Abstract
Background
Investigate the utility of cardiovascular responses such as heart rate (HR), blood pressure (BP), and heart rate variability (HRV) in the prognosis of children with acute acquired brain injury (ABI).
Methods
Children under 18 years with severe acute acquired brain injury (ABI) who survived at least 12 h after PICU admission were included in a prospective observational cohort in a tertiary academic PICU. Physiological variables, neurological data, laboratory tests (chemistry and hematology), and medications were recorded within 12 h of admission. Linear and nonlinear HRV indices, CT scans, PICU scores, and survival rates were evaluated.
Results
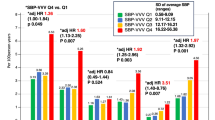
Seventy-two children, median age 10.7 years (IQR 4.1–13.6), were eligible for the study; 28 (38.9%) were diagnosed with brain death (BD). Tachycardia, SBP and MBP < 5th percentile, and MBP and DBP> 99th percentile were significantly associated with mortality. Poincaré SD1/SD2 was significantly associated with mortality after adjusting for age, sex and ongoing medication.
Conclusion
Tachycardia, systolic hypotension and median hypo and hypertension were associated to mortality in children with severe ABI. While further validation through larger, multicenter studies is necessary, the Poincaré SD1/SD2 ratio has shown promise as a prognostic tool for predicting mortality in children with severe ABI.
Impact statement
-
This study explores cardiovascular changes, including heart rate and blood pressure, and linear/nonlinear HRV measures using ECG at 1000 Hz, and compare them with other prognostic factors like brain tomography and PICU scores. Tachycardia, hypo/hypertension in the early hours after admission are linked to early mortality in children with severe traumatic and non-traumatic brain injury. Linear/non-linear measures of HRV were also related to survival. Higher HRV values indicating better survival chances. We identified Poincaré SD1/SD2 ratio as a promising tool for predicting mortality in children with severe ABI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Johnson, A. R., DeMatt, E. & Salorio, C. F. Predictors of outcome following acquired brain injury in children. Dev. Disabil. Res Rev. 15, 124–132 (2009).
Silva, M. J., Carneiro, B., Mota, R. & Baptista, M. J. Cardiovascular events in children with brain injury: A systematic review. Int. J. Cardiol. 387, 1–10 (2023).
Johnston, B. W., Barrett-Jolley, R., Krige, A. & Welters, I. D. Heart rate variability: Measurement and emerging use in critical care medicine. J. Intensive Care Soc. 21, 148–157 (2020).
Biswas, A. K., Scott, W. A. & Sommerauer, J. F. Heart rate variability after acute traumatic brain injury in children. Crit Care Med. 28, 3907–3912 (2000).
Francesco, B. et al. Linear and nonlinear heart rate variability indexes in clinical practice. Comput. Math Methods Med. 2012, 219080 (2012).
Sassi, R. et al. Advances in heart rate variability signal analysis: Joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace 17, 1341–1353 (2015).
Taralov, Z. Z., Terziyski, K. V. & Kostianev, S. S. Heart rate variability as a method for assessment of the autonomic nervous system and the adaptations to different physiological and pathological conditions. Folia Med. (Plovdiv.). 57, 173–180 (2015).
Martínez, J. P., Almeida, R., Olmos, S., Rocha, A. P. & Laguna, P. A Wavelet-based ECG delineator evaluation on standard databases. IEEE Trans. Biomed. Eng. 51, 570–581 (2004).
Martin, B., DeWitt, P. E., Albers, D. & Bennett, T. D. Development of a pediatric blood pressure percentile tool for clinical decision support. JAMA Netw. Open. 5, 10 (2022).
Fleming, S. et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: A systematic review of observational studies. Lancet 377, 1011–1018 (2011).
Pollack, M. M., Patel, K. M. & Ruttimann, U. E. PRISM III: An updated pediatric risk of mortality score. Crit. Care Med. 24, 743–752 (1996).
Casertano A. et al. An overview of hypoglycemia in children including a comprehensive practical diagnostic flowchart for clinical Use. Front Endocrinol (Lausanne) 12 (2021).
Balakrishnan, B. et al. GCS-pupil score has a stronger association with mortality and poor functional outcome than GCS alone in pediatric severe traumatic brain injury. Pediatr. Neurosurg. 56, 432–439 (2021).
Anjali, M. M. & Unnikrishnan, D. T. Effectiveness of PRISM III score in predicting the severity of illness and mortality of children admitted to pediatric intensive care unit: a cross-sectional study. Egypt. Pediatr. Assoc. Gaz. 71, 1–6 (2023).
Beslow, L. A. et al. Pediatric intracerebral hemorrhage score: a simple grading scale for intracerebral hemorrhage in children. Stroke 45, 66–70 (2014).
Ryu, J. A. et al. Prognostic value of computed tomography score in patients after extracorporeal cardiopulmonary resuscitation. Crit. Care. 22, 323 (2018).
Nakagawa, T. A. et al. Clinical report - Guidelines for the determination of brain death in infants and children: An update of the 1987 task force recommendations. Pediatrics 128, 2139–2155 (2011).
Gonçalves, H., Rocha, A. P., Ayres-De-Campos, D. & Bernardes, J. Internal versus external intrapartum foetal heart rate monitoring: The effect on linear and nonlinear parameters. Physiol. Meas. 27, 307–319 (2006).
Yentes, J. M. et al. The appropriate use of approximate entropy and sample entropy with short data sets. Ann. Biomed. Eng. 41, 349–365 (2013).
McCamley, J. D., Denton, W., Arnold, A., Raffalt, P. C. & Yentes, J. M. On the calculation of sample entropy using continuous and discrete human gait data. Entropy 20, 10 (2018).
Novak, V., Saul, J. P. & Eckberg, D. L. Task Force report on heart rate variability. Circulation 96, 1056–1057 (1997).
Hayes M. H. Statistical Digital Signal Processing and Modelling. (John Wiley & Sons, New York, 1996).
Richman, J. S. & Moorman, J. R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Physiol. Heart Circ. Physiol. 278, H2039–H2049 (2000).
Uzun, I. S., Asyali, M. H., Celebi, G. & Pehlivan, M. Nonlinear analysis of heart rate variability. Annu. Int. Conf. IEEE Eng. Med. Biol.-Proc. 2, 1581–1584 (2001).
Pincus, S. M. Approximate entropy as a measure of system complexity. Proc. Natl Acad. Sci. USA 88, 2297–2301 (1991).
Brasel, K., Guse, C., Gentilello, L. & Nirula, R. HR in TBI 2007 abstract. J. Trauma. 62, 812–817 (2007).
Reisner, A., Chen, X., Kumar, K. & Reifman, J. Prehospital heart rate and blood pressure increase the positive predictive value of the glasgow coma scale for high-mortality traumatic brain injury. J. Neurotrauma 31, 906–913 (2014).
Victorino, G. P., Battistella, F. D. & Wisner, D. H. Does tachycardia correlate with hypotension after trauma? J. Am. Coll. Surg. 196, 679–684 (2003).
Yao, S. H. W., Chong, S. L., James, V., Lee, K. P. & Ong, G. Y. K. Associations of initial haemodynamic profiles and neurological outcomes in children with traumatic brain injury: A secondary analysis. Emerg. Med. J. 39, 527–533 (2022).
Suttipongkaset, P. et al. Blood pressure thresholds and mortality in pediatric traumatic brain injury. Pediatrics 142, 2 (2018).
Erickson, S. L., Killien, E. Y., Wainwright, M., Mills, B. & Vavilala, M. S. Mean arterial pressure and discharge outcomes in severe pediatric traumatic brain injury. Neurocrit Care. 34, 1017–1025 (2021).
Freeman, A. D. et al. Does hypertension at initial presentation adversely affect outcomes in pediatric traumatic brain injury? J. Pediatr. Surg. 55, 702–706 (2020).
Lulla, A. et al. Prehospital guidelines for the management of traumatic brain injury.; 273rd Edition. Prehosp. Emerg. Care. 27, 507–538 (2023).
Lui, A., Kumar, K. K. & Grant, G. A. Management of severe traumatic brain injury in pediatric patients. Front. Toxicol. 24, 1–14 (2022).
Rapenne, T. et al. Could heart rate variability predict outcome in patients with severe head injury? A pilot study. J. Neurosurg. Anesthesiol. 13, 260–268 (2001).
Rapenne, T. et al. Could heart rate variability analysis become an early predictor of imminent brain death? A pilot study. Anesth. Analg. 91, 329–336 (2000).
Florez-Perdomo, W. A. et al. A systematic review and meta-analysis on effect of beta-blockers in severe traumatic brain injury. Neurol. Res. 43, 609–615 (2021).
Butera, G., Bonnet, D., Kachaner, J., Sidi, D. & Villain, E. Heart rate variability in children with hypertrophic cardiomyopathy. Heart 89, 205–206 (2003).
Bhogal, A. S. et al. Which heart rate variability index is an independent predictor of mortality in cirrhosis? Digestive Liver Dis. 51, 695–702 (2019).
Milecević, G. Low to high frequency ratio of heart rate variability spectra fails to describe sympatho-vagal balance in cardiac patients. Coll. Antropol. 29, 295–300 (2005).
Toichi, M., Sugiura, T., Murai, T. & Sengoku, A. A new method of assessing cardiac autonomic function and its comparison with spectral analysis and coefficient of variation of R-R interval. J. Auton. Nerv. Syst. 62, 79–84 (1997).
Guzik, P. et al. Correlations between the Poincaré plot and conventional heart rate variability parameters assessed during paced breathing. J. Physiol. Sci. 57, 63–71 (2007).
Piantino, J. A. et al. Early heart rate variability and electroencephalographic abnormalities in acutely brain-injured children who progress to brain death∗. Pediatr. Crit. Care Med. 20, 38–46 (2019).
Henriques, T. et al. Nonlinear methods most applied to heart-rate time series: A review. Entropy 22, 309 (2020).
Serafi, A. S. Heart rate variability rate (HRV) – analysis and clinical significance. Int. J. Biol. Biotech. 15, 193–199 (2018).
Kwon, O. et al. Electrocardiogram sampling frequency range acceptable for heart rate variability analysis. Health. Inf. Res. 24, 198–206 (2018).
Acknowledgements
A.P.R., partially supported by CMUP, member of LASI, which is financed by national funds through FCT—Fundação para a Ciência e a Tecnologia, I.P., under the projects with reference UIDB/00144/2020 and UIDP/00144/2020.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data—M.J.S.; H.G.; R.A.; C.C.D.; A.I.A.; C.G.; A.P.R.;I.A. Drafting the article or revising it critically for important intellectual content—M.J.S.; M.J.B.; C.G.; R.A.; H.G.; C.C.D. Final approval of the version to be published—M.J.S.; I.A.; C.G.; M.J.B.; A.P.R.; R.A.; C.C.D.; H.G.
Corresponding author
Ethics declarations
Competing interests
The authors whose names are listed immediately above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Silva, M.J., Gonçalves, H., Almeida, R. et al. Cardiovascular responses as predictors of mortality in children with acute brain injury. Pediatr Res 97, 2347–2353 (2025). https://doi.org/10.1038/s41390-024-03679-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03679-2