Abstract
Background
Childhood obesity is a global public health issue, and the status of clinical practice guidelines (CPGs) as instruction manuals for the management of childhood obesity remains unclear. This study aims to identify and apprise the methodological and reporting quality of CPGs focused on childhood obesity and provide an overview of key recommendations.
Methods
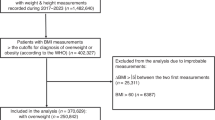
Databases and websites reporting guidelines were searched from January, 2018 to September, 2023. The methodological quality was graded using the AGREE II, and RIGHT was used to assess the reporting completeness.
Results
Among the six included CPGs, two were rated as high quality and considered “Recommended” and three were reported no less than 80%. CPGs included 184 recommendations cover diagnosis, assessment and management of complications, interventions and prevention. The diagnostic criteria for children with obesity over 2 years of age are based on normative BMI percentiles, depending on sex and age. CPGs recommended the delivery of multi-component behavior-changed interventions included controlling diet and increasing physical activity. Pharmacological interventions and bariatric surgery are considered as complementary therapies.
Conclusion
CPGs for childhood obesity should emphasize the impact of psychological factors and consider the provision of interventions from multiple settings, and could consider the role of complementary alternative therapies.
Impact
-
Six guidelines have been published in the past 5 years focusing children obesity.
-
Recommendations covered diagnosis, multiple intervention and prevention.
-
Guidelines should focus on the role of complementary alternative therapies.
-
Guidelines should emphasize the impact of psychological factors.
-
Guidelines should consider the provision of interventions from multiple settings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data are provided in the article and the Electronic Supplementary Material.
References
Pan, X. F., Wang, L. & Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 9, 373–392 (2021).
Hu, K. & Staiano, A. E. Trends in obesity prevalence among children and adolescents aged 2 to 19 years in the US from 2011 to 2020. JAMA Pediatr. 176, 1037–1039 (2022).
Osei Bonsu, E. & Addo, I. Y. Prevalence and correlates of overweight and obesity among under-five children in Egypt. Front. Public Health 10, 1067522 (2022).
World Health Organization. WHO European Regional Obesity Report 2022 (World Health Organization, 2022).
Buoncristiano, M. et al. Childhood overweight and obesity in Europe: changes from 2007 to 2017. Obes. Rev. 22, e13226 (2021).
Lister, N. B. et al. Child and adolescent obesity. Nat. Rev. Dis. Prim. 9, 24 (2023).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
World Health Organization. Obesity. https://www.who.int/health-topics/obesity#tab=tab_1 (2019).
Mei, Z. et al. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am. J. Clin. Nutr. 75, 978–985 (2002).
World Health Organization. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad hoc Working Group on Science and Evidence for Ending Childhood Obesity (World Health Organization, 2016).
Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. et al. Clinical Practice Guidelines We Can Trust (National Academies Press, 2011).
Gooey, M. et al. Clinical practice guidelines for the prevention of childhood obesity: a systematic review of quality and content. Obes. Rev. 23, e13492 (2022).
Tully, L. et al. Guidelines for treating child and adolescent obesity: a systematic review. Front. Nutr. 9, 902865 (2022).
Tian, C. et al. Barriers and strategies of clinical practice guideline implementation in China: aggregated analysis of 16 cross-sectional surveys. J. Public Health 1–14 (2023). Online ahead of print.
Mathew, A. & Clase, C. M. Conflicts of interest and the trustworthiness of clinical practice guidelines. Clin. J. Am. Soc. Nephrol. 17, 771–773 (2022).
Chen, Y., Wang, C., Shang, H., Yang, K. & Norris, S. L. Clinical practice guidelines in China. BMJ 360, j5158 (2018).
Shekelle, P. G. et al. Validity of the Agency for Healthcare Research and Quality clinical practice guidelines: how quickly do guidelines become outdated? JAMA 286, 1461–1467 (2001).
Shojania, K. G. et al. How quickly do systematic reviews go out of date? A survival analysis. Ann. Intern. Med. 147, 224–233 (2007).
Miake-Lye, I. M., Hempel, S., Shanman, R. & Shekelle, P. G. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst. Rev. 5, 28 (2016).
Hajizadeh, A. et al. Recommendation mapping of the World Health Organization’s guidelines on tuberculosis: a new approach to digitizing and presenting recommendations. J. Clin. Epidemiol. 134, 138–149 (2021).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Johnston, A., Kelly, S. E., Hsieh, S. C., Skidmore, B. & Wells, G. A. Systematic reviews of clinical practice guidelines: a methodological guide. J. Clin. Epidemiol. 108, 64–76 (2019).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 5, 210 (2016).
Brouwers, M. C. et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 182, E839–E842 (2010).
Brouwers, M. et al. Appraisal of Guidelines for Research & Evaluation II. https://www.agreetrust.org/wp‐content/uploads/2017/12/AGREE‐II‐Users‐Manual‐and‐23‐item‐Instrument‐2009‐Update‐2017.pdf (2017).
Chen, Y. et al. A reporting tool for practice guidelines in health care: the RIGHT statement. Ann. Intern. Med. 166, 128–132 (2017).
Kramer, M. S. & Feinstein, A. R. Clinical biostatistics. LIV. The biostatistics of concordance. Clin. Pharmacol. Ther. 29, 111–123 (1981).
Ríos, E. et al. Evaluation of the quality of clinical practice guidelines for the management of esophageal or gastric variceal bleeding. Eur. J. Gastroenterol. Hepatol. 26, 422–431 (2014).
Santesso, N., Wiercioch, W., Barbara, A. M., Dietl, H. & Schünemann, H. J. Focus groups and interviews with the public led to the development of a template for a GRADE Plain Language Recommendation (PLR). J. Clin. Epidemiol. 141, 18–25 (2022).
American Psychological Association. Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescents (American Psychological Association, 2018).
Henry, B. W., Ziegler, J., Parrott, J. S. & Handu, D. Pediatric weight management evidence-based practice guidelines: components and contexts of interventions. J. Acad. Nutr. Diet. 118, 1301–1311.e23 (2018).
Hampl, S. E. et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 151, e2022060640 (2023).
Valerio, G. et al. Diagnosis, treatment and prevention of pediatric obesity: consensus position statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics. Ital. J. Pediatr. 44, 88 (2018).
Yi, D. Y. et al. Clinical practice guideline for the diagnosis and treatment of pediatric obesity: recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition. Korean J. Pediatr. 62, 3–21 (2019).
National Institute for Health and Care Excellence. Obesity: Identification, Assessment and Management (National Institute for Health and Care Excellence (NICE), 2023).
Ojeda-Rodríguez, A. et al. Improved diet quality and nutrient adequacy in children and adolescents with abdominal obesity after a lifestyle intervention. Nutrients 10, 1500 (2018).
Puder, J. J. & Munsch, S. Psychological correlates of childhood obesity. Int. J. Obes. 34, S37–S43 (2010).
Smith, J. D., Fu, E. & Kobayashi, M. A. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu. Rev. Clin. Psychol. 16, 351–378 (2020).
Anderson, S. E., Sacker, A., Whitaker, R. C. & Kelly, Y. Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study. Int. J. Obes. 41, 1459–1466 (2017).
Schlam, T. R., Wilson, N. L., Shoda, Y., Mischel, W. & Ayduk, O. Preschoolers’ delay of gratification predicts their body mass 30 years later. J. Pediatr. 162, 90–93 (2013).
Styne, D. M. et al. Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 102, 709–757 (2017).
Harrison, K. et al. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: the Six-Cs model. Child. Dev. Perspect. 5, 50–58 (2011).
Reinehr, T. Lifestyle intervention in childhood obesity: changes and challenges. Nat. Rev. Endocrinol. 9, 607–614 (2013).
Grant-Guimaraes, J., Feinstein, R., Laber, E. & Kosoy, J. Childhood overweight and obesity. Gastroenterol. Clin. North. Am. 45, 715–728 (2016).
Barnett, S. J. et al. Long-term follow-up and the role of surgery in adolescents with morbid obesity. Surg. Obes. Relat. Dis. 1, 394–398 (2005).
Melstrom, L. G. et al. Adenocarcinoma of the gastroesophageal junction after bariatric surgery. Am. J. Surg. 196, 135–138 (2008).
Sui, Y. et al. A systematic review on use of Chinese medicine and acupuncture for treatment of obesity. Obes. Rev. 13, 409–430 (2012).
Guo, T. et al. Acupoint catgut embedding for obesity: systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2015, 401914 (2015).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926 (2008).
Sarkies, M. N., Jones, L. K., Gidding, S. S. & Watts, G. F. Improving clinical practice guidelines with implementation science. Nat. Rev. Cardiol. 19, 3–4 (2022).
Tian, C. et al. The effects of exercise on insomnia disorders: an umbrella review and network meta-analysis. Sleep Med. 115, 66–75 (2024).
Author information
Authors and Affiliations
Contributions
C.T. and M.X. was responsible for development of the search strategy and did the systematic searches. Y.Y.W. and B.T. screened titles and abstracts. C.T., H.H.L., Y.L. and M.Y.S. screened full text. C.T. and M.X. extracted data. C.T., H.H.L., M.Y.S. and Y.W. did the AGREE II and RIGHT assessment. L.G. provided methodological support. F.Y.N. and J.W. provided clinical guidance. C.T. wrote the manuscript, and Q.L. and L.G. revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical approval information, institution(s) and number(s)
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tian, C., Xu, M., Lai, H. et al. Management for children and adolescents with overweight and obesity: a recommendations mapping. Pediatr Res 97, 92–98 (2025). https://doi.org/10.1038/s41390-024-03357-3
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03357-3


