Abstract
Background
Celiac disease (CD) in children and adolescents has been linked with increased susceptibility for cardiometabolic disease in adulthood. We explored the interaction between body composition and metabolic syndrome (MetS) components in pediatric CD.
Methods
We conducted a retrospective observational study of patients with CD followed at our Pediatric Endocrine and Gastroenterology Units between 1/2018-1/2022. Data on sociodemographic, clinical, laboratory, and body composition parameters (bioelectrical impedance analysis, BIA) were collected.
Results
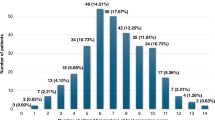
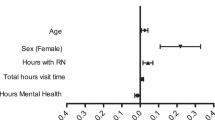
Forty-four patients with MetS components and 67 patients without them were enrolled. The cohort’s mean age at BIA assessment was 11.5 ± 3.6 years. Individuals with MetS components were older (P = 0.045), had higher BMI z-scores (P < 0.001), higher total and truncal fat percentage levels (P < 0.001), lower muscle-to-fat ratio z-scores (P = 0.018), higher sarcopenic indices (P = 0.05), higher systolic blood pressure percentiles (P = 0.001), higher triglycerides levels (P = 0.009), and higher triglycerides/HDL-c ratios (P < 0.001) than those without MetS components. A sex- and age-adjusted model revealed that the diagnosis of MetS components was positively associated with fat percentage (odds ratio = 1.087, confidence interval [1.010–1.171], P = 0.027), but not with BMI z-scores (P = 0.138).
Conclusions
We found that fat percentage but not weight status is associated with risk for MetS components in individuals with childhood-onset CD. Preventive interventions should target an improvement in body composition.
Impact
-
The literature on cardiometabolic risk in pediatric patients with celiac disease (CD) is sparse.
-
Our analysis revealed that at least one metabolic syndrome (MetS) component was present in two out of every five children and adolescents with CD.
-
An increase in fat percentage but not in body mass index z-scores predicted the presence of MetS components in our cohort.
-
These findings suggest that the weight status of children and adolescents with CD does not mirror their risk for MetS components.
-
Body composition analysis should be considered as an integral part of the clinical evaluation in young patients with CD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Husby, S. et al. European society paediatric gastroenterology, hepatology and nutrition guidelines for diagnosing coeliac disease 2020. J. Pediatr. Gastroenterol. Nutr. 70, 141–156 (2020).
Ward, Z. J. et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N. Engl. J. Med. 381, 2440–2450 (2019).
Theethira, T. G. & Dennis, M. Celiac disease and the gluten-free diet: consequences and recommendations for improvement. Dig. Dis. 33, 175–182 (2015).
Anania, C., Pacifico, L., Olivero, F., Perla, F. M. & Chiesa, C. Cardiometabolic risk factors in children with celiac disease on a gluten-free diet. World J. Clin. Pediatr. 6, 143–148 (2017).
Lerner, A. & Blank, M. Hypercoagulability in celiac disease-an update. Autoimmun. Rev. 13, 1138–1141 (2014).
Ungprasert, P., Wijarnpreecha, K. & Tanratana, P. Risk of venous thromboembolism in patients with celiac disease: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 31, 1240–1245 (2016).
Deutschmann, A. et al. Onset of thrombin generation occurs more rapidly in pediatric patients with celiac disease. J. Pediatr. Gastroenterol. Nutr. 61, 230–233 (2015).
West, J., Logan, R. F., Card, T. R., Smith, C. & Hubbard, R. Risk of vascular disease in adults with diagnosed coeliac disease: a population-based study. Aliment Pharm. Ther. 20, 73–79 (2004).
Zifman, E. et al. The effect of gluten-free diet on cardiovascular risk factors in newly diagnosed pediatric celiac disease patients. J. Pediatr. Gastroenterol. Nutr. 68, 684–688 (2019).
Norsa, L. et al. Cardiovascular disease risk factor profiles in children with celiac disease on gluten-free diets. World J. Gastroenterol. 19, 5658–5664 (2013).
Wei, L. et al. The association between coeliac disease and cardiovascular disease. Aliment Pharm. Ther. 27, 514–519 (2008).
Ford, E. & Chaoyang, L. Defining the metabolic syndrome in children and adolescents: Will the real definition please stand up? J. Pediatr. 152, 160–164 (2008).
Magge, S. N., Goodman, E. & Armstrong, S. C. The metabolic syndrome in children and adolescents: Shifting the focus to cardiometabolic risk factor clustering. Pediatrics. 140, e20171603 (2017).
Shalitin, S. & Wabitsch, M. Obesity and metabolic syndrome in the pediatric age. Horm. Res Paediatr. 95, 103 (2022).
Kyle, U. G., Earthman, C. P., Pichard, C. & Coss-Bu, J. A. Body composition during growth in children: limitations and perspectives of bioelectrical impedance analysis. Eur. J. Clin. Nutr. 69, 1298–1305 (2015).
McCarthy, H. D. Body fat measurements in children as predictors for the metabolic syndrome: focus on waist circumference. Proc. Nutr. Soc. 65, 385–392 (2006).
Salton, N. et al. Muscle-to-fat ratio for predicting metabolic syndrome components in children with overweight and obesity. Child Obes. 18, 132–142 (2022).
Brener, A. et al. Sex differences in body composition in youth with type 1 diabetes and its predictive value in cardiovascular disease risk assessment. Diabetes Metab. Res. Rev. 21, e3584 (2022).
Więch, P. et al. The relationship between body composition and a gluten free diet in children with celiac disease. Nutrients 10, 1817 (2018).
Barone, M. et al. A comparison of the nutritional status between adult celiac patients on a long-term, strictly gluten-free diet and healthy subjects. Eur. J. Clin. Nutr. 70, 23–27 (2016).
Vereczkei, Z. et al. It is high time for personalized dietary counseling in celiac disease: A systematic review and meta-analysis on body composition. Nutrients 13, 2947 (2021).
Marshall, W. A. & Tanner, J. M. Variations in the pattern of pubertal changes in boys. Arch. Dis. Child 45, 13–23 (1970).
Marshall, W. A. & Tanner, J. M. Variations in pattern of pubertal changes in girls. Arch. Dis. Child 44, 291–303 (1969).
Oberhuber, G., Granditsch, G. & Vogelsang, H. The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur. J. Gastroenterol. Hepatol. 11, 1185–1194 (1999).
Lee, S. Y. & Gallagher, D. Assessment methods in human body composition. Curr. Opin. Clin. Nutr. Metab. Care 11, 566–572 (2008).
Shypailo, R. J. & Motil, K. J. The use of bioimpedance in pediatric health, nutrition, and disease. J. Pediatr. Gastroenterol. Nutr. 67, 435–436 (2018).
McCarthy, H. D., Samani-Radia, D., Jebb, S. A. & Prentice, A. M. Skeletal muscle mass reference curves for children and adolescents. Pediatr. Obes. 9, 249–259 (2014).
Israel Central Bureau of Statistics (CBS). Characterization and classification of geographical units by the socio-economic level of the population, 2015 (2020) https://www.cbs.gov.il/he/publications/DocLib/2020/1765_socio_economic_2015/e_print.pdfref
Chou, J. H., Roumiantsev, S. & Singh, R. PediTools electronic growth chart calculators: applications in clinical care, research, and quality improvement. J. Med. Internet Res. Jan. 22, e16204 (2020).
Kuczmarski, R. J. et al. 2000 CDC Growth charts for the United States: methods and development. Vital-. Health Stat. 11, 1–190 (2002).
Ogden, C. L. & Flegal, K. M. Changes in terminology for childhood overweight and obesity. Natl Health Stat. Rep. 25, 1–5 (2010). PMID: 20939253.
Tanner, J. M., Goldstein, H. & Whitehouse, R. H. Standards for children’s height at ages 2-9 years allowing for heights of parents. Arch. Dis. Child 45, 755–762 (1970).
Shypailo, R. Age-based pediatric blood pressure reference charts (2018). Retrieved 1/14/2021 from the Baylor College of Medicine, Children’s Nutrition Research Center, Body Composition Laboratory Web Site. https://www.bcm.edu/bodycomplab/BPappZjs/BPvAgeAPPz.html.
Flynn, J. T. et al. Subcommittee on screening and management of high blood pressure in children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 140, e20171904 (2017).
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128(Suppl 5), S213–S256 (2011).
Pantoja-Torres, B. et al. Insulin Resistance and Metabolic Syndrome Research Group. High triglycerides to HDL-cholesterol ratio is associated with insulin resistance in normal-weight healthy adults. Diabetes Metab. Syndr. 13, 382–388 (2019).
Urbina, E. M. et al. Triglyceride to HDL-C ratio and increased arterial stiffness in children, adolescents, and young adults. Pediatrics 131, e1082–e1090 (2013).
Giannini, C. et al. The triglyceride-to-HDL cholesterol ratio: association with insulin resistance in obese youths of different ethnic backgrounds. Diabetes Care 34, 1869–1874 (2011).
Israel Center for Disease Control, Ministry of Health State of Israel. Mabat Youth Second National Health and Nutrition Survey of 7th–12th grade students 2015–2016. Publication no. 373. https://www.health.gov.il/publicationsfiles/mabat_kids2_11_2015-2016-eng.pdf (2017).
Auricchio, R. et al. Gluten consumption and inflammation affect the development of celiac disease in at-risk children. Sci. Rep. 12, 5396 (2022).
Tuttle, C. S. L., Thang, L. A. N. & Maier, A. B. Markers of inflammation and their association with muscle strength and mass: A systematic review and meta-analysis. Ageing Res Rev. 64, 101185 (2020).
Tilg, H. & Moschen, A. R. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat. Rev. Immunol. 6, 772–783 (2006).
Nishikawa, H., Asai, A., Fukunishi, S., Nishiguchi, S. & Higuchi, K. Metabolic Syndrome and Sarcopenia. Nutrients 13, 3519 (2021).
Anafy, A. et al. The effect of gluten-free diet on body mass index in paediatric celiac disease. Acta Paediatr. 110, 2233–2239 (2021).
Aljada, B., Zohni, A. & El-Matary, W. The gluten-free diet for celiac disease and beyond. Nutrients 13, 3993 (2021).
Melini, V. & Melini, F. Gluten-free diet: gaps and needs for a healthier diet. Nutrients 11, 170 (2019).
Calvo-Lerma, J. et al. Differences in the macronutrient and dietary fibre profile of gluten-free products as compared to their gluten-containing counterparts. Eur. J. Clin. Nutr. 73(Jun), 930–936 (2019).
Brener, A. et al. The heritability of body composition. BMC Pediatr. 21, 225 (2021).
Jung, J. Y. et al. Levels of systolic and diastolic blood pressure and their relation to incident metabolic syndrome. Cardiology 142, 224–231 (2019).
Hansen, M. L., Gunn, P. W. & Kaelber, D. C. Underdiagnosis of hypertension in children and adolescents. JAMA 298, 874–879 (2007).
Myette, R. L., Burger, D., Geier, P. & Feber, J. Diastolic hypertension is associated with proteinuria in pediatric patients. Health Sci. Rep. 4, e346 (2021).
Acknowledgements
This work was performed by Oren Kassner in partial fulfillment of the MD thesis requirements of the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel. We are grateful to Esther Eshkol for editorial assistance.
Author information
Authors and Affiliations
Contributions
A.Y.-F. substantial contribution to the conception and design of the study, interpretation of data analysis and drafting of the article. O.K. made a substantial contribution to the design of the study, curation, statistical analysis and interpretation of the data and drafting of the article. Y.F., H.M.-L., A.A., D.L., H.I., E.E.-T., and S.C. made a substantial contribution to the curation and interpretation of the data and revised the manuscript for important intellectual content. Y.L. and A.B. made a substantial contribution to the conception and design of the study, interpretation of data analysis and revised the manuscript for important intellectual content incorporating the comments of all co-authors. A.B. is the guarantor of this work, and as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
The study was approved by the Ethics Committee of the Tel-Aviv Sourasky Medical Center according to the Helsinki Declaration. Informed consent by the participants was waived since the data were retrieved from the subjects’ medical records and all personal identification was omitted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yerushalmy-Feler, A., Kassner, O., Frank, Y. et al. Body composition in pediatric celiac disease and metabolic syndrome component risk—an observational study. Pediatr Res 94, 618–625 (2023). https://doi.org/10.1038/s41390-023-02496-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-023-02496-3
This article is cited by
-
Body composition in prepubertal children with idiopathic premature adrenarche: implications for cardiometabolic health
Pediatric Research (2025)
-
The role of IGF1 in determining body composition in children and adolescents with growth hormone deficiency and those with idiopathic short stature
Endocrine (2024)