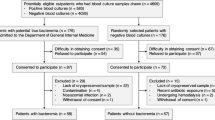
Methods
To assess the impact of pediatric ID consultation on management and outcomes, we conducted a cohort study of children with S. aureus bacteremia at St. Louis Children’s Hospital from 2011 to 2018. We assessed adherence to six established quality-of-care indicators (QCIs). We applied propensity score methodology to examine the impact of ID consultation on risk of treatment failure, a composite of all-cause mortality or hospital readmission within 90 days.
Results
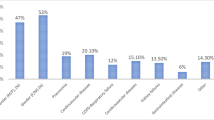
Of 306 patients with S. aureus bacteremia, 193 (63%) received ID consultation. ID consultation was associated with increased adherence to all QCIs, including proof-of-cure blood cultures, indicated laboratory studies, echocardiography, source control, targeted antibiotic therapy, and antibiotic duration. Obtaining proof-of-cure blood cultures and all indicated laboratory studies were associated with improved outcomes. In propensity score-weighted analyses, risk of treatment failure was similar among patients who did and did not receive ID consultation. However, the number of events was small and risk estimates were imprecise.
Conclusions
For children with S. aureus bacteremia, ID consultation improved adherence to QCIs, some of which were associated with improved clinical outcomes.
Impact
-
In children with Staphylococcus aureus bacteremia, consultation by an infectious diseases (ID) physician improved adherence to established quality-of-care indicators (QCIs).
-
The current literature regarding ID consultation in pediatric S. aureus bacteremia is sparse. Three prior international studies demonstrated improved quality of care with ID consultation, though results were disparate regarding clinical outcomes.
-
This article impacts the current literature by strengthening the evidence that ID consultation in children improves adherence to QCIs, and demonstrates that adherence to QCIs improves clinical outcomes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hamdy, R. F., Dona, D., Jacobs, M. B. & Gerber, J. S. Risk factors for complications in children with Staphylococcus aureus bacteremia. J. Pediatrics 208, 214–220.e2 (2019).
Kumarachandran, G., Johnson, J. K., Shirley, D. A., Graffunder, E. & Heil, E. L. Predictors of adverse outcomes in children with Staphylococcus aureus bacteremia. J. Pediatr. Pharm. Ther. 22, 218–226 (2017).
Cardenas-Comfort C, Kaplan SL, Vallejo JG, McNeil JC. Follow-up blood cultures in children with Staphylococcus aureus bacteremia. Pediatrics 146, e20201821 (2020).
Duguid RC, Al Reesi M, Bartlett AW, Palasanthiran P, McMullan BJ. Impact of infectious diseases consultation on management and outcome of Staphylococcus aureus bacteremia in children. J. Pediatric Infect. Dis. Soc. 10, 569–575 (2021).
Iwamoto, M. et al. Trends in invasive methicillin-resistant Staphylococcus aureus infections. Pediatrics 132, e817–e824 (2013).
Friedland, I. R., du Plessis, J. & Cilliers, A. Cardiac complications in children with Staphylococcus aureus bacteremia. J. Pediatr. 127, 746–748 (1995).
Vogel, M. et al. Infectious disease consultation for Staphylococcus aureus bacteremia – a systematic review and meta-analysis. J. Infect. 72, 19–28 (2016).
Tissot, F. et al. Mandatory infectious diseases consultation for MRSA bacteremia is associated with reduced mortality. J. Infect. 69, 226–234 (2014).
Borde, J. P. et al. Adherence to an antibiotic stewardship bundle targeting Staphylococcus aureus blood stream infections at a 200-bed community hospital. Infection 42, 713–719 (2014).
Schmitt, S. et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin. Infect. Dis. 58, 22–28 (2014).
Hadano, Y. et al. Reduction of 30-day death rates from Staphylococcus aureus bacteremia by mandatory infectious diseases consultation: comparative study interventions with and without an infectious disease specialist. Int J. Infect. Dis. 103, 308–315 (2021).
Fries, B. L. et al. Infectious diseases consultation and the management of Staphylococcus aureus bacteremia. Clin. Infect. Dis. 58, 598–599 (2014).
Ten Oever, J. et al. Development of quality indicators for the management of Staphylococcus aureus bacteraemia. J. Antimicrob. Chemother. 74, 3344–3351 (2019).
Saunderson, R. B. et al. Impact of infectious diseases consultation on the management of Staphylococcus aureus bacteraemia in children. BMJ Open 4, e004659 (2014).
Campbell, A. J. et al. Pediatric Staphylococcus aureus bacteremia: clinical spectrum and predictors of poor outcome. Clin. Infect. Dis. 74, 604–613 (2022).
Liu, C. et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 52, e18–e55 (2011).
McMullan, B. J. et al. Clinical management of Staphylococcus aureus bacteremia in neonates, children, and adolescents. Pediatrics 146, e20200134 (2020).
Yang, D. & Dalton, J. E. A unified approach to measuring the effect size between two groups using SAS. In: SAS Global Forum (Orlando FL, 2012).
Hamdy, R. F. et al. Epidemiology of methicillin-resistant Staphylococcus aureus bacteremia in children. Pediatrics 139, e20170183 (2017).
Lloyd, E. C. et al. Impact of a Best Practice Advisory for pediatric patients with Staphylococcus aureus bacteremia. J. Pediatric Infect. Dis. Soc. 10, 282–288 (2021).
Messacar, K. et al. A handshake from antimicrobial stewardship opens doors for infectious disease consultations. Clin. Infect. Dis. 64, 1449–1452 (2017).
Mayer, M. L. Disparities in geographic access to pediatric subspecialty care. Matern Child Health J. 12, 624–632 (2008).
Acknowledgements
We thank Andrew Janowski, MD, Patrick Reich, MD, MSCI, and David Hunstad, MD, for study design contributions and thoughtful review of the manuscript.
Funding
This work was supported by the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital; National Institutes of Health (NIH)/National Center for Advancing Translational Sciences [grant number UL1-TR002345 and TL1-TR002344 to K.J.W.]; and the Agency for Healthcare Research and Quality (AHRQ) [grant number R01-HS024269 to S.A.F.]. These funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or AHRQ.
Author information
Authors and Affiliations
Contributions
All authors confirm that they have contributed significantly to the work, have seen and approved the submission of this version of the manuscript, and take full responsibility for the manuscript. Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: K.J.W., Y.M., A.M.B., P.G.H., F.A., J.F., G.M., J.J.M., J.G.N., and S.A.F. Drafting the article or revising it critically for important intellectual content: K.J.W., A.M.B., P.G.H., J.G.N., and S.A.F. Final approval of the version to be published: K.J.W., Y.M., A.M.B., P.G.H., F.A., J.F., G.M., J.J.M., J.G.N., and S.A.F.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Whittington, K.J., Ma, Y., Butler, A.M. et al. The impact of infectious diseases consultation for children with Staphylococcus aureus bacteremia. Pediatr Res 92, 1598–1605 (2022). https://doi.org/10.1038/s41390-022-02251-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02251-0