Abstract
Background
This study evaluated of clinical characteristics, outcomes, and mortality risk factors of a severe multisystem inflammatory syndrome in children admitted to a the pediatric intensive care unit.
Methods
A retrospective multicenter cohort study was conducted between March 2020 and April 2021 at 41 PICUs in Turkey. The study population comprised 322 children diagnosed with multisystem inflammatory syndrome.
Results
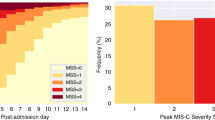
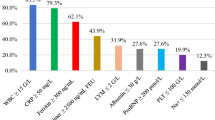
The organ systems most commonly involved were the cardiovascular and hematological systems. Intravenous immunoglobulin was used in 294 (91.3%) patients and corticosteroids in 266 (82.6%). Seventy-five (23.3%) children received therapeutic plasma exchange treatment. Patients with a longer duration of the PICU stay had more frequent respiratory, hematological, or renal involvement, and also had higher D-dimer, CK-MB, and procalcitonin levels. A total of 16 patients died, with mortality higher in patients with renal, respiratory, or neurological involvement, with severe cardiac impairment or shock. The non-surviving group also had higher leukocyte counts, lactate and ferritin levels, and a need for mechanical ventilation.
Conclusions
In cases of MIS-C, high levels of D-dimer and CK-MB are associated with a longer duration of PICU stay. Non-survival correlates with elevated leukocyte counts and lactate and ferritin levels. We were unable to show any positive effect of therapeutic plasma exchange therapy on mortality.
Impact
-
MIS-C is a life-threatening condition.
-
Patients need to be followed up in the intensive care unit.
-
Early detection of factors associated with mortality can improve outcomes.
-
Determining the factors associated with mortality and length of stay will help clinicians in patient management.
-
High D-dimer and CK-MB levels were associated with longer PICU stay, and higher leukocyte counts, ferritin and lactate levels, and mechanical ventilation were associated with mortality in MIS-C patients.
-
We were unable to show any positive effect of therapeutic plasma exchange therapy on mortality.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed in the current study are not publicly available as the patients were in intensive care, but they available from the corresponding author upon reasonable request.
References
Rosenberg, E. S. et al. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York State—March 2020. Clin. Infect. Dis. 71, 1953–1959 (2020).
World Health Organization. Coronavirus diseases (COVID-19) situation report–2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200527-covid-19-sitrep-128.pdf?sfvrsn=11720c0a_2 (2020).
Castagnoli, R. et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 174, 882–889 (2020).
Yonker, L. M., Shen, K. & Kinane, T. B. Lessons unfolding from pe- diatric cases of COVID-19 disease caused by SARS-CoV-2 infection. Pediatr. Pulmonol. 55, 1085–1086 (2020).
Riphagen, S., Gomez, X., Gonzalez-Martinez, C., Wilkinson, N. & Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 395, 1607–1608 (2020).
Verdoni, L. et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 6736, 1–8 (2020).
Whittaker, E. et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA 324, 259–269 (2020).
Belhadjer, Z. et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation 142, 429–436 (2020).
Centers for Disease Control and Prevention. Multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19). CDC Health Alert Network. https://emergency.cdc.gov/han/2020/han00432.asp (2020).
Radia, T. et al. Multi-system inflammatory syndrome in children & adolescents (MIS-C): a systematic review of clinical features and presentation. Paediatr. Respir. Rev. 38, 51–57 (2021).
Emeksiz, S. et al. Therapeutic plasma exchange: a potential management strategy for critically ill MIS-C patients in the pediatric intensive care unit. Transfus. Apher. Sci. 60, 103119 (2021).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the european association of cardiovascular imaging. Eur. Heart J. Cardiovasc. Imaging 16, 233–271 (2015).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Pollack, M. M., Patel, K. M. & Ruttimann, U. E. PRISM III: an updated pediatric risk of mortality score. Crit. Care Med. 24, 743–752 (1996).
Leteurtre, S. et al. PELOD-2: an update of the Pediatric logistic organ dysfunction score. Crit. Care Med. 41, 1761–1773 (2013).
Lima-Setta, F. et al. Multisystem inflammatory syndrome in children (MIS-C) during SARS-CoV-2 pandemic in Brazil: a multicenter, prospective cohort study. J. Pediatr. 97, 354–361 (2021).
Feldstein, L. R. et al. Multisystem inflammatory syndrome in US children and adolescents. N. Engl. J. Med. 383, 334–346 (2020).
Davies, P. et al. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: a multicentre observational study. Lancet Child Adolesc. Health 4, 669–677 (2020).
Scully, E. P., Haverfield, J., Ursin, R. L., Tannenbaum, C. & Klein, S. L. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat. Rev. Immunol. 20, 442–447 (2020).
Godfred-Cato, S. et al. COVID-19–associated multisystem inflammatory syndrome in children—United States, March–July 2020. Morb. Mortal. Wkly. Rep. 69, 1074 (2020).
Ahmed, M. et al. Multisystem inflammatory syndrome in children: a systematic review. EClinicalMedicine 26, 100527 (2020).
Son, M. B. F. et al. Multisystem inflammatory syndrome in children—initial therapy and outcomes. N. Engl. J. Med. 385, 23–34 (2021).
Maheshwari, A. et al. Comparison of clinical and laboratory profile of survivors and non‐survivors of SARS‐CoV‐2‐related multisystem inflammatory syndrome of childhood in India: an observational study. J. Paediatr. Child Health 58, 136–140 (2022).
Pereira, M. F. B. et al. Severe clinical spectrum with high mortality in pediatric patients with COVID-19 and multisystem inflammatory syndrome. Clinics 75, e2209 (2020).
Shekerdemian, L. et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 174, 868–873 (2020).
Zhao, Y., Yin, L., Patel, J., Tang, L. & Huang, Y. The inflammatory markers of multisystem inflammatory syndrome in children (MIS‐C) and adolescents associated with COVID‐19: a meta‐analysis. J. Med. Virol. 93, 4358–4369 (2021).
Dufort, E. M. et al. Multisystem inflammatory syndrome in children in New York State. N. Engl. J. Med. 383, 347–358 (2020).
Bautista-Rodriguez, C. et al. Multisystem inflammatory syndrome in children: an international survey. Pediatrics 147, e2020024554 (2021).
Capone, C. A. et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 infection. J. Pediatr. 224, 141–145 (2020).
García-Salido, A. et al. Severe manifestations of SARS-CoV-2 in children and adolescents: from COVID-19 pneumonia to multisystem inflammatory syndrome: a multicentre study in pediatric intensive care units in Spain. Crit. Care 24, 1–13. (2020).
Moraleda, C. et al. Multi-inflammatory syndrome in children related to SARS-CoV-2 in Spain. Clin. Infect. Dis. 72, e397–e401 (2021).
Lee, Y. P. et al. Distinct clinical and immunological features of SARS– CoV-2–induced multisystem inflammatory syndrome in children. J. Clin. Investig. 130, 5942–5950 (2020).
Toubiana, J. et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ 369, m2094 (2020).
Torres, J. P. et al. Multisystem inflammatory syndrome in children (MIS-C): Report of the clinical and epidemiological characteristics of cases in Santiago de Chile during the SARS-CoV-2 pandemic. Int. J. Infect. Dis. 100, 75–81 (2020).
Keith, P. et al. A novel treatment approach to the novel coronavirus: an argument for the use of therapeutic plasma exchange for fulminant COVID-19. Crit. Care 24, 128 (2020).
Author information
Authors and Affiliations
Consortia
Contributions
G.S., A.I., A.C., I.B., and A.A. conceptualized and designed the study, collected data, drafted the initial manuscript, and reviewed and revised the manuscript. N.A., S.K., F.A., T.K., G.A., O.S., F.V., P.Y.O., M.D., A.Z.B., S.O., G.A., M.K., S.B., U.A., A.B.A., M.H., A.F.Y., T.D., N.Z., A.O., H.S.K., F.İ.G., L.T., D.Y., N.Y., U.Y., M.A., M.A.K., M.C., A.D., F.B., F.S., M.O., S.T., C.K., A.Y., N.A., C.O., A.Y., E.S., B.K., C.D., E.G., S.E., P.S., E.S., H.F.A., M.B., F.D., S.E., G.O., M.D., M.N.T., G.O.Y., D.L., S.H., E.Z.B., M.M., A.B., N.K., E.A.O., M.N.O., F.E., M.U., A.E.A., N.O.K., A.B., S.Ö., T.C., Y.O., and A.O.K. collected data and designed the data collection instruments. T.K., H.S.K., D.Y., N.Y., and E.S. collected data, critically reviewed the manuscript for important intellectual content, and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Scientific Research Platform of the Turkish Republic Ministry of Health and was ethically approved by Acıbadem Mehmet Ali Aydınlar University Medical Research Evaluation board (2021-02/16). Since it was a retrospective study, ethics committee approval was obtained while patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sık, G., Inamlık, A., Akçay, N. et al. Mortality risk factors among critically ill children with MIS-C in PICUs: a multicenter study. Pediatr Res 94, 730–737 (2023). https://doi.org/10.1038/s41390-023-02518-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-023-02518-0
This article is cited by
-
The association between abdominal ultrasound findings and clinical severity in MIS-C children with extracardiac symptoms
European Journal of Pediatrics (2025)
-
Acute kidney injury in children with moderate-severe COVID-19 and multisystem inflammatory syndrome in children: a referral center experience
Pediatric Nephrology (2024)