Abstract
Background
Echocardiography is the reference standard for diagnosing pulmonary hypertension (PH) and cardiac dysfunction (CD) in congenital diaphragmatic hernia (CDH). The use of an adjunct non-invasive biomarker would be invaluable. Plasma N-terminal brain Natriuretic Peptide (NT-proBNP) has been evaluated as a biomarker in CDH. Our objective was to investigate the utility of urinary NT-proBNP as an adjunct biomarker in CDH.
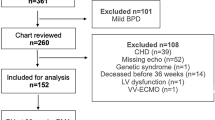
Methods
Prospective observational study of neonates with CDH. Urinary NT-proBNP and its ratio to urinary creatinine (UNBCR) were analyzed at 24 h of life (HOL). Spearman’s correlation was used to quantify the association between the urinary NT-proBNP with corresponding plasma concentrations. Logistic regression and receiver operating characteristic (ROC) curve analyses were used to examine urinary NT-proBNP and UNBCR’s association with need for ECMO. The Kruskal–Wallis test was used to compare urinary NT-proBNP concentrations with echocardiography parameters of PH and CD.
Results
Urinary NT-proBNP and UNBCR positively correlated with plasma concentrations. Patients with high right ventricular (RV) pressures had higher urinary NT-proBNP concentrations. Both urinary NT-proBNP and UNBCR concentrations increased with worsening left and right ventricular dysfunction on first postnatal echocardiogram.
Conclusion
We report the feasibility of urinary NT-proBNP as a non-invasive biomarker to assess PH and CD in CDH.
Impact statement
-
Non-invasive biomarkers are an important area of research in neonates as they have the potential to decrease the need for blood sampling, which may cause pain, stress, and induce iatrogenic anemia. Use of non-invasive biomarkers could be especially useful in congenital diaphragmatic hernia (CDH) who may need Extra-Corporeal Life Support (ECLS) for their management. We evaluated the potential utility of the urinary NT-proBNP in CDH. Plasma NT-proBNP has been studied in neonates with CDH; however, urinary NT-proBNP has not been explored, making this the first study to examine its potential as a biomarker.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this manuscript.
References
McGivern, M. R. et al. Epidemiology of congenital diaphragmatic hernia in Europe: a register-based study. Arch. Dis. Child Fetal Neonatal Ed. 100, F137–F144 (2015).
Pierro, M. & Thebaud, B. Understanding and treating pulmonary hypertension in congenital diaphragmatic hernia. Semin. Fetal Neonatal Med. 19, 357–363 (2014).
Patel, N. et al. Early postnatal ventricular dysfunction is associated with disease severity in patients with congenital diaphragmatic hernia. J. Pediatr. 203, 400–407 (2018).
Ferguson, D. M. et al. Early, postnatal pulmonary hypertension severity predicts inpatient outcomes in congenital diaphragmatic hernia. Neonatology 118, 147–154 (2021).
El-Khuffash, A. & Molloy, E. J. Are B-type natriuretic peptide (BNP) and N-terminal-pro-BNP useful in neonates? Arch. Dis. Child.-Fetal Neonatal Ed. 92, F320–F324 (2007).
Iliodromiti, Z. et al. Serum and urinary N-terminal pro-brain natriuretic peptides as biomarkers for bronchopulmonary dysplasia of preterm neonates. Front. Pediatr. 8, 588738 (2020).
Lammers, A. E., Hislop, A. A. & Haworth, S. G. Prognostic value of B-type natriuretic peptide in children with pulmonary hypertension. Int. J. Cardiol. 135, 21–26 (2009).
Reynolds, E. W. Brain-type natriuretic peptide in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatrics 114, 1297–1304 (2004).
Mine, K. et al. B‐type natriuretic peptide for assessment of haemodynamically significant patent ductus arteriosus in premature infants. Acta Paediatr. 102, e347–e352 (2013).
Kurihara, N. et al. Usefulness of measurement of urinary N-terminal pro-brain natriuretic peptide in neonatal period. Pediatr. Int. 53, 10–1111 (2011).
Celik, I. H., Erdeve, O., Demırel, G., Canpolat, F. E. & Dilmen, U. Elevated urinary NT-proBNP after pharmacological closure of patent ductus arteriosus in very low birth weight infants. Early Hum. Dev. 89, 187–189 (2013).
Khan, S. S. et al. Urinary NT-proBNP levels and echocardiographic parameters for patent ductus arteriosus. J. Perinatol. 37, 1319–1324 (2017).
Müller, N. et al. Perioperative urinary NT-ProBNP values and their usefulness as diagnostic and prognostic markers in children with congenital heart disease. Clin. Chim. Acta 518, 28–3219 (2021).
Naeem, B. et al. Urinary NT-proBNP as a potential noninvasive biomarker for screening of pulmonary hypertension in preterm infants: a pilot study. J. Perinatol. 40, 628–632 (2020).
Baptista, M. J. et al. N-terminal-pro-B type natriuretic peptide as a useful tool to evaluate pulmonary hypertension and cardiac function in CDH infants. Neonatology 94, 22–30 (2008).
Gupta, V. S. et al. Elevated proBNP levels are associated with disease severity, cardiac dysfunction, and mortality in congenital diaphragmatic hernia. J. Pediatr. Surg. 56, 1214–1219 (2021).
Heindel, K. et al. Early postnatal changes of circulating N-terminal-pro-B-type natriuretic peptide in neonates with congenital diaphragmatic hernia. Early Hum. Dev. 146, 105049 (2020).
Ruano, R. et al. Fetal lung volume and quantification of liver herniation by magnetic resonance imaging in isolated congenital diaphragmatic hernia. Ultrasound Obstet. Gynecol. 43, 662–669 (2014).
Gokulakrishnan, G. et al. Brain natriuretic peptide and N‐terminal brain natriuretic peptide for the diagnosis of haemodynamically significant patent ductus arteriosus in preterm neonates. Cochrane Database Syst. Rev. 12, CD013129 (2022).
Cortés, R. et al. Variability of NT‐proBNP plasma and urine levels in patients with stable heart failure: a 2‐year follow‐up study. Heart 93, 957 (2007).
Cortés, R. et al. Diagnostic and prognostic value of urine NT‐proBNP levels in heart failure patients. Eur. J. Heart Fail. 8, 621–627 (2006).
Reynen, S. et al. Urinary N‐terminal pro‐brain natriuretic peptide: prognostic value in patients with acute chest pain. ESC Heart Fail. 8, 2293–2305 (2021).
Abman, S. H. et al. Pediatric pulmonary hypertension: guidelines from the American Heart Association and American thoracic Society. Circulation 132, 2037–2099 (2015).
Christou, E. et al. Urinary NT-proBNP: a useful biomarker for the diagnosis of respiratory distress in the neonatal population. Cureus 15, e39019 (2023).
Patel, N., Massolo, A. C., Kraemer, U. S. & Kipfmueller, F. The heart in congenital diaphragmatic hernia: knowns, unknowns, and future priorities. Front. Pediatr. 10, 890422 (2022).
Bo, B. et al. Increased N-terminal Pro-B-Type natriuretic peptide during extracorporeal life support is associated with poor outcome in neonates with congenital diaphragmatic hernia. J. Pediatr. 241, 83–89 (2022).
Elgendy, M. M. et al. Acute kidney injury in infants diagnosed with congenital diaphragmatic hernia. Pediatr. Res. 94, 1083–1088 (2023).
Anwar, A., Ruffenach, G., Mahajan, A., Eghbali, M. & Umar, S. Novel biomarkers for pulmonary arterial hypertension. Respir. Res. 17, 1–0 (2016).
Warwick, G., Thomas, P. S. & Yates, D. H. Biomarkers in pulmonary hypertension. Eur. Respir. J. 32, 503–512 (2008).
Acknowledgements
We acknowledge the time, effort, and dedication of the Newborn Center Nursing staff in helping with timely sample collection and storage of patient samples for this project. This study was funded by the Evie Whitlock Funding for Fellows in Neonatal-Perinatal Medicine at Baylor College of Medicine.
Author information
Authors and Affiliations
Contributions
Srirupa Hari Gopal- Conceptualization, methodology, investigation, writing original draft, editing draft, funding acquisition, visualization; Kelly Frances Martinek-Investigation, data curation, review original draft; Judith Becker-Investigation, resources, review original draft; Nidhy Varghese- Resources, review original draft; Betul Yilmaz- Resources, review original draft; Joseph Hagan- Data curation, formal analysis, review original draft; Sharada H. Gowda- Resources, review original draft; Mohan Pammi- Methodology, Resources, review original draft; Sridevi Devaraj- Methodology, Resources, review original draft; Caraciolo J. Fernandes- Conceptualization, methodology, resources, supervision, and review of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Parental consent was required for this study and obtained following Institutional Review Board guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hari Gopal, S., Martinek, K.F., Vacher, C. et al. Utility of urinary NT-proBNP in congenital diaphragmatic hernia: a prospective pilot study. Pediatr Res 97, 2305–2311 (2025). https://doi.org/10.1038/s41390-024-03600-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03600-x
This article is cited by
-
Utility of NT-proBNP as a biomarker in Congenital Diaphragmatic Hernia
Pediatric Research (2025)
-
Incidence and risk factors of pulmonary hypertension in neonates with congenital diaphragmatic hernia: a systematic review and meta-analysis
Pediatric Surgery International (2025)