Abstract
Background
A wide range of outcomes for infants and parents has been reported in clinical trials testing FCC interventions. This systematic review aimed to identify outcomes, outcome measures, and time-points reported in experimental studies testing FCC interventions in neonatal care units.
Methods
This review included experimental studies investigating FCC interventions in neonatal settings. Database searches were conducted in MEDLINE, EMBASE, CINAHL, Cochrane, PsycINFO, Scopus, JBI, Lilacs, and SciELO, completed in December 2022 and updated in November 2023. Critical appraisal was performed using the JBI checklist for randomized controlled trials, and a narrative synthesis process was used. Outcomes were categorized into the Comet Taxonomy core areas.
Results
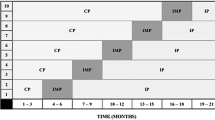
The search identified 8787 papers; 42 studies were included in the analysis. Totally, 60 outcomes were identified: 42 infant and 18 parents’ outcomes. Outcomes were clustered into 12 domains for infants and five domains for parents and measured by 97 outcome measures. The included studies reported 25 and 27 different time-points for infants and parents, respectively.
Conclusion
This review of studies testing FCC interventions identified heterogeneity and inconsistency of outcomes, outcome measures, and time-points measuring the outcomes. Developing a core outcome set for FCC studies is warranted to benchmark the evidence and identify best-practices.
Impact
-
This systematic review identified inconsistency of outcomes, outcome measures, and time-points reported in quantitative studies testing family-centered care interventions in neonatal care settings.
-
The lack of standardized outcomes and outcome measures reported in clinical trials makes it difficult to synthesize data to provide conclusive recommendations.
-
This systematic review will contribute to the development of a core outcome set for research testing family-centered care interventions in neonatal care settings.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The dataset generated during and /or analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization (WHO). Preterm Birth. https://www.who.int/news-room/fact-sheets/detail/preterm-birth (2021).
Mactier, H. et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch. Dis. Child Fetal Neonatal Ed. 105, 232–239 (2020).
van den Hoogen, A. et al. Parents’experience of VOICE: Anovel support programme in the NICU. Nurs. Crit. Care 26, 201–208 (2021).
Ding, X. et al. Effects of family-centred care interventions on preterm infants and parents in neonatal intensive care units: a systematic review and meta-analysis of randomised controlled trials. Aust. Crit. Care 32, 63–75 (2019).
Mendelson, T. et al. A mindfulness intervention to reduce maternal distress in neonatal intensive care: a mixed methods pilot study. Arch. Women’s Ment. Health 21, 791–799 (2018).
European Standards of Care Newborn Health. Infant & family-centered developmental care. https://newborn-health-standards.org/standards/standards-english/infant-family-centred-developmental-care/ (2019).
Mikkelsen, G. & Frederiksen, K. Family-centred care of children in hospital - a concept analysis. J. Adv. Nurs. 67, 1152–1162 (2011).
Oude Maatman, S. M. et al. Factors influencing implementation of family-centered care in a neonatal intensive care unit. Front. Pediatr. 8, 222 (2020).
Abukari, A. S. & Schmollgruber, S. Concepts of family-centered care at the neonatal and paediatric intensive care unit: a scoping review. J. Pediatr. Nurs. 71, e1–e10 (2023).
Banerjee, J., Aloysius, A., Platonos, K. & Deierl, A. Family centred care and family delivered care—what are we talking about? J. Neonatal Nurs. 24, 8–12 (2018).
Institute for Patient and Family Centred Care. What is PFCC? https://www.ipfcc.org/about/pfcc.html (2021).
Segers, E., Ockhuijsen, H., Baarendse, P., van Eerden, I. & van den Hoogen, A. The impact of family centred care interventions in a neonatal or paediatric intensive care unit on parents’ satisfaction and length of stay: a systematic review. Intensive Crit. Care Nurs. 50, 63–70 (2019).
Yu, X. & Zhang, J. Family‐centred care for hospitalized preterm infants: a systematic review and meta‐analysis. Int. J. Nurs. Pract. 25, e12705 (2019).
Williamson, P. R. et al. The Comet Handbook: Version 1.0. Trials 18, 1–50 (2017).
Webbe, J. W. H. et al. Core outcomes in neonatology: development of a core outcome set for neonatal research. Arch. Dis. Child. Fetal Neonatal Ed. 105, 425–431 (2020).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst. Rev. 10, 89 (2021).
Latour, J., van den Hoogen, A., Axelin, A., Kostenzer, J. Evaluating family-centered care interventions and outcomes in neonatal care. PROSPERO. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022297580 (2022).
Westrup, B. Newborn individualized developmental care and assessment program (Nidcap)—family-centered developmentally supportive care. Early Hum. Dev. 83, 443–449 (2007).
Tufanaru, C., Munn, Z., Aromataris, E., Campbell, J., Hopp, L. Systematic reviews of effectiveness. In: Aromataris E, Munn Z, editors, JBI Manual for Evidence Synthesis. https://synthesismanual.jbi.global (2020).
Dodd, S. et al. A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. J. Clin. Epidemiol. 96, 84–92 (2018).
Abdeyazdan, Z., Shahkolahi, Z., Mehrabi, T. & Hajiheidari, M. A family support intervention to reduce stress among parents of preterm infants in neonatal intensive care unit. Iran. J. Nurs. Midwifery Res. 19, 349–353 (2014).
Ahlqvist‐Björkroth, S. et al. Fewer maternal depression symptoms after the close collaboration with parents intervention: two‐year follow‐up. Acta Paediatr. 111, 1160–1166 (2022).
Ansari, N. S., Franck, L. S., Tomlinson, C., Colucci, A. & O’Brien, K. A pilot study of family-integrated care (FICare) in critically Ill preterm and term infants in the Nicu: FICare Plus. Children 10, 1337 (2023).
Bastani, F., Abadi, T. A. & Haghani, H. Effect of family-centered care on improving parental satisfaction and reducing readmission among premature infants: a randomized controlled trial. J. Clin. Diagn. Res. 9, SC04–SC08 (2015).
Borimnejad, L., Mehrnoosh, N., Fatemi, N. S. & Haghani, H. Impacts of creating opportunities for parent empowerment on maternal stress: a quasi-experimental study. Iran. J. Nurs. Midwifery Res. 18, 218–221 (2013).
Bostanabad, M., NamdarArshatnab, H., Balila, M., Asghari Jafarabadi, M. & Ravanbakhsh, K. Effect of family-centered intervention in neonatal intensive care unit on anxiety of parents. Int. J. Pediatr. 5, 5101–5111 (2017).
Chen, H. & Dong, L. The effect of family integrated care on the prognosis of premature infants. BMC Pediatr. 22, 1–7 (2022).
Dai, K. et al. Application of family-centered empowerment model in primary caregivers of premature infants: a quasi-experimental study. Front. Pediatr. 11, 1137188 (2023).
De Bernardo, G., Svelto, M., Giordano, M., Sordino, D. & Riccitelli, M. Application of family-centered empowerment model in primary caregivers of premature infants: a quasi-experimental study. Italian Journal of Pediatrics 43, 1–11 (2017).
Franck, L. S. et al. Neonatal outcomes from a quasi-experimental clinical trial of family integrated care versus family-centered care for preterm infants in U.S. Nicus. BMC Pediatr. 22, 1–14 (2022).
Franck, L. S. et al. Maternal mental health after infant discharge: a quasi-experimental clinical trial of family integrated care versus family-centered care for preterm infants in U.S. Nicus. BMC Pediatrics 23, 396 (2023).
Glazebrook, C. et al. Randomised Trial of a Parenting Intervention During Neonatal Intensive Care. Arch. Dis. Child. - Fetal Neonatal Ed. 92, F438–F443 (2007).
He, F. B. et al. Effectiveness of the close collaboration with parents intervention on parent-infant closeness in Nicu. BMC Pediatr. 21, 1–8 (2021).
He, S.-W. et al. Impact of Family Integrated Care on Infants’ Clinical Outcomes in Two Children’s Hospitals in China: A Pre-Post Intervention Study. Ital. J. Pediatr. 44, 1–7 (2018).
Hei, M. et al. Family integrated care for preterm infants in china: a cluster randomized controlled trial. J. Pediatr. 228, 36–43 e32 (2021).
Heo, Y. J. & Oh, W. O. The effectiveness of a parent participation improvement program for parents on partnership, attachment infant growth in a neonatal intensive care unit: a randomized controlled trial. Int J. Nurs. Stud. 95, 19–27 (2019).
Horner, S., Benbrook, K., Hoffman, M. & Libutti, L. Implementing Guidelines for Nicu Parent Presence: Effects on Parent and Infant Stress. J. Perinat. Neonatal. Nurs. (2023).
Ingram, J. C. et al. Does family-centred neonatal discharge planning reduce healthcare usage? A before and after study in South West England. BMJ Open 6, e010752 (2016).
Khanjari, S. et al. The effect of family-centered education on the quality of life of the parents of premature infants. J. Neonatal Nurs. 28, 407–412 (2022).
Lehtonen, L. et al. Parent–infant closeness after preterm birth and depressive symptoms: a longitudinal study. Front. Psychol. 13, 906531 (2022).
Liang, X., Miao, A., Zhang, W., Li, M. & Xing, Y. Effect of family integrated care on physical growth and language development of premature infants: a retrospective study. Transl. Pediatr. 11, 965–977 (2022).
Liu, M., Xu, Y. & Li, Y. Effects of family participatory nursing on clinical outcomes of premature infants in Nicu and families’ psychological status. Contrast Media Mol. Imaging 2022, 1–8 (2022).
Lv, B. et al. Family-centered care improves clinical outcomes of very-low-birth-weight infants: a quasi-experimental study. Front. Pediatr. 7, 138 (2019).
Månsson, C., Sivberg, B., Selander, B. & Lundqvist, P. The impact of an individualised neonatal parent support programme on parental stress: a quasi‐experimental study. Scand. J. Caring Sci. 33, 677–687 (2019).
McLean, M. A. et al. Lower maternal chronic physiological stress and better child behavior at 18 months: follow-up of a cluster randomized trial of neonatal intensive care unit family integrated care. J. Pediatr. 243, 107–115.e104 (2022).
Melnyk, B. M. et al. Improving cognitive development of low‐birth‐weight premature infants with the cope program: a pilot study of the benefit of early Nicu intervention with mothers. Res. Nurs. Health 24, 373–389 (2001).
Melnyk, B. M. et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics 118, e1414–e1427 (2006).
Mianaei, S. J., Karahroudy, F. A., Rassouli, M. & Tafreshi, M. Z. The effect of creating opportunities for parent empowerment program on maternal stress, anxiety, and participation in Nicu Wards in Iran. Iran. J. Nurs. Midwifery Res. 19, 94–100 (2014).
Nieves, H., Clements-Hickman, A. & Davies, C. C. Effect of a parent empowerment program on parental stress, satisfaction, and length of stay in the neonatal intensive care unit. J. Perinat. Neonatal Nurs. 35, 92–99 (2021).
O’Brien, K. et al. Effectiveness of family integrated care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc. Health 2, 245–254 (2018).
Ou, J., Zhong, X. & Zhang, X. Effects of family integrated care on weight gain in extremely preterm infants. Minerva Pediatr. 75, 253–259 (2023).
Penticuff, J. H. & Arheart, K. L. Effectiveness of an intervention to improve parent-professional collaboration in neonatal intensive care. J. Perinat. Neonatal Nurs. 19, 187–202 (2005).
Rajabzadeh, Z., Moudi, Z., Abbasi, A. & Miri-Aliabad, G. The effect of family-centered educational supportive intervention on parental stress of premature infants hospitalized in the Nicu. Med. Surg. Nurs. J. 9, e111847 (2021).
Sajadi, H., Akhoundzadeh, G. & Hojjati, H. The effect of empowerment program on participation of mothers with premature infants hospitalized in neonatal intensive care unit of Sayyed Shirazi Hospital in Gorgan, in 2018. Indian J. Forensic Med. Toxicol. 14, 1269–1276 (2020).
Samsudin, S. et al. The impact of structured kangaroo care education on premature infants’ weight gain, breastfeeding and length of hospitalization in Malaysia. J. Multidiscip. Healthc. 16, 1023–1035 (2023).
Van Veenendaal, N. R. et al. Association of a family integrated care model with paternal mental health outcomes during neonatal hospitalization. JAMA Netw. Open 5, e2144720 (2022).
Verma, A. et al. Family-centered care to complement care of sick newborns: a randomized controlled trial. Indian Pediatr. 54, 455–459 (2017).
Weis, J., Zoffmann, V., Greisen, G. & Egerod, I. The effect of person-centred communication on parental stress in a Nicu: a randomized clinical trial. Acta Paediatr. 102, 1130–1136 (2013).
Yu, Y.-T. et al. Family-centered care improved neonatal medical and neurobehavioral outcomes in preterm infants: randomized controlled trial. Phys. Ther. 97, 1158–1168 (2017).
Yu, Y.-T. et al. Family-centered care enhanced neonatal neurophysiological function in preterm infants: randomized controlled trial. Phys. Ther. 99, 1690–1702 (2019).
Zhang, R. et al. Involvement of parents in the care of preterm infants: a pilot study evaluating a family-centered care intervention in a chinese neonatal ICU. Pediatr. Crit. Care Med. 19, 741–747 (2018).
Zhang, Y. et al. Effect of family integrated care on maternal stress in preterm infants in the neonatal intensive care unit: a bi‐center experience. Asia-Pac. Psychiatry 15, e12521 (2023).
Beaton, D., Maxwell, L., Grosskleg, S., Shea, B. and Tugwell, P. The OMERACT Handbook Version 2.1. https://omeract.org/wp-content/uploads/2021/12/ (2021)
Williamson, P. R. et al. Developing core outcome sets for clinical trials: issues to consider. Trials 13, 132 (2012).
Bialy, L., Vandermeer, B., Lacaze‐Masmonteil, T., Dryden, D. M. & Hartling, L. A meta‐epidemiological study to examine the association between bias and treatment effects in neonatal trials. Evid. Based Child Health 9, 1052–1059 (2014).
Page, M. J. et al. Epidemiology and reporting characteristics of systematic reviews of biomedical research: a cross-sectional study. PLoS Med. 13, e1002028 (2016).
Moher, D., Tetzlaff, J., Tricco, A. C., Sampson, M. & Altman, D. G. Epidemiology and reporting characteristics of systematic reviews. PLoS Med. 4, e78 (2007).
Franck, L. S. et al. Improving family-centered care for infants in neonatal intensive care units: recommendations from frontline healthcare professionals. Adv. Neonatal Care 22, 79–86 (2022).
Raiskila, S. et al. Parents’ presence and parent–infant closeness in 11 neonatal intensive care units in six European countries vary between and within the countries. Acta Paediatr. 106, 878–888 (2017).
Alsadaan, N. et al. Impacts of integrating family-centered care and developmental care principles on neonatal neurodevelopmental outcomes among high-risk neonates. Children 10, 1751 (2023).
North, K. et al. Family Involvement in the Routine Care of Hospitalized Preterm or Low Birth Weight Infants: A Systematic Review and Meta-Analysis. Pediatrics 150, e2022057092O (2022).
Vetcho, S., Cooke, M. & Ullman, A. J. Family-centred care in dedicated neonatal units: an integrative review of international perspectives. J. Neonatal Nurs. 26, 73–92 (2020).
Tugwell, P. et al. Omeract: an international initiative to improve outcome measurement in rheumatology. Trials 8, 38 (2007).
Fink, E. L. et al. A core outcome set for pediatric critical care. Crit. Care Med. 48, 1819–1828 (2020).
Henry, C. J. et al. Neonatal sepsis: a systematic review of core outcomes from randomised clinical trials. Pediatr. Res. 91, 735–742 (2022).
Gallagher, K., Chant, K., Mancini, A., Bluebond-Langner, M. & Marlow, N. The neopace study: study protocol for the development of a core outcome set for neonatal palliative care. BMC Palliat. Care 22, 203 (2023).
Funding
This work was partially funded by the Republic of Turkey Ministry of National Education. The first author, Cansel Kocakabak, received a PhD studentship of the Republic of Turkey Ministry of National Education.
Author information
Authors and Affiliations
Contributions
A.v.d.H. and J.M.L. designed the review protocol. M.R. devised the search strategies for each database and ran the searches. C.K., M.S., A.v.d.H., J.M.L., M.C.Y., and J.K. screened articles to be included in the review. C.K., A.v.d.H., and J.M.L. performed the data synthesis. A.A., J.K., M.C.Y., M.S., and P.S. checked and confirmed the data synthesis. C.K., A.v.d.H., J.M.L., and P.S. drafted the first manuscript. A.A., J.K., M.C.Y., M.S. contributed to revised manuscript versions. All authors agreed on the final manuscript version and agreed to be accountable for the work reported in the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kocakabak, C., van den Hoogen, A., Rothfus, M. et al. Identifying outcomes and outcome measures in neonatal family-centered care trials: a systematic review. Pediatr Res 97, 56–66 (2025). https://doi.org/10.1038/s41390-024-03293-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03293-2
This article is cited by
-
Nurturing compassion in neonatal end-of-life care: a qualitative exploration of palliative care nurses’ roles and experiences
BMC Nursing (2025)
-
Family-centred care as a mediator in the relationship between parental nurse support and parental stress in neonatal intensive care units
BMC Nursing (2024)