Abstract
Backgrounds
Pediatric patients with congenital heart disease (CHD) often require surgical repair using cardiopulmonary bypass. Despite advancements, mortality and complication rates remain significant.
Methods & Results
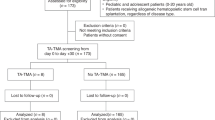
We prospectively examined 101 patients undergoing congenital cardiac surgery, identifying a mortality rate of 4.0% and a complication rate of 31.6%. Neonates and infants exhibited multiple complications more frequently. Prolonged bypass time was significantly associated with complications, with each additional 30 min increasing the odds by 1.46 times (95% CI 1.01–2.10, p = 0.042). We further investigated the involvement of damage-associated molecular pattern (DAMP) molecules by proteomics and ELISA. Plasma levels of DAMPs, including histones and high mobility group box 1 (HMGB1), were significantly elevated in the complication group. As these molecules target Toll-like receptor (TLR)2 and TLR4, mRNA expression of TLR2 and TLR4 in neutrophils was upregulated in the complication group. In vitro and in vivo analyses demonstrated that histones and HMGB1 induced the formation of neutrophil extracellular traps (NETs). This finding aligned with greater NETs formation observed at the end of CPB and during the postoperative period in neonates and infants who developed postoperative complications.
Conclusion
Targeting NETs and associated DAMPs may provide a novel therapeutic approach to mitigate complications in this patient population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All the data are presented in this manuscript.
References
Hoffman, J. I. & Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 39, 1890–1900 (2002).
Gilboa, S. M., Salemi, J. L., Nembhard, W. N., Fixler, D. E. & Correa, A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation 122, 2254–2263 (2010).
Brown, K. L. et al. Incidence and risk factors for important early morbidities associated with pediatric cardiac surgery in a UK population. J. Thorac. Cardiovasc Surg. 158, 1185–1196.e1187 (2019).
Murao, A., Aziz, M., Wang, H., Brenner, M. & Wang, P. Release mechanisms of major DAMPs. Apoptosis 26, 152–162 (2021).
Bianchi, M. E. DAMPs, PAMPs and alarmins: all we need to know about danger. J. Leukoc. Biol. 81, 1–5 (2007).
Kawai, C. et al. Circulating extracellular histones are clinically relevant mediators of multiple organ injury. Am. J. Pathol. 186, 829–843 (2016).
Maisat, W. & Yuki, K. Narrative review of systemic inflammatory response mechanisms in cardiac surgery and immunomodulatory role of anesthetic agents. Ann. Card. Anaesth. 26, 133–142 (2023).
Denning, N. L., Aziz, M., Gurien, S. D. & Wang, P. DAMPs and NETs in sepsis. Front Immunol. 10, 2536 (2019).
Mereweather L. J., Constantinescu-Bercu A., Crawley J. T. B., Salles C., II. Platelet-neutrophil crosstalk in thrombosis. Int. J. Mol. Sci. 2023;24
Carestia, A. et al. Mediators and molecular pathways involved in the regulation of neutrophil extracellular trap formation mediated by activated platelets. J. Leukoc. Biol. 99, 153–162 (2016).
Vourc’h, M., Roquilly, A. & Asehnoune, K. Trauma-induced damage-associated molecular patterns-mediated remote organ injury and immunosuppression in the acutely Ill patient. Front Immunol. 9, 1330 (2018).
Loza, M. J. et al. Assembly of inflammation-related genes for pathway-focused genetic analysis. PLoS ONE 2, e1035 (2007).
Marelli, A., Gauvreau, K., Landzberg, M. & Jenkins, K. Sex differences in mortality in children undergoing congenital heart disease surgery: a United States population-based study. Circulation 122, S234–S240 (2010).
Faraoni, D., Nasr, V. G. & DiNardo, J. A. Overall hospital cost estimates in children with congenital heart disease: analysis of the 2012 Kid’s inpatient database. Pediatr. Cardiol. 37, 37–43 (2016).
Schaefer, L. Complexity of danger: the diverse nature of damage-associated molecular patterns. J. Biol. Chem. 289, 35237–35245 (2014).
Gong, T., Liu, L., Jiang, W. & Zhou, R. DAMP-sensing receptors in sterile inflammation and inflammatory diseases. Nat. Rev. Immunol. 20, 95–112 (2020).
Langseth, M. S. et al. Double-stranded DNA and NETs components in relation to clinical outcome after ST-elevation myocardial infarction. Sci. Rep. 10, 5007 (2020).
Hanata, N. et al. Serum extracellular traps associate with the activation of myeloid cells in SLE patients with the low level of anti-DNA antibodies. Sci. Rep. 12, 18397 (2022).
Lesouhaitier, M. et al. Neutrophil function and bactericidal activity against Staphylococcus aureus after cardiac surgery with cardiopulmonary bypass. J. Leukoc. Biol. 111, 867–876 (2022).
Gessler, P., Pfenninger, J., Pfammatter, J. P., Carrel, T. & Dahinden, C. Inflammatory response of neutrophil granulocytes and monocytes after cardiopulmonary bypass in pediatric cardiac surgery. Intensiv. Care Med. 28, 1786–1791 (2002).
Narasaraju, T. et al. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am. J. Pathol. 179, 199–210 (2011).
Hidalgo, A. et al. Neutrophil extracellular traps: from physiology to pathology. Cardiovasc. Res. 118, 2737–2753 (2022).
Block H., Rossaint J., Zarbock A. The fatal circle of NETs and NET-Associated DAMPs contributing to organ dysfunction. Cells. 11, 1919 (2022).
Iba, T., Levi, M. & Levy, J. H. Sepsis-induced coagulopathy and disseminated intravascular coagulation. Semin Thromb. Hemost. 46, 89–95 (2020).
Pircher, J., Engelmann, B., Massberg, S. & Schulz, C. Platelet-neutrophil crosstalk in atherothrombosis. Thromb. Haemost. 119, 1274–1282 (2019).
Mandel J., Casari M., Stepanyan M., Martyanov A., Deppermann C. Beyond hemostasis: platelet innate immune interactions and thromboinflammation. Int. J. Mol. Sci. 23, 3878 (2022).
Urban, C. F. et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 5, e1000639 (2009).
Radermecker C., et al. Neutrophil extracellular traps infiltrate the lung airway, interstitial, and vascular compartments in severe COVID-19. J. Exp. Med. 2020;217.
Döring, Y., Libby, P. & Soehnlein, O. Neutrophil extracellular traps participate in cardiovascular diseases: recent experimental and clinical insights. Circ. Res. 126, 1228–1241 (2020).
Iba, T. et al. Potential diagnostic markers for disseminated intravascular coagulation of sepsis. Blood Rev. 30, 149–155 (2016).
McDonald, B. et al. Platelets and neutrophil extracellular traps collaborate to promote intravascular coagulation during sepsis in mice. Blood 129, 1357–1367 (2017).
Vogel, S. et al. Platelet-derived HMGB1 is a critical mediator of thrombosis. J. Clin. Invest. 125, 4638–4654 (2015).
Zarbock, A., Polanowska-Grabowska, R. K. & Ley, K. Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Rev. 21, 99–111 (2007).
Fuchs, T. A., Bhandari, A. A. & Wagner, D. D. Histones induce rapid and profound thrombocytopenia in mice. Blood 118, 3708–3714 (2011).
Gould, T. J., Lysov, Z. & Liaw, P. C. Extracellular DNA and histones: double-edged swords in immunothrombosis. J. Thromb. Haemost. 13, S82–S91 (2015).
Papayannopoulos, V., Metzler, K. D., Hakkim, A. & Zychlinsky, A. Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J. Cell Biol. 191, 677–691 (2010).
Silvestre-Roig, C., Fridlender, Z. G., Glogauer, M. & Scapini, P. Neutrophil diversity in health and disease. Trends Immunol. 40, 565–583 (2019).
Funding
This is supported by NICHD R21HD109119 (K.Y.).
Author information
Authors and Affiliations
Contributions
Idea and Experiment design- W.M., L.H., Y.C., S.E., S.W.K., J.C, and K.Y. Experiment execution- W.M., L.H., S.S., Y.S., S.E. Manuscript draft- W.M., K.Y. Manuscript editing- S.K., H.V.P., S.E., Grant acquisition- K.Y.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
For clinical samples, the protocol was approved by the Boston Children’s Hospital IRB committee, and we obtained consent from patients’ parents and/or guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Posted history: This manuscript was previously posted to bioRxiv preprint https://doi.org/10.1101/2023.12.21.572768.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maisat, W., Hou, L., Sandhu, S. et al. Neutrophil extracellular traps formation is associated with postoperative complications in congenital cardiac surgery. Pediatr Res 98, 1545–1558 (2025). https://doi.org/10.1038/s41390-024-03717-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03717-z
This article is cited by
-
Revisiting risk factors and incidence of postoperative tachyarrhythmias in pediatric cardiac surgery
Scientific Reports (2025)