Abstract
Background
Preterm birth is a common cause of dystonia. Though dystonia is often associated with striatal dysfunction after neonatal brain injury, cortical dysfunction may best predict dystonia following preterm birth. Furthermore, abnormal sensorimotor cortex inhibition is associated with genetic and idiopathic dystonias. To investigate cortical dysfunction and dystonia following preterm birth, we developed a new model of preterm birth in mice.
Methods
We induced preterm birth in C57BL/6J mice at embryonic day 18.3, ~24 h early. Leg adduction variability and amplitude, metrics we have shown distinguish between dystonia from spasticity during gait in people with CP, were quantified from gait videos of mice. Parvalbumin-positive interneurons, the largest population of cortical inhibitory interneurons, were quantified in the sensorimotor cortex and striatum.
Results
Mice born preterm demonstrate increased leg adduction amplitude and variability during gait, suggestive of clinically observed dystonic gait features. Mice born preterm also demonstrate fewer parvalbumin-positive interneurons and reduced parvalbumin immunoreactivity in the sensorimotor cortex, but not the striatum, suggesting dysfunction of cortical inhibition.
Conclusions
These data may suggest an association between cortical dysfunction and dystonic gait features following preterm birth. We propose that our novel mouse model of preterm birth can be used to study this association.
Impact
-
Mouse models of true preterm birth are valuable for studying clinical complications of prematurity.
-
Mice born preterm demonstrate increased leg adduction amplitude and variability during gait, suggestive of clinically observed dystonic gait features.
-
Mice born preterm demonstrate fewer parvalbumin-positive interneurons and reduced parvalbumin immunoreactivity in the sensorimotor cortex, suggesting dysfunction of cortical inhibition.
-
Mice born preterm do not demonstrate changes in parvalbumin immunoreactivity in the striatum.
-
Cortical dysfunction may be associated with dystonic gait features following preterm birth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available from qualified investigators upon request.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Himmelmann, K. et al. Dyskinetic cerebral palsy in Europe: trends in prevalence and severity. Arch. Dis. Child 94, 921–926 (2009).
Steeves, T., Day, L., Dykeman, J., Jette, N. & Pringsheim, T. The prevalence of primary dystonia: a systematic review and meta-analysis. Mov. Disord. 27, 1789–1796 (2012).
Himmelmann, K. & Uvebrant, P. The panorama of cerebral palsy in Sweden part XII shows that patterns changed in the birth years 2007-2010. Comp. Study 107, 462–468 (2018).
Van Naarden Braun, K. et al. Birth prevalence of cerebral palsy: a population-based study. Pediatrics 137, 1–9 (2016).
Ueda, K., Aravamuthan, B. R. & Pearson, T. S. Dystonia in individuals with spastic cerebral palsy and isolated periventricular leukomalacia. Dev. Med. Child Neurol. 65, 94–99 (2023).
Chintalapati, K., Pearson, T. S., Ueda, K. & Aravamuthan, B. R. Brain region size differences associated with dystonia in people with cerebral palsy born premature. Pediatr. Neurol. 148, 8–13 (2023).
Albanese, A. et al. Phenomenology and classification of dystonia: a consensus update. Mov. Disord. 28, 863–873 (2013).
Sanger, T. D., Delgado, M. R., Gaebler-Spira, D., Hallett, M. & Mink, J. W. Classification and definition of disorders causing hypertonia in childhood. in Pediatrics vol. 111 e89–e97 (American Academy of Pediatrics, 2003).
Sanger, T. D. et al. Definition and classification of hyperkinetic movements in childhood. Mov. Disord. 25, 1538–1549 (2010).
Aravamuthan, B. R., Pearson, T. S., Chintalapati, K. & Ueda, K. Under-recognition of leg dystonia in people with cerebral palsy. Ann. Child Neurol. Soc. 1, 162–167 (2023).
Miao, H., Mathur, A. M. & Aravamuthan, B. R. Spasticity and dystonia are underidentified in young children at high risk for cerebral palsy. J. Child Neurol. 37, 105–111 (2022).
Bohn, E., Goren, K., Switzer, L., Falck-Ytter, Y. & Fehlings, D. Pharmacological and neurosurgical interventions for individuals with cerebral palsy and dystonia: a systematic review update and meta-analysis. Dev. Med. Child Neurol. 63, 1038–1050 (2021).
Clancy, B., Finlay, B. L., Darlington, R. B. & Anand, K. J. S. Extrapolating brain development from experimental species to humans. Neurotoxicology 28, 931–937 (2007).
Semple, B. D., Blomgren, K., Gimlin, K., Ferriero, D. M. & Noble-Haeusslein, L. J. Brain development in rodents and humans: Identifying benchmarks of maturation and vulnerability to injury across species. Prog. Neurobiol. 106–107, 1–16 (2013).
Mccarthy, R. et al. Mouse models of preterm birth: suggested assessment and reporting guidelines. Biol. Reprod. 99, 922–937 (2018).
Le Dieu-Lugon, B. et al. Why considering sexual differences is necessary when studying encephalopathy of prematurity through rodent models. Eur. J. Neurosci. 52, 2560–2574 (2020).
Chen, R. et al. Impact of gestational age on risk of cerebral palsy: unravelling the role of neonatal morbidity. Int J. Epidemiol. 50, 1852 (2021).
Boyle, C. A. et al. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics 127, 1034–1042 (2011).
Oleas, J., Yokoi, F., Deandrade, M. P., Pisani, A. & Li, Y. Engineering animal models of dystonia. Mov. Disord. 28, 990–1000 (2013).
Richter, F. & Richter, A. Genetic animal models of dystonia: common features and diversities. Prog. Neurobiol. 121, 91–113 (2014).
Tassone, A., Sciamanna, G., Bonsi, P., Martella, G. & Pisani, A. Experimental models of dystonia. Int. Rev. Neurobiol. 98, 551–572 (2011).
Aravamuthan, B. R. et al. Determinants of gait dystonia severity in cerebral palsy. Dev. Med. Child Neurol. 65, 968–977 (2023).
Aravamuthan, B. R. et al. Gait features of dystonia in cerebral palsy. Dev. Med. Child Neurol. 63, 748–754 (2021).
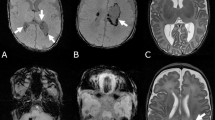
Aravamuthan, B. R. & Waugh, J. L. Localization of basal ganglia and thalamic damage in dyskinetic cerebral palsy. Pediatr. Neurol. 54, 11–21 (2016).
Chintalapati, K., Miao, H., Mathur, A., Neil, J. & Aravamuthan, B. R. Objective and clinically feasible analysis of diffusion MRI data can help predict dystonia after neonatal brain injury. Pediatr. Neurol. 118, 6–11 (2020).
Eskow Jaunarajs, K. L., Bonsi, P., Chesselet, M. F., Standaert, D. G. & Pisani, A. Striatal cholinergic dysfunction as a unifying theme in the pathophysiology of dystonia. Prog. Neurobiol. 127–128, 91–107 (2015).
Eskow Jaunarajs, K. L., Scarduzio, M., Ehrlich, M. E., Mcmahon, L. L. & Standaert, D. G. Diverse mechanisms lead to common dysfunction of striatal cholinergic interneurons in distinct genetic mouse models of Dystonia. J. Neurosci. 39, 7195–7205 (2019).
Bonsi, P. et al. Centrality of striatal cholinergic transmission in basal ganglia function. Front. Neuroanat. 5, 6 (2011).
Pappas, S. S. et al. Forebrain deletion of the dystonia protein torsinA causes dystonic-like movements and loss of striatal cholinergic neurons. Elife 4, 1–25 (2015).
Corp, D. T. et al. Network localization of cervical dystonia based on causal brain lesions. Brain 142, 1660 (2019).
Garibotto, V. et al. In vivo evidence for GABA(A) receptor changes in the sensorimotor system in primary dystonia. Mov. Disord. 26, 852–857 (2011).
Miocinovic, S., De Hemptinne, C., Qasim, S., Ostrem, J. L. & Starr, P. A. Patterns of cortical synchronization in isolated dystonia compared with Parkinson disease. JAMA Neurol. 72, 1244–1251 (2015).
Norris, S. A. et al. Regional, not global, functional connectivity contributes to isolated focal dystonia. Neurology 95, E2246–E2258 (2020).
Gallea, C. et al. Loss of inhibition in sensorimotor networks in focal hand dystonia. Neuroimage Clin. 17, 90–97 (2017).
Nahar, L., Delacroix, B. M. & Nam, H. W. The role of parvalbumin interneurons in neurotransmitter balance and neurological disease. Front. Psychiatry 12, 679960 (2021).
Lim, L., Mi, D., Llorca, A. & Marín, O. Development and functional diversification of cortical interneurons. Neuron 100, 294 (2018).
Tremblay, R., Lee, S. & Rudy, B. GABAergic interneurons in the neocortex: from cellular properties to circuits. Neuron 91, 260 (2016).
Juarez, P. & Martínez Cerdeño, V. Parvalbumin and parvalbumin chandelier interneurons in autism and other psychiatric disorders. Front. Psychiatry 13, 913550 (2022).
Jiang, X., Lachance, M. & Rossignol, E. Involvement of cortical fast-spiking parvalbumin-positive basket cells in epilepsy. Prog. Brain Res. 226, 81–126 (2016).
Påhlman, M., Gillberg, C. & Himmelmann, K. Autism and attention-deficit/hyperactivity disorder in children with cerebral palsy: high prevalence rates in a population-based study. Dev. Med. Child Neurol. 63, 320–327 (2021).
Dos Santos Rufino, A., Påhlman, M., Olsson, I. & Himmelmann, K. Characteristics and challenges of epilepsy in children with cerebral palsy-a population-based study. J. Clin. Med. 12, 346 (2023).
Hamann, M., Richter, A., Meillasson, F. V., Nitsch, C. & Ebert, U. Age-related changes in parvalbumin-positive interneurons in the striatum, but not in the sensorimotor cortex in dystonic brains of the dtsz mutant hamster. Brain Res. 1150, 190–199 (2007).
Morin, C. et al. The impact of mouse preterm birth induction by RU-486 on microglial activation and subsequent hypomyelination. Int. J. Mol. Sci. 23, 4867 (2022).
Bernard, N. et al. Continuation of pregnancy after first-trimester exposure to mifepristone: an observational prospective study. BJOG 120, 568–575 (2013).
Hill, N. C. W., Selinger, M., Ferguson, J. & Mackenzie, I. Z. The placental transfer of mifepristone (RU 486) during the second trimester and its influence upon maternal and fetal steroid concentrations. Br. J. Obstet. Gynaecol. 97, 406–411 (1990).
Nath, T. et al. Using DeepLabCut for 3D markerless pose estimation across species and behaviors. Nat. Protoc. 14, 2152–2176 (2019).
Mathis, A. et al. DeepLabCut: markerless pose estimation of user-defined body parts with deep learning. Nat. Neurosci. 21, 1281–1289 (2018).
Broom, L. et al. A translational approach to capture gait signatures of neurological disorders in mice and humans. Sci. Rep. 7, 1–17 (2017).
Brégou Bourgeois, A., Mariani, B., Aminian, K., Zambelli, P. Y. & Newman, C. J. Spatio-temporal gait analysis in children with cerebral palsy using, foot-worn inertial sensors. Gait Posture 39, 436–442 (2014).
Carcreff, L. et al. Comparison of gait characteristics between clinical and daily life settings in children with cerebral palsy. Sci. Rep. 10, 1–11 (2020).
Faul, F., Erdfelder, E., Lang, A.-G. & Buchner, A. GPOWER: a general power analysis program. Behav. Res. Methods 39, 175–191 (2007).
Vannucci, S. J. & Back, S. A. The Vannucci model of hypoxic-ischemic injury in the neonatal rodent: 40 years later. Dev. Neurosci. 44, 186–193 (2022).
Rice, J. E., Vannucci, R. C. & Brierley, J. B. The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann. Neurol. 9, 131–141 (1981).
Mcclelland, V. M. et al. Somatosensory evoked potentials and central motor conduction times in children with dystonia and their correlation with outcomes from deep brain stimulation of the globus pallidus internus. Clin. Neurophysiol. 129, 473–486 (2018).
Johnston, M. V. & Hagberg, H. Sex and the pathogenesis of cerebral palsy. Dev. Med. Child Neurol. 49, 74–78 (2007).
Jinnah, H. A. et al. Rodent models for dystonia research: characteristics, evaluation, and utility. Mov. Disord. 20, 283–292 (2005).
Chalard, A., Amarantini, D., Tisseyre, J., Marque, P. & Gasq, D. Spastic co-contraction is directly associated with altered cortical beta oscillations after stroke. Clin. Neurophysiol. 131, 1345–1353 (2020).
Gracies, J.-M. Pathophysiology of spastic paresis. II: emergence of muscle overactivity. Muscle Nerve 31, 552–571 (2005).
Funding
Funding supporting this work is from the National Institutes of Neurological Disorders and Stroke: 1K08NS117850-01A1 (BRA) and 1R01NS112234 (RG).
Author information
Authors and Affiliations
Contributions
Kat Gemperli helped design the study, contributed to data collection, carried out data analyses, and critically reviewed and revised the manuscript. Femi Folorunso, Ben Norin, Rebecca Joshua, Rachel Rykowski, and Clayton Hill: contributed to data collection, carried out data analyses, and critically reviewed and revised the manuscript. Rafael Galindo helped design the study, supervised data collection, and critically reviewed and revised the manuscript. Bhooma Aravamuthan conceptualized and designed the study, supervised data collection and analysis, drafted the initial manuscript, and critically reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gemperli, K., Folorunso, F., Norin, B. et al. Preterm birth is associated with dystonic features and reduced cortical parvalbumin immunoreactivity in mice. Pediatr Res 97, 2475–2484 (2025). https://doi.org/10.1038/s41390-024-03603-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03603-8