Abstract
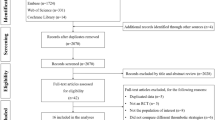
Direct oral anticoagulants (DOACs) are widely used to treat venous thromboembolism (VTE) in adults. Little attention is given to pediatric VTE (PVTE). The objective of this study is to study the efficacy and safety of DOACs in published PVTE randomized control trials (RCTs). PubMed, Embase, China National Knowledge Infrastructure, the Cochrane Library, SinoMed, and ClinicalTrials.gov were searched until 2021, to identify RCTs that enrolled patients with VTE <18 years of age who received DOACs versus standard anticoagulation. Outcomes were evaluated using the Mantel–Haenszel method of random-effects model. Our study evaluated seven RCTs that included 1139 cases of PVTE, which had a low risk of publication and assessment bias. Compared with standard anticoagulation, patients receiving DOACs presented a lower rate of recurrent VTE (relative risk [RR], 0.42 [confidence interval {CI}, 0.20 to 0.89]), similar mortality rate (RR, 0.50 [CI, 0.07 to 3.57]), major bleeding (RR, 0.46 [CI, 0.14 to 1.57]), and higher clinically relevant nonmajor bleeding (RR, 2.71 [CI, 1.05 to 7.02]) with low heterogeneity. Limiting to subgroups, dabigatran and rivaroxaban yielded similar findings, except for a higher incidence of nonmajor bleeding during rivaroxaban use. DOACs could be an alternative to standard anticoagulation in PVTE. Dabigatran and rivaroxaban have similar effects.
Impact
-
In venous thromboembolism (VTE), direct oral anticoagulants (DOACs) are widely used as a substitution for standard anticoagulation in most situations for adults; however, little attention is paid to the pediatric population.
-
For pediatric VTE, previous meta-analyses have emphasized the epidemiology, risk factors, and the use of traditional anticoagulants, and seldom reported the use of novel oral anticoagulants.
-
This is the first meta-analysis of randomized controlled trials that focuses on the efficacy outcomes and safety endpoints of DOACs compared with standard anticoagulation in pediatric VTE.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets used and analyzed in this study are available from the corresponding author upon reasonable request. All data generated or analyzed during this study are included in the article.
References
Raffini, L., Huang, Y. S., Witmer, C. & Feudtner, C. Dramatic increase in venous thromboembolism in children's hospitals in the United States from 2001 to 2007. Pediatrics 124, 1001–1008 (2009).
Brown, M. A. & Fulkerson, D. H. Incidence of venous thromboembolism in hospitalized pediatric neurosurgical patients: a retrospective 25-year institutional experience. Childs Nerv. Syst. 36, 987–992 (2020).
Sharathkumar, A. A. et al. Epidemiology and outcomes of clinically unsuspected venous thromboembolism in children: a systematic review. J. Thromb. Haemost. 18, 1100–1112 (2020).
Bidlingmaier, C. et al. Safety and efficacy of low molecular weight heparins in children: a systematic review of the literature and meta-analysis of single-arm studies. Semin Thromb. Hemost. 37, 814–825 (2011).
Monagle, P. & Newall, F. Management of thrombosis in children and neonates: practical use of anticoagulants in children. Hematol. Am. Soc. Hematol. Educ. Program 2018, 399–404 (2018).
Goldenberg, N. A. et al. Improving evidence on anticoagulant therapies for venous thromboembolism in children: key challenges and opportunities. Blood 126, 2541–2547 (2015).
Chopard, R., Albertsen, I. E., & Piazza, G. Diagnosis and treatment of lower extremity venous thromboembolism: a review. JAMA 324, 1765–1776 (2020).
Renner, E. & Barnes, G. D. Antithrombotic management of venous thromboembolism: JACC Focus Seminar. J. Am. Coll. Cardiol. 76, 2142–2154 (2020).
Macartney, C. A. & Chan, A. K. Thrombosis in children. Semin Thromb. Hemost. 37, 763–761 (2011).
Monagle, P. et al. American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2, 3292–3316 (2018).
Davila, J. G. et al. Characterizing the use of direct oral anticoagulants in children using the American Thrombosis and Hemostasis Network Dataset (ATHNdataset). Blood 134, 1156 (2019).
Davila, J. G. et al. Athn 15: characterizing the real-world use of direct oral anticoagulants in pediatric patients – interim analysis. Blood 136, 19-20 (2020).
Kucine, N. et al. Provider practices regarding prophylactic anticoagulation in children with leukemia. Blood 134, 3412 (2019).
Pinchinat, A. et al. A pilot study of an oral anticoagulant, apixaban, in secondary prophylaxis of venous thromboembolism (VTE) in children and adolescents. Blood 134, 4 (2019).
Manis, M. M., Cummins, L. E., Kyle, J. A. & Taylor, S. M. Successful use of apixaban for Paget-Schroetter syndrome in a pediatric patient. J. Pediatr. Pharm. Ther. 26, 508–511 (2021).
Schulman, S. & Kearon, C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 3, 692–694 (2005).
Kaatz, S. et al. Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J. Thromb. Haemost. 13, 2119–2126 (2015).
Corbett, M. S., Higgins, J. P. & Woolacott, N. F. Assessing baseline imbalance in randomised trials: implications for the Cochrane risk of bias tool. Res Synth. Methods 5, 79–85 (2014).
Palys, K. E. & Berger, V. W. A note on the jadad score as an efficient tool for measuring trial quality. J. Gastrointest. Surg. 17, 1170–1171 (2013).
Kahan, B. C. & Harhay, M. O. Many multicenter trials had few events per center, requiring analysis via random-effects models or GEEs. J. Clin. Epidemiol. 68, 1504–1511 (2015).
Chalmers, E. et al. Guideline on the investigation, management and prevention of venous thrombosis in children. Br. J. Haematol. 154, 196–207 (2011).
Lebas, A. et al. EPNS/SFNP guideline on the anticoagulant treatment of cerebral sinovenous thrombosis in children and neonates. Eur. J. Paediatr. Neurol. 16, 219–228 (2012).
Monagle, P. et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141, e737S–e801S (2012).
Bai, Y., Deng, H., Shantsila, A. & Lip, G. Rivaroxaban versus dabigatran or warfarin in real-world studies of stroke prevention in atrial fibrillation: systematic review and meta-analysis. Stroke 48, 970–976 (2017).
Shah, S. H. et al. Clinical risk factors for central line-associated venous thrombosis in children. Front Pediatr. 3, 35 (2015).
Patel, N. et al. Rates of venous thromboembolism and central line-associated bloodstream infections among types of central venous access devices in critically ill children. Crit. Care Med. 48, 1340–1348 (2020).
Onyeama, S. N. et al. Central venous catheter-associated venous thromboembolism in children with hematologic malignancy. J. Pediatr. Hematol. Oncol. 40, e519–e524 (2018).
Mitchell, W. B. et al. Children and young adults hospitalized for severe COVID-19 exhibit thrombotic coagulopathy. Pediatr. Blood Cancer 68, e28975 (2021).
Betensky, M. & Goldenberg, N. A. Post-thrombotic syndrome in children. Thromb. Res. 164, 129–135 (2018).
Carpenter, S. L., Richardson, T. & Hall, M. Increasing rate of pulmonary embolism diagnosed in hospitalized children in the United States from 2001 to 2014. Blood Adv. 2, 1403–1408 (2018).
Blevins, E. M. et al. A multicenter cohort study of inferior vena cava filter use in children. Pediatr. Blood Cancer 62, 2089–2093 (2015).
Neshat-Vahid, S. et al. Association of thrombophilia and catheter-associated thrombosis in children: a systematic review and meta-analysis. J. Thromb. Haemost. 14, 1749–1758 (2016).
Mai, V. et al. Extended anticoagulation for VTE: a systematic review and meta-analysis. Chest 155, 1199–1216 (2019).
Chaudhary, R. et al. DOACs versus VKAs in older adults treated for acute venous thromboembolism: systematic review and meta-analysis. J. Am. Geriatr. Soc. 68, 2021–2026 (2020).
Schoot, R. A., Kremer, L. C., van de Wetering, M. D. & van Ommen, C. H. Systemic treatments for the prevention of venous thrombo-embolic events in paediatric cancer patients with tunnelled central venous catheters. Cochrane Database Syst. Rev. 9, Cd009160 (2013).
Mahajerin, A. et al. Hospital-associated venous thromboembolism in pediatrics: a systematic review and meta-analysis of risk factors and risk-assessment models. Haematologica 100, 1045–1050 (2015).
Klaassen, I. L. M. et al. Are low-molecular-weight heparins safe and effective in children? A systematic review. Blood Rev. 33, 33–42 (2019).
Engel, E. R. et al. Predictors of postthrombotic syndrome in pediatric thrombosis: a systematic review and meta-analysis of the literature. J. Thromb. Haemost. 18, 2601–2612 (2020).
Brandão, L. R. et al. Safety of dabigatran etexilate for the secondary prevention of venous thromboembolism in children. Blood 135, 491–504 (2020).
Yee, D. L., O'Brien, S. H. & Young, G. Pharmacokinetics and pharmacodynamics of anticoagulants in paediatric patients. Clin. Pharmacokinet. 52, 967–980 (2013).
Halton, J. M. L. et al. Pharmacokinetics, pharmacodynamics, safety and tolerability of dabigatran etexilate oral liquid formulation in infants with venous thromboembolism. Thromb. Haemost. 117, 2168–2175 (2017).
Yetman, R. J. et al. Apixaban pharmacodynamic activity in umbilical cord, paediatric, and adult plasma. Thromb. Haemost. 117, 1518–1527 (2017).
Monagle, P. et al. Bodyweight-adjusted rivaroxaban for children with venous thromboembolism (EINSTEIN-Jr): results from three multicentre, single-arm, phase 2 studies. Lancet Haematol. 6, e500–e509 (2019).
Sinegre, T. et al. In vitro assessment of edoxaban anticoagulant effect in pediatric plasma. Thromb. Res. 178, 112–118 (2019).
Esch, J. J., Hellinger, A., Friedman, K. G. & VanderPluym, C. J. Apixaban for treatment of intracardiac thrombosis in children with congenital heart disease. Interact. Cardiovasc Thorac. Surg. 30, 950–951 (2020).
Jaffray, J. & Young, G. Direct oral anticoagulants for use in paediatrics. Lancet Child Adolesc. Health 6, 207–214 (2022).
Branstetter, J. et al. Efficacy and safety of non-vitamin K antagonist oral anticoagulants in pediatric venous thromboembolism treatment and thromboprophylaxis: a systematic review of the literature. Semin. Thrombosis Hemost. 47, 643–653 (2021).
Ng, C. et al. A network meta-analysis of direct oral anticoagulants for portal vein thrombosis in cirrhosis. Hepatol. Int. 15, 1196–1206 (2021).
Funding
Project of Hunan Provincial Health Commission (B2019111). Hunan Provincial Natural Science Foundation Project (2020JJ5504, 2022JJ40385); Guangxi Science and Technology Planning Project (2017AB45033).
Author information
Authors and Affiliations
Contributions
Conception and study design: J.C., G.S.B., X.Q.; data search and extraction: J.C., F.W.; data analysis: J.C., G.S.B., F.W.; manuscript revision: X.Q. All authors were involved in writing the paper, and in reading and approving the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, J., Bi, G., Wu, F. et al. Direct oral anticoagulants versus standard anticoagulation in children treated for acute venous thromboembolism. Pediatr Res 93, 1491–1498 (2023). https://doi.org/10.1038/s41390-022-02294-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02294-3
This article is cited by
-
Efficacy and Safety of Direct Oral Anticoagulants in Pediatric Venous Thromboembolism: A Systematic Review and Meta-Analysis
Indian Journal of Pediatrics (2025)
-
Efficacy and safety of antithrombotic therapy for preventing and treating pediatric thromboembolic disease: a systematic review
Scientific Reports (2024)
-
Comparison of the efficacy and safety between rivaroxaban and dabigatran in the treatment of acute portal vein thrombosis in cirrhosis
BMC Gastroenterology (2023)