Abstract
Background
While endogenous sex hormones (e.g., testosterone, estradiol) are important factors regulating adipose tissue distribution, studies evaluating such relationships in youth across a wide weight status spectrum are limited.
Methods
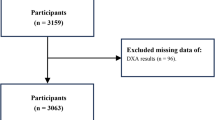
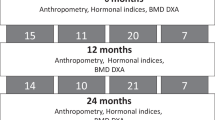
We performed a cross-sectional analysis of 8–21-year-old youth. Multiple linear regression models were used to evaluate associations between sex hormones and adiposity measures (android/gynoid ratio (A/G), total fat mass (FM), visceral adipose tissue (VAT), waist circumference (WC)) and total lean mass (LM), adjusting for pubertal stage and race/ethnicity, and stratified by sex and weight status.
Results
Among 342 youth, the mean age was 13.0 ± 2.8 years old (52.6% female; 38.9% normal weight [NW]; 27.8% overweight/obesity [OW/OB]; 33.3% severe obesity [SO]). Testosterone was positively associated with LM among males with NW (1462 g, 95% CI: 255–2668 g) and OW/OB (3792 g, 95% CI: 1244–6340 g), with A/G and WC among males with NW (0.01, 95% CI: 0–0.2 and 10 mm, 95% CI: 4–16 mm, respectively), and negatively associated with WC among males with SO (−43 mm, −81 to −5 mm). Estradiol was positively associated with A/G, FM, and WC among males with SO, and VAT in females with NW.
Conclusion
Our findings showed that sex hormones were associated with adipose tissue deposition in youth across the weight spectrum.
Impact statement
-
Sex hormones (e.g., testosterone, estradiol) are associated with various adiposity measures among male and female children and adolescents across a weight status spectrum.
-
We evaluated associations between sex hormones and various adiposity measures among 8–21-year-olds across a weight status spectrum (normal weight, overweight/class 1 obesity, class 2–3 obesity). We found that estradiol was positively associated with total fat mass, android/gynoid ratio, and waist circumference in males with class 2–3 obesity, and testosterone was positively associated with lean mass in males with normal weight and overweight/class 1 obesity.
-
Sex hormones may influence, or may be influenced by, adiposity in youth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Owing to the language used in the parental consent forms for this study regarding data sharing, the datasets cannot be shared externally.
References
Jebeile, H., Kelly, A. S., O’Malley, G. & Baur, L. A. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diab. Endocrinol. 10, 351–365 (2022).
Loomba-Albrecht, L. A. & Styne, D. M. Effect of puberty on body composition. Curr. Opin. Endocrinol. Diab. Obes. 16, 10–15 (2009).
Guo, S. S., Wu, W., Chumlea, W. C. & Roche, A. F. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am. J. Clin. Nutr. 76, 653–658 (2002).
Mittal, B. Subcutaneous adipose tissue & visceral adipose tissue. Indian J. Med. Res. 149, 571–573 (2019).
Kelly, A. S. et al. Reaching the tipping point: identification of thresholds at which visceral adipose tissue may steeply increase in youth. Obesity 28, 139–145 (2020).
Syme, C. et al. Intra-abdominal adiposity and individual components of the metabolic syndrome in adolescence. Arch. Pediatr. Adolesc. Med. 162, 453 (2008).
Taksali, S. E. et al. High visceral and low abdominal subcutaneous fat stores in the obese adolescent: a determinant of an adverse metabolic phenotype. Diabetes 57, 367–371 (2008).
Mathieu, P., Poirier, P., Pibarot, P., Lemieux, I. & DespréS, J.-P. Visceral obesity. Hypertension 53, 577–584 (2009).
Fox, C. S. et al. Abdominal visceral and subcutaneous adipose tissue compartments. Circulation 116, 39–48 (2007).
Navarro, G., Allard, C., Xu, W. & Mauvais‐Jarvis, F. The role of androgens in metabolism, obesity, and diabetes in males and females. Obesity 23, 713–719 (2015).
Mauvais-Jarvis, F., Clegg, D. J. & Hevener, A. L. The role of estrogens in control of energy balance and glucose homeostasis. Endocr. Rev. 34, 309–338 (2013).
Steiner, B. M. & Berry, D. C. The regulation of adipose tissue health by estrogens. Front. Endocrinol. 13, 889923 (2022).
Mongraw-Chaffin, M. L. et al. Association between sex hormones and adiposity: qualitative differences in women and men in the multi-ethnic study of atherosclerosis. J. Clin. Endocrinol. Metab. 100, E596–E600 (2015).
Ciardullo, S. et al. Differential association of sex hormones with metabolic parameters and body composition in men and women from the United States. J. Clin. Med. 12, 4783 (2023).
Vigil, P., Meléndez, J., Petkovic, G. & Del Río, J. P. The importance of estradiol for body weight regulation in women. Front. Endocrinol. 13, 951186 (2022).
Kelly, D. M. & Jones, T. H. Testosterone and obesity. Obes. Rev. 16, 581–606 (2015).
Yuxin, L. et al. Research progress on the relationship between obesity-inflammation-aromatase axis and male infertility. Oxid. Med. Cell. Longev. 2021, 1–7 (2021).
Fyfe‐Johnson, A. L. et al. Ideal cardiovascular health and adiposity: implications in youth. J. Am. Heart Assoc. 7, e007467 (2018).
Kuczmarski, R. J. et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 11, 1–190 (2002).
Wei, R., Ogden, C. L., Parsons, V. L., Freedman, D. S. & Hales, C. M. A method for calculating BMI z-scores and percentiles above the 95(Th) percentile of the CDC growth charts. Ann. Hum. Biol. 47, 514–521 (2020).
Kelly, A. S. et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches. Circulation 128, 1689–1712 (2013).
Kaul, S. et al. Dual-energy X-ray absorptiometry for quantification of visceral Fat. Obesity 20, 1313–1318 (2012).
Bosch, T. A. et al. Abdominal body composition differences in Nfl football players. J. Strength Cond. Res. 28, 3313–3319 (2014).
Irby, D. J. et al. Approaches to handling missing or “problematic” pharmacology data: Pharmacokinetics. CPT: Pharmacomet. Syst. Pharmacol. 10, 291–308 (2021).
Bomberg, E. M., Addo, O. Y., Sarafoglou, K. & Miller, B. S. Adjusting for pubertal status reduces overweight and obesity prevalence in the United States. J. Pediatr. 231, 200–206.e201 (2021).
Kim, C., Harrall, K. K., Glueck, D. H. & Dabelea, D. Sex steroids and adiposity in a prospective observational cohort of youth. Obes. Sci. Pract. 7, 432–440 (2021).
Loh, N. Y. et al. Sex hormones, adiposity, and metabolic traits in men and women: a Mendelian randomisation study. Eur. J. Endocrinol. 186, 407–416 (2022).
Gallo, M. F., Lopez, L. M., Grimes, D. A., Schulz, K. F. & Helmerhorst, F. M. Combination contraceptives: effects on weight. Cochrane Database Syst. Rev. 2014, Cd003987 (2014).
Nokoff, N. J. in Endotext (Feingold, K. R. et al. eds.) (MDText.com, Inc. Copyright©2000–2023, MDText.com, Inc., 2000).
Klaver, M. et al. Early hormonal treatment affects body composition and body shape in young transgender adolescents. J. Sex. Med. 15, 251–260 (2018).
Schagen, S. E., Cohen-Kettenis, P. T., Delemarre-van de Waal, H. A. & Hannema, S. E. Efficacy and safety of gonadotropin-releasing hormone agonist treatment to suppress puberty in gender dysphoric adolescents. J. Sex. Med. 13, 1125–1132 (2016).
Rosenfield, R. L. Normal and premature adrenarche. Endocr. Rev. 42, 783–814 (2021).
Acknowledgements
The authors would like to thank the individuals who participated in the parent research study from which these analyses were obtained. We also thank Ms. Rebecca Freese for statistical consulting.
Funding
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH) under award number R01 HL110957 (A.S.K.), and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the NIH under award number K23 DK125668 (E.M.B.). Additional support was provided by the NIH National Center for Advancing Translational Sciences (NCATS) under award number UL1TR002494, and an NIH NHLBI National Research Service Award (F32 HL127851-01; J.R.R.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
S.J.: Analysis and interpretation of data, Drafting the article, revising it critically for important intellectual content, Final approval of the version to be published. J.R.R.: Substantial contributions to conception and design, acquisition of data, revising it critically for important intellectual content, Final approval of the version to be published. A.S.K.: Substantial contributions to conception and design, acquisition of data, revising it critically for important intellectual content, Final approval of the version to be published. E.M.B.: Substantial contributions to conception and design, interpretation of data, revising it critically for important intellectual content, Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
E.M.B. has been a site principal investigator and is a site co-investigator for Novo Nordisk. J.R. receives donation of drug/placebo for Boehringer Ingelheim. A.S.K. serves as an unpaid consultant for Novo Nordisk, Vivus, Eli Lilly, and Boehringer Ingelheim as well as receives donated drug/placebo from Novo Nordisk and Vivus for National Institute of Diabetes, and Digestive, and Kidney Diseases-funded clinical trials. All authors have no relevant conflicts of interest to disclose related to this work.
Consent to participate
Consent/assent were obtained from parents/guardians and participants, respectively.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jang, S., Ryder, J.R., Kelly, A.S. et al. Association between endogenous sex hormones and adiposity in youth across a weight status spectrum. Pediatr Res 97, 1892–1899 (2025). https://doi.org/10.1038/s41390-024-03578-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03578-6