Abstract
Background
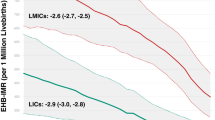
Limited data exist on population-level mortality outcomes related to extreme neonatal hyperbilirubinemia (EHB) and this study examines trends in annual infant mortality rate (IMR) attributed to hemolytic and perinatal jaundice among Germany, France, Italy, Portugal, Greece and Spain from 1990 to 2019.
Methods
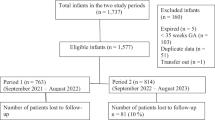
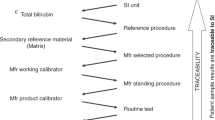
Data on annual incident cases and disability-adjusted life years were collected from the 2019 Global Burden of Disease study. Live birth cohort data were sourced from UN World Population Prospects. We quantified temporal trends, with relative percent changes. Average annual percent changes (AAPCs) were evaluated using the Joinpoint Regression Program.
Results
EHB-related infant mortality decreased from 21.4 (95%CI: 16.1, 27.1) in 1990 to 4.2 (95%CI: 1.9, 7.6) per million live births in 2019. Germany demonstrated lowest AAPC of –3.2% (95% CI: –3.8, –2.5), while Portugal had the highest AAPC of –8.6% (95% CI –11.9, –5.1) in reducing infant mortality due to EHB. There were distinct divergences in the trajectories of declining EHB mortality among the studied countries.
Conclusion
This study highlights a significant decline in infant mortality due to extreme hyperbilirubinemia, emphasizing the need for national surveillance and tailored guidelines to prevent bilirubin induced neurological damage.
Impact
-
This cross-sectional analysis revealed a marked decline in infant mortality rates attributed to extreme hyperbilirubinemia across the selected European countries.
-
The rates of decline varied significantly between countries, demonstrating notable heterogeneity in mortality trends when stratified by age at death.
-
Implementing data-driven surveillance systems can optimize the alignment of equitable healthcare services, strengthen accountability measures, and identify critical operational inefficiencies.
-
In the European Union, country-specific hyperbilirubinemia guidelines should be reinforced to ensure effective screening and post-discharge follow-up protocols that are tailored to risk burden and available healthcare resources.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All raw data were openly available from the Global Burden of Disease Results Tool (https://vizhub.healthdata.org/gbd-results/), Institute of Health Metrics and Evaluation, University of Washington, USA. Derived data supporting the findings of this study are available from the corresponding author [R.V] on request.
Change history
03 February 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41390-024-03791-3
References
Shapiro, S. M., Bhutani, V. K. & Johnson, L. Hyperbilirubinemia and kernicterus. Clin. Perinatol. 33, 387–410 (2006).
Johnson, L., Bhutani, V. K., Karp, K., Sivieri, E. M. & Shapiro, S. M. Clinical report from the pilot USA Kernicterus Registry (1992 to 2004). J. Perinatol. 29, S25–S45 (2009).
Kasirer, Y., Kaplan, M. & Hammerman, C. Kernicterus on the spectrum. Neoreviews 24, e329–e342 (2023).
Practice parameter: management of hyperbilirubinemia in the healthy term newborn. American Academy of Pediatrics. Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Pediatrics 94: 558–565. (1994).
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114, 297–316 (2004).
Maisels, M. J. et al. Hyperbilirubinemia in the newborn infant > or =35 weeks’ gestation: an update with clarifications. Pediatrics 124, 1193–1198 (2009).
Bhutani, V. K., Maisels, M. J., Stark, A. R. & Buonocore, G. Management of jaundice and prevention of severe neonatal hyperbilirubinemia in infants >or=35 weeks gestation. Neonatology 94, 63–67 (2008).
Rennie, J., Burman-Roy, S. & Murphy, M. S. Guideline Development Group. Neonatal jaundice: summary of NICE guidance. BMJ 340, c2409 (2010).
Cortey, A. et al. Management of jaundice in the newborn≥35 GW: From screening to follow-up after discharge. Guidelines for clinical practice. Arch. Pediatr. 24, 192–203 (2017).
Romagnoli, C. et al. Italian guidelines for management and treatment of hyperbilirubinaemia of newborn infants ≥ 35 weeks’ gestational age. Ital. J. Pediatr. 40, 11 (2014).
German guidelines for diagnosis of hyperbilirubinemia. https://register.awmf.org/assets/guidelines/024-007l_S2k_Hyperbilirubinaemie_Neugeborenen_Diagnostik_Therapie_2015-08-verlaengert.pdf.
Sánchez-Redondo, MD et al. Guidelines for prevention, detection and management of hyperbilirubinaemia in newborns of 35 or more weeks of gestation. Pediatr. (Barc.) 87, 294.e1–294.e8 (2017).
Konstantinou, D. Guidelines for the management of hyperbilirubinemia in neonates of >= 35 weeks of gestation. Pediatriki 75, 12–21 (2012).
Bhutani, V. K., Johnson, L. & Sivieri, E. M. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics 103, 6–14 (1999).
De Luca, D., Jackson, G. L., Tridente, A., Carnielli, V. P. & Engle, W. D. Transcutaneous bilirubin nomograms: A systematic review of population differences and analysis of bilirubin kinetics. Arch. Pediatr. Adolesc. Med. 163, 1054–1059 (2009).
Vidavalur, R. & Devapatla, S. Trends in hospitalizations of newborns with hyperbilirubinemia and kernicterus in United States: an epidemiological study. J. Matern Fetal Neonatal Med 35, 7701–7706 (2022).
Bhatt, P. et al. Trends and Resource Use for Kernicterus Hospitalizations in the United States. Hosp. Pediatr. 12, e185–e190 (2022).
Okumura, A. et al. Neonatal jaundice in preterm infants with bilirubin encephalopathy. Neonatology 118, 301–309 (2021).
Alkén, J., Håkansson, S., Ekéus, C., Gustafson, P. & Norman, M. Rates of extreme neonatal hyperbilirubinemia and kernicterus in children and adherence to national guidelines for screening, diagnosis, and treatment in Sweden. JAMA Netw. Open 2, e190858 (2019).
Donneborg, M. L., Hansen, B. M., Vandborg, P. K., Rodrigo-Domingo, M. & Ebbesen, F. Extreme neonatal hyperbilirubinemia and kernicterus spectrum disorder in Denmark during the years 2000–2015. J. Perinatol. 40, 194–202 (2020).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol. 61, 344–349 (2008).
Hemolytic disease and other neonatal jaundice — Level 4 cause. Institute for Health Metrics and Evaluation., 2020 https://www.healthdata.org/results/gbd_summaries/2019/hemolytic-disease-and-other-neonatal-jaundice-level-4-cause.
Global Burden of Disease Study 2019. https://ghdx.healthdata.org/gbd-2019/data-input-sources.
Stevens, G. A. et al. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet 388, e19–e23 (2016).
GBD results. https://vizhub.healthdata.org/gbd-results/.
World Population Prospects - Population Division - United Nations. https://population.un.org/wpp/.
Joinpoint Regression Program. https://surveillance.cancer.gov/joinpoint/.
De Luca, D., Sanchez-Luna, M., Schettler, K., Bont, L. & Baraldi, E. Universal infant immunisation against respiratory syncytial virus and European inequalities: the pandemics lesson has not been learnt. Lancet Reg. Health Eur. 34, 100753 (2023).
De Luca, D., Romagnoli, C., Tiberi, E., Zuppa, A. A. & Zecca, E. Skin bilirubin nomogram for the first 96 h of life in a European normal healthy newborn population, obtained with multiwavelength transcutaneous bilirubinometry. Acta Paediatr. 97, 146–150 (2008).
Varvarigou, A. et al. Transcutaneous bilirubin nomogram for prediction of significant neonatal hyperbilirubinemia. Pediatrics 124, 1052–1059 (2009).
European Commission. Public Health Newsletter. https://health.ec.europa.eu/other-pages/basic-page/health-eu-newsletter-250-focus_en#:~:text=There%20is%20an%20estimated%20shortage,leaving%20other%20countries%20with%20shortages.
Bhutani, V. K., Vidavalur, R. & Wong, R. J. Advances to diminish global newborn kernicterus mortality. J. Perinatol. 44, 493–500 (2024).
Vidavalur R., Bhutani V. K. Trends in infant mortality due to haemolytic disease and other perinatal jaundice in the USA, 1999–2020. Arch Dis Child Fetal Neonatal Ed fetalneonatal-2023-326006. (2023).
Breindahl, M. et al. The European database for subspecialist training in neonatology - transparency achieved. Neonatology 103, 74–82 (2013).
Missiou-Tsagaraki, S. Screening for glucose-6-phosphate dehydrogenase deficiency as a preventive measure: prevalence among 1,286,000 Greek newborn infants. J. Pediatr. 119, 293–299 (1991).
Triandafyllidou A. Immigration towards Greece at the eve of the 21st century. A critical assessment. https://www.eliamep.gr.
Galanis, P. et al. Public health services knowledge and utilization among immigrants in Greece: A cross-sectional study. BMC Health Serv. Res 13, 350 (2013).
Zilidis, C. & Hadjichristodoulou, C. Economic crisis impact and social determinants of perinatal outcomes and infant mortality in Greece. Int J. Environ. Res Public Health 17, 6606 (2020).
OECD Data Explorer. https://stats.oecd.org/Index.aspx?DataSetCode=MIG.
World Bank Net Migration Data. https://data.worldbank.org/indicator/SM.POP.NETM.
David, M., Pachaly, J., Wiemer, A. & Gross, M. M. Out-of-hospital births in Germany-a comparison of ‘large’, ‘medium’, and ‘small’ free-standing birth centres. Z. Geburtshilfe Neonatol. 210, 166–172 (2006).
Society for Quality in Out-of-Hospital Obstetrics. https://www.quag.de/downloads/Summary%20For%20Out%20Of%20Hospital%20Births%20in%20Germany-2022.pdf.
Benavente-Fernández, I. et al. Hospital discharge criteria for very low birth weight newborns. An. de. Pediatr.ía (Engl. Ed.) 87, 54.e1–54.e8 (2017).
Author information
Authors and Affiliations
Contributions
R.V., D.deL., V.K.B.: responsible for conceptualization and design of the study. D.deL.: wrote the first draft of manuscript, interpreted the findings, reviewed and revised the final draft of manuscript. R.V.: Responsible for data collection, analyzed and visualized the data, wrote the first draft of manuscript, reviewed and revised the final manuscript. V.K.B.: provided critically important inputs into content of the manuscript, provided overall supervision, reviewed the final manuscript. K.F.S., M.S.L., C.D., S.F., and G.M.: Provided valuable inputs into country-level data, revised the manuscript for critically important content and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors accept responsibility to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
As the study used publicly available data with no patient specific information, it was deemed exempt from Institutional Review Board review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vidavalur, R., Schettler, K.F., Dani, C. et al. Trends of extreme hyperbilirubinemia related infant mortality in select European countries (1990–2019). Pediatr Res 98, 121–126 (2025). https://doi.org/10.1038/s41390-024-03695-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03695-2
This article is cited by
-
Neonatal encephalopathy in India: spatiotemporal variations in declining mortality
Pediatric Research (2025)
-
Neonatal hyperbilirubinemia: past lessons, current practices, and future directions
European Journal of Pediatrics (2025)