Abstract
Background
To characterize a cohort of ventilator-dependent infants and children with bronchopulmonary dysplasia-associated pulmonary hypertension (BPD-PH) and to describe their cardiorespiratory outcomes.
Methods
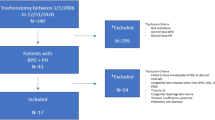
Subjects with BPD on chronic home ventilation were recruited from outpatient clinics. PH was defined by its presence on ≥1 cardiac catheterization or echocardiogram on or after 36 weeks post-menstrual age. Kaplan–Meier analysis was used to compare the timing of key events.
Results
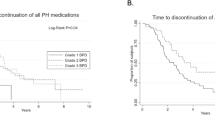
Of the 154 subjects, 93 (60.4%) had PH and of those, 52 (55.9%) required PH-specific medications. The ages at tracheostomy, transition to home ventilator, and hospital discharge were older in those with PH. Most subjects were weaned off oxygen and liberated from the ventilator by 5 years of age, which did not occur later in subjects with PH. The mortality rate after initial discharge was 2.6%.
Conclusions
The majority of infants with BPD-PH receiving chronic invasive ventilation at home survived after initial discharge. Subjects with BPD-PH improved over time as evidenced by weaning off oxygen and PH medications, ventilator liberation, and tracheostomy decannulation. While the presence of PH was not associated with later ventilator liberation or decannulation, the use of PH medications may be a marker of a more protracted disease trajectory.
Impact statement
-
There is limited data on long-term outcomes of children with bronchopulmonary dysplasia (BPD) who receive chronic invasive ventilation at home, and no data on those with the comorbidity of pulmonary hypertension (PH).
-
Almost all subjects with BPD-PH who were on chronic invasive ventilation at home survived after their initial hospital discharge.
-
Subjects with BPD-PH improved over time as evidenced by weaning off oxygen, PH medications, liberation from the ventilator, and tracheostomy decannulation.
-
The presence of PH did not result in later ventilator liberation or decannulation; however, the use of outpatient PH medications was associated with later ventilation liberation and decannulation.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The data that support the findings of this study are available from the BPD Collaborative but restrictions apply to the availability of these data, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the BPD Collaborative.
References
Northway, W. H. Jr, Rosan, R. C. & Porter, D. Y. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N. Engl. J. Med. 276, 357–368 (1967).
Malloy, K. W. & Austin, E. D. Pulmonary hypertension in the child with bronchopulmonary dysplasia. Pediatr. Pulmonol. 56, 3546–3556 (2021).
Mourani, P. M. & Abman, S. H. Pulmonary vascular disease in bronchopulmonary dysplasia: pulmonary hypertension and beyond. Curr. Opin. Pediatrics 25, 329–337 (2013).
Bhat, R., Salas, A. A., Foster, C., Carlo, W. A. & Ambalavanan, N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics 129, e682–689, (2012).
Mirza, H. et al. Pulmonary hypertension in preterm infants: prevalence and association with bronchopulmonary dysplasia. J. Pediatrics 165, 909–914 e901 (2014).
Mourani, P. M. et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. https://doi.org/10.1164/rccm.201409-1594OC (2014).
Arjaans, S. et al. Identification of gaps in the current knowledge on pulmonary hypertension in extremely preterm infants: a systematic review and meta-analysis. Paediatr. Perinat. Epidemiol. 32, 258–267 (2018).
Lagatta, J. M. et al. The impact of pulmonary hypertension in preterm infants with severe bronchopulmonary dysplasia through 1 Year. J. Pediatrics 203, 218–224.e213 (2018).
Altit, G., Bhombal, S., Hopper, R. K., Tacy, T. A. & Feinstein, J. Death or resolution: the “natural history” of pulmonary hypertension in bronchopulmonary dysplasia. J. Perinatol. 39, 415–425 (2019).
Khemani, E. et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics 120, 1260–1269 (2007).
Arjaans, S. et al. Fate of pulmonary hypertension associated with bronchopulmonary dysplasia beyond 36 weeks postmenstrual age. Arch. Dis. Child. Fetal Neonatal Ed. 106, 45–50 (2021).
Guaman, M. C. et al. Invasive mechanical ventilation at 36 weeks post-menstrual age, adverse outcomes with a comparison of recent definitions of bronchopulmonary dysplasia. J. Perinatol. 41, 1936–1942 (2021).
Murthy, K. et al. Inter-center variation in death or tracheostomy placement in infants with severe bronchopulmonary dysplasia. J. Perinatol. 37, 723–727 (2017).
Manimtim, W. M. et al. Respiratory outcomes for ventilator-dependent children with bronchopulmonary dysplasia. Pediatrics 151, https://doi.org/10.1542/peds.2022-060651 (2023).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Oken, E., Kleinman, K. P., Rich-Edwards, J. & Gillman, M. W. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatrics 3, 6 (2003).
Wu, K. Y. et al. Characterization of disease phenotype in very preterm infants with severe bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 201, 1398–1406 (2020).
Abman, S. H. et al. Characterisation of paediatric pulmonary hypertensive vascular disease from the PPHNet Registry. Eur. Respir. J 59, https://doi.org/10.1183/13993003.03337-2020 (2022).
Yung, D. et al. A multidisciplinary approach to severe bronchopulmonary dysplasia is associated with resolution of pulmonary hypertension. Front. Pediatr. 11, 1077422 (2023).
Mirza, H., Mandell, E. W., Kinsella, J. P., McNamara, P. J. & Abman, S. H. Pulmonary vascular phenotypes of prematurity: the path to precision medicine. J. Pediatrics 259, 113444 (2023).
Arjaans, S. et al. Clinical significance of early pulmonary hypertension in preterm infants. J. Pediatrics 251, 74–81.e73 (2022).
Akangire, G. et al. Outcomes of infants with severe bronchopulmonary dysplasia who received tracheostomy and home ventilation. Pediatr. Pulmonol. 58, 753–762 (2023).
Cristea, A. I., Carroll, A. E., Davis, S. D., Swigonski, N. L. & Ackerman, V. L. Outcomes of children with severe bronchopulmonary dysplasia who were ventilator dependent at home. Pediatrics 132, e727–734, (2013).
House, M., Nathan, A., Bhuiyan, M. A. N. & Ahlfeld, S. K. Morbidity and respiratory outcomes in infants requiring tracheostomy for severe bronchopulmonary dysplasia. Pediatr. Pulmonol. 56, 2589–2596 (2021).
Upadhyay, K., Vallarino, D. A. & Talati, A. J. Outcomes of neonates with tracheostomy secondary to bronchopulmonary dysplasia. BMC Pediatrics 20, 414 (2020).
Hansen, T. P. et al. A multidisciplinary chronic lung disease team in a neonatal intensive care unit is associated with increased survival to discharge of infants with tracheostomy. J. Perinatol. 41, 1963–1971 (2021).
Akangire, G. & Manimtim, W. Tracheostomy in infants with severe bronchopulmonary dysplasia: a review. Front. Pediatr. 10, 1066367 (2022).
Gibbs, K., Jensen, E. A., Alexiou, S., Munson, D. & Zhang, H. Ventilation strategies in severe bronchopulmonary dysplasia. Neoreviews 21, e226–e237 (2020).
Kielt, M. J. et al. Classifying multicenter approaches to invasive mechanical ventilation for infants with bronchopulmonary dysplasia using hierarchical clustering analysis. Pediatr. Pulmonol. 58, 2323–2332 (2023).
Gentle, S. J. et al. Intermittent hypoxemia and bronchopulmonary dysplasia with pulmonary hypertension in preterm infants. Am. J. Respir. Crit. Care Med. 207, 899–907 (2023).
Mahgoub, L. et al. Pulmonary vein stenosis of ex-premature infants with pulmonary hypertension and bronchopulmonary dysplasia, epidemiology, and survival from a multicenter cohort. Pediatr. Pulmonol. 52, 1063–1070 (2017).
Mourani, P. M., Ivy, D. D., Rosenberg, A. A., Fagan, T. E. & Abman, S. H. Left ventricular diastolic dysfunction in bronchopulmonary dysplasia. J. Pediatrics 152, 291–293 (2008).
Goss, K. N. et al. Early pulmonary vascular disease in young adults born preterm. Am. J. Respir. Crit. Care Med. 198, 1549–1558 (2018).
Collaco, J. M. et al. Characteristics of infants or children presenting to outpatient bronchopulmonary dysplasia clinics in the United States. Pediatric Pulmonol. https://doi.org/10.1002/ppul.25332 (2021).
Author information
Authors and Affiliations
Contributions
Contributions to conception and design, analysis, and interpretation of data: Gangaram G. Akangire, Winston Manimtim, Amit Agarwal, Stamatia Alexiou, Steven H. Abman, Sharon A. McGrath-Morrow, Joseph M. Collaco; Acquisition of data: Gangaram G. Akangire, Winston Manimtim, Amit Agarwal, Stamatia Alexiou, Brianna C. Aoyama, Eric D. Austin, Manvi Bansal, Julie L. Fierro, Lystra P. Hayden, Jacob A. Kaslow, Khanh V. Lai, Jonathan C. Levin, Audrey N. Miller, Jessica L. Rice, Michael C. Tracy, Steven H. Abman, Sharon A. McGrath-Morrow, Joseph M. Collaco; Drafting the manuscript: Gangaram G. Akangire, Winston Manimtim, Joseph M. Collaco; Revising manuscript critically for intellectual content and final approval for version to be published: Gangaram G. Akangire, Winston Manimtim, Amit Agarwal, Stamatia Alexiou, Brianna C. Aoyama, Eric D. Austin, Manvi Bansal, Julie L. Fierro, Lystra P. Hayden, Jacob A. Kaslow, Khanh V. Lai, Jonathan C. Levin, Audrey N. Miller, Jessica L. Rice, Michael C. Tracy, Christopher D. Baker, Sarah E. Bauer, A. Ioana Cristea, Sara K. Dawson, Laurie Eldredge, Jennifer K. Henningfeld, Robin L. McKinney, Roopa Siddaiah, Natalie M. Villafranco, Steven H. Abman, Sharon A. McGrath-Morrow, Joseph M. Collaco.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patient consent was required and obtained per local institutional IRBs.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akangire, G.G., Manimtim, W., Agarwal, A. et al. Outcomes of infants and children with bronchopulmonary dysplasia-associated pulmonary hypertension who required home ventilation. Pediatr Res 97, 387–394 (2025). https://doi.org/10.1038/s41390-024-03495-8
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03495-8
This article is cited by
-
Toward precision for bronchopulmonary dysplasia: Moving past current definitions
Journal of Perinatology (2026)
-
Home is where the right ventricle lives: bronchopulmonary dysplasia-associated pulmonary hypertension and home ventilation
Pediatric Research (2025)