Abstract
Objective
To explore the role of daily trans-anal irrigation (TAI) before pull-through surgery in preventing Hirschsprung disease-associated enterocolitis (HAEC) and improving other clinical outcomes in short-segment Hirschsprung disease (HSCR).
Methods
We enrolled the children with short-segment HSCR who received primary pull-through surgery from February 2012 to August 2019 at our hospital. They were divided into two groups. Daily TAI group: daily TAI once diagnosed until undergoing surgery. Non-daily TAI group: anal dilation or glycerine enema, supplemented with TAI if these were noneffective. HAEC, nutritional status at surgery, postoperative rehabilitation, and long-term defecation function were compared.
Results
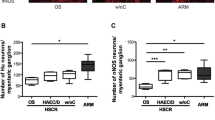
A total of 191 children were enrolled, 147 in the Daily TAI group and 44 others. 44 pairs of children were successfully matched by 1:1 propensity score matching. In all, 10 (11.36%) of the 88 children developed HAEC, 5 (5/44, 11.36%) in the Daily TAI group and 5 (5/44, 11.36%) in another, and the difference was not statistically significant (χ2 = 0.000, p = 1.000). Besides, there was no significant difference in the nutritional status at surgery, postoperative rehabilitation indicators, and the defecation function.
Conclusion
For children with short-segment HSCR, preoperative daily TAI had no significant advantage over non-daily TAI in preventing HAEC and improving other clinical outcomes.
Impact
-
For children with short-segment Hirschsprung disease, one or more times trans-anal irrigations (TAI) per day before pull-through surgery may not be necessary.
-
Daily TAI had no significant advantage over non-daily TAI in preventing preoperative and postoperative HAEC.
-
Whether to receive daily TAI before surgery did not affect postoperative recovery and long-term defecation function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Taguchi, T., Obata, S. & Ieiri, S. Current status of Hirschsprung’s disease: based on a nationwide survey of Japan. Pediatr. Surg. Int. 33, 497–504 (2017).
Kyrklund, K. et al. Ernica guidelines for the management of rectosigmoid Hirschsprung’s disease. Orphanet J. Rare Dis. 15, 164 (2020).
Westfal, M. L. et al. Optimal timing for soave primary pull-through in short-segment Hirschsprung disease: a meta-analysis. J. Pediatr. Surg. 57, 719–725 (2022).
Zani, A. et al. European paediatric surgeons’ association survey on the management of Hirschsprung disease. Eur. J. Pediatr. Surg. 27, 96–101 (2017).
Lewit, R. A., Kuruvilla, K. P., Fu, M. & Gosain, A. Current understanding of Hirschsprung-associated enterocolitis: pathogenesis, diagnosis and treatment. Semin Pediatr. Surg. 31, 151162 (2022).
Zhang, Z. et al. Hirschsprung-associated enterocolitis: transformative research from bench to bedside. Eur. J. Pediatr. Surg. 32, 383–390 (2022).
Onishi, S. et al. Optimal timing of definitive surgery for Hirschsprung’s disease to achieve better long-term bowel function. Surg. Today 52, 92–97 (2022).
Lu, C. et al. Single-stage transanal endorectal pull-through procedure for correction of Hirschsprung disease in neonates and nonneonates: a multicenter study. J. Pediatr. Surg. 52, 1102–1107 (2017).
Lu, C. et al. Feasibility and efficacy of home rectal irrigation in neonates and early infancy with Hirschsprung disease. Pediatr. Surg. Int. 35, 1245–1253 (2019).
Lin, Z., Lin, Y., Bai, J., Wu, D. & Fang, Y. Outcomes of preoperative anal dilatation for Hirschsprung disease. J. Pediatr. Surg. 56, 483–486 (2021).
Zhang, J. S., Kong, C. & Li, L. Endoscopic decompression with a transanal drainage tube for the treatment of Hirschsprung’s disease in newborns. J. Laparoendosc. Adv. Surg. Tech. A 31, 959–963 (2021).
Mosiello, G. et al. Consensus review of best practice of transanal irrigation in children. J. Pediatr. Gastroenterol. Nutr. 64, 343–352 (2017).
Hill, B. & Mitchell, A. Transanal irrigation at a glance. Br. J. Nurs. 31, 308–314 (2022).
Gayer, G., Zissin, R., Apter, S., Oscadchy, A. & Hertz, M. Perforations of the rectosigmoid colon induced by cleansing enema: Ct findings in 14 patients. Abdom. Imaging 27, 453–457 (2002).
Gosain, A. et al. Guidelines for the diagnosis and management of Hirschsprung-associated enterocolitis. Pediatr. Surg. Int. 33, 517–521 (2017).
Teitelbaum, D. H., Drongowski, R. A., Chamberlain, J. N. & Coran, A. G. Long-term stooling patterns in infants undergoing primary endorectal pull-through for Hirschsprung’s disease. J. Pediatr. Surg. 32, 1049–1052 (1997).
Austin, P. C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 46, 399–424 (2011).
Best, K. E. et al. Hirschsprung’s disease prevalence in Europe: a register based study. Birth Defects Res A Clin. Mol. Teratol. 100, 695–702 (2014).
Bradnock, T. J. & Walker, G. M. Evolution in the management of Hirschsprung’s disease in the UK and Ireland: a national survey of practice revisited. Ann. R. Coll. Surg. Engl. 93, 34–38 (2011).
Lee, C. C. et al. Clinical impacts of delayed diagnosis of Hirschsprung’s disease in newborn infants. Pediatr. Neonatol. 53, 133–137 (2012).
Beltman, L., Labib, H., Oosterlaan, J., van Heurn, E. & Derikx, J. Risk factors for complications in patients with Hirschsprung disease while awaiting surgery: beware of bowel perforation. J. Pediatr. Surg. 57, 561–568 (2022).
Kessmann, J. Hirschsprung’s disease: diagnosis and management. Am. Fam. Physician 74, 1319–1322 (2006).
Wessner, S. & Burjonrappa, S. Review of nutritional assessment and clinical outcomes in pediatric surgical patients: does preoperative nutritional assessment impact clinical outcomes? J. Pediatr. Surg. 49, 823–830 (2014).
Wang, D. et al. Screening of undernutrition in children with Hirschsprung disease using preoperative anthropometric parameters: a multicenter cross-sectional study. JPEN J. Parenter. Enter. Nutr. 47, 151–158 (2023).
Ahmad, H. et al. Evaluation and treatment of the post pull-through Hirschsprung patient who is not doing well; update for 2022. Semin. Pediatr. Surg. 31, 151164 (2022).
Langer, J. C. et al. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr. Surg. Int. 33, 523–526 (2017).
Saadai, P. et al. Guidelines for the management of postoperative soiling in children with Hirschsprung disease. Pediatr. Surg. Int. 35, 829–834 (2019).
Aworanti, O. M., McDowell, D. T., Martin, I. M. & Quinn, F. Does functional outcome improve with time postsurgery for Hirschsprung disease? Eur. J. Pediatr. Surg. 26, 192–199 (2016).
Temple, S. J., Shawyer, A. & Langer, J. C. Is daily dilatation by parents necessary after surgery for Hirschsprung disease and anorectal malformations? J. Pediatr. Surg. 47, 209–212 (2012).
Acknowledgements
This work was supported by The Natural Science Foundation of China (81801496), and Nanjing Special Fund for Health Science and Technology Development (YKK21147).
Author information
Authors and Affiliations
Contributions
Study design: W.B.T., J.T., H.L. Data collection: H.L., J.T., C.G.L. Statistical analysis: H.L., J.T., W.L. Writing of the first draft of the manuscript: H.L., J.T. Manuscript revision: W.B.T., J.T.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent was obtained from the parents or guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, H., Tang, J., Lu, C. et al. For short-segment Hirschsprung disease, daily trans-anal irrigation before pull-through surgery is necessary?. Pediatr Res 98, 224–230 (2025). https://doi.org/10.1038/s41390-024-03730-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03730-2