Abstract
Background
The immune heterogeneity of biliary atresia (BA) presents a challenge for development of prognostic biomarkers. This study aimed to identify early immune signatures associated with biliary drainage after Kasai Portoenterostomy (KPE).
Methods
Serum samples, liver slides, and clinical data were obtained from patients enrolled in the NIDDK-supported Childhood Liver Disease Research Network. Serum cytokines and hepatic immune cell subsets were measured at diagnosis and compared among 3 groups: 38 infants with BA (20 with evidence of bile flow after KPE; 18 without) and 17 non-BA cholestatic infants.
Results
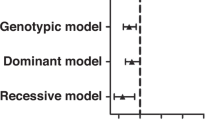
BA participants had lower numbers of lipid associated macrophages (LAM), and increased serum levels of Eotaxin-3, interleukin (IL) 12p70, and IL-8 versus non-BA groups (p < 0.05 for all). Among BA participants, monocyte like macrophages and serum levels of granulocyte-macrophage colony stimulating factor (GM-CSF) were increased in BA participants with good biliary drainage (p = 0.004 and p < 0.001 respectively). Levels of GM-CSF, IL-16, c-reactive protein, TNF-β predicted successful biliary drainage with an area under the receiver operating curve of 0.84 (p < 0.001).
Conclusion
These findings suggest that distinct macrophage-associated immune networks at diagnosis may impact biliary drainage after KPE. Identification of early prognostic immune-modulatory markers has potential to improve patient stratification for medical and surgical therapies.
Impact statement
-
We identify serum cytokines, particularly GM-CSF, that are associated with future biliary drainage in patients with biliary atresia.
-
Characterization of macrophage-associated immune networks provides novel insight into early disease mechanism that may impact patient outcomes.
-
Early prognostic biomarkers markers in biliary atresia can help in patient stratification for medical and surgical therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Bezerra, J. A. et al. Biliary atresia: Clinical and research challenges for the twenty-first century. Hepatology 68, 1163–1173 (2018).
Kilgore, A. & Mack, C. L. Update on investigations pertaining to the pathogenesis of biliary atresia. Pediatr Surg Int 33, 1233–1241 (2017).
Ortiz-Perez, A. et al. Innate immunity and pathogenesis of biliary atresia. Front Immunol 11, 329 (2020).
Shneider, B. L. et al. Total serum bilirubin within 3 months of hepatoportoenterostomy predicts short-term outcomes in biliary atresia. J Pediatr 170, 211–217.e211-212 (2016).
Serinet, M. O. et al. Impact of age at kasai operation on its results in late childhood and adolescence: A rational basis for biliary atresia screening. Pediatrics 123, 1280–1286 (2009).
Superina, R. et al. The anatomic pattern of biliary atresia identified at time of kasai hepatoportoenterostomy and early postoperative clearance of jaundice are significant predictors of transplant-free survival. Ann Surg 254, 577–585 (2011).
Hukkinen, M., Pihlajoki, M. & Pakarinen, M. P. Predicting native liver injury and survival in biliary atresia. Semin Pediatr Surg 29, 150943 (2020).
Lages, C. S. et al. The dendritic Cell-T Helper 17-macrophage axis controls cholangiocyte injury and disease progression in murine and human biliary atresia. Hepatology 65, 174–188 (2017).
Mack, C. L. et al. Biliary atresia is associated with Cd4+ Th1 cell-mediated portal tract inflammation. Pediatr Res 56, 79–87 (2004).
Russo, P. et al. Key histopathologic features of liver biopsies that distinguish biliary atresia from other causes of infantile cholestasis and their correlation with outcome: A multicenter study. Am J Surg Pathol 40, 1601–1615 (2016).
Hill, R. et al. Th-17 cells infiltrate the liver in human biliary atresia and are related to surgical outcome. J Pediatr Surg 50, 1297–1303 (2015).
Kim, S. et al. Correlation of immune markers with outcomes in biliary atresia following intravenous immunoglobulin therapy. Hepatol Commun 3, 685–696 (2019).
Lopez, R. N., Ooi, C. Y. & Krishnan, U. Early and peri-operative prognostic indicators in infants undergoing hepatic portoenterostomy for biliary atresia: A review. Curr Gastroenterol Rep 19, 16 (2017).
Wu, J. F. et al. Quantification of serum matrix metallopeptide 7 levels may assist in the diagnosis and predict the outcome for patients with biliary atresia. J Pediatr 208, 30–37.e31 (2019).
Kobayashi, H., Puri, P., O’Briain, D. S., Surana, R. & Miyano, T. Hepatic Overexpression of Mhc Class Ii Antigens and Macrophage-Associated Antigens (Cd68) in patients with biliary atresia of poor prognosis. J Pediatr Surg 32, 590–593 (1997).
Udomsinprasert, W., Ungsudechachai, T., Vejchapipat, P., Poovorawan, Y. & Honsawek, S. Systemic cytokine profiles in biliary atresia. PLoS ONE 17, e0267363 (2022).
Arango Duque, G. & Descoteaux, A. Macrophage cytokines: Involvement in immunity and infectious diseases. Front Immunol 5, 491 (2014).
Wen, Y., Lambrecht, J., Ju, C. & Tacke, F. Hepatic macrophages in liver homeostasis and diseases-diversity, plasticity and therapeutic opportunities. Cell Mol Immunol 18, 45–56 (2021).
Taylor, S. A. et al. Transcriptional profiling of pediatric cholestatic livers identifies three distinct macrophage populations. PLoS ONE 16, e0244743 (2021).
Jaitin, D. A. et al. Lipid-associated macrophages control metabolic homeostasis in a Trem2-dependent manner. Cell 178, 686–698.e614 (2019).
Schwarz, K. B. et al. Extrahepatic anomalies in infants with biliary atresia: results of a large prospective North American Multicenter Study. Hepatology 58, 1724–1731 (2013).
Antala, S. & Taylor, S. A. Biliary atresia in children: Update on disease mechanism, therapies, and patient outcomes. Clin Liver Dis 26, 341–354 (2022).
Tracy, T. F. Jr., Dillon, P., Fox, E. S., Minnick, K. & Vogler, C. The inflammatory response in pediatric biliary disease: Macrophage phenotype and distribution. J Pediatr Surg 31, 121–125 (1996).
Davenport, M. et al. Immunohistochemistry of the liver and biliary tree in extrahepatic biliary atresia. J Pediatr Surg 36, 1017–1025 (2001).
Nagayabu, K. et al. The clinical impact of macrophage polarity after kasai portoenterostomy in biliary atresia. Front Pediatr 12, 1338131 (2024).
Wang, J. et al. Liver immune profiling reveals pathogenesis and therapeutics for biliary atresia. Cell 183, 1867–1883.e1826 (2020).
Ye, C. et al. Single-cell and spatial transcriptomics reveal the fibrosis-related immune landscape of biliary atresia. Clin Transl Med 12, e1070 (2022).
Ye, R. et al. Single cell RNA-sequencing analysis reveals that n-acetylcysteine partially reverses hepatic immune dysfunction in biliary atresia. JHEP Rep 5, 100908 (2023).
Ram, A. K. et al. Polymeric immunoglobulin receptor and galectin-3-binding protein are raised in biliary atresia: reveals a proteomic-based study. J Proteom 287, 104974 (2023).
She, S. et al. Functional roles of chemokine receptor ccr2 and its ligands in liver disease. Front Immunol 13, 812431 (2022).
Seki, E. et al. Ccr2 promotes hepatic fibrosis in mice. Hepatology 50, 185–197 (2009).
Cai, S. Y. et al. Bile acids initiate cholestatic liver injury by triggering a hepatocyte-specific inflammatory response. JCI Insight 2, e90780 (2017).
Feng, D. et al. Monocyte-derived macrophages orchestrate multiple cell-type interactions to repair necrotic liver lesions in disease models. J Clin Invest 133, e166954 (2023).
Martin, M. & Blom, A. M. Complement in removal of the dead - balancing inflammation. Immunol Rev 274, 218–232 (2016).
Eguchi, A. et al. Complement complex 1 subunit q-mediated hepatic stellate cell activation with connective tissue growth factor elevation is a prognostic factor for survival in rat and human chronic liver diseases. Hepatol Commun 6, 3515–3527 (2022).
Vonderlin, J., Chavakis, T., Sieweke, M. & Tacke, F. The multifaceted roles of macrophages in NAFLD pathogenesis. Cell Mol Gastroenterol Hepatol 15, 1311–1324 (2023).
Madadi-Sanjani, O. et al. Growth factors assessed during kasai procedure in liver and serum are not predictive for the postoperative liver deterioration in infants with biliary atresia. J Clin Med 10, 1978 (2021).
Nguyen, H. P. A. et al. Study protocol of phase 2 open-label multicenter randomized controlled trial for granulocyte-colony stimulating factor (Gcsf) in post-kasai type 3 biliary atresia. Pediatr Surg Int 38, 1019–1030 (2022).
Mysore, K. R., Shneider, B. L. & Harpavat, S. Biliary atresia as a disease starting in utero: implications for treatment, diagnosis, and pathogenesis. J Pediatr Gastroenterol Nutr 69, 396–403 (2019).
Harpavat, S., Finegold, M. J. & Karpen, S. J. Patients with biliary atresia have elevated direct/conjugated bilirubin levels shortly after birth. Pediatrics 128, e1428–e1433 (2011).
Acknowledgements
The authors acknowledge the support provided by the Northwestern University Pathology Core and Immunotherapy Assessment Core. Heather Van Doren, Senior Medical Editor with Arbor Research Collaborative for Health, provided editorial assistance on this manuscript.
Funding
Supported by the National Institute of Diabetes, Digestive, and Kidney Diseases (NIDDK) U01 grants (DK103149 to Baylor College of Medicine, DK062470 to Children’s Healthcare of Atlanta, DK103135 to The Hospital for Sick Children, DK062436 and DK062436-19S1 to Ann & Robert H. Lurie Children’s Hospital of Chicago, DK062497 to Cincinnati Children’s Hospital Medical Center, DK103140 to University of Utah, DK084575 to Seattle Children’s Hospital, DK062481 to The Children’s Hospital of Philadelphia, DK062466 to Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center, DK062456 to University of Michigan, DK084536 to Riley Hospital for Children, DK062500 to University of California San Francisco Children’s Hospital, DK084538 to Children’s Hospital Los Angeles, DK062453 to University of Colorado Denver and Children’s Hospital Colorado) and the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), Clinical and Translational Sciences Awards (UL1TR002378 to Children’s Healthcare of Atlanta, UL1 TR000423 and UL1 RR025014 to Seattle Children’s Hospital, UL1 TR001878 to The Children’s Hospital of Philadelphia, UL1 TR001857 to Children’s Hospital of Pittsburgh of UPMC, UL1 TR001872 to UCSF Children’s Hospital, UL1 TR002535 and UM1 TR004399 to University of Colorado Denver, and UL1TR00130 to Children’s Hospital of Los Angeles). Additional support provided by NIDDK K08 grant DK121937 and R03 grant DK135784 (Sarah A. Taylor).
Author information
Authors and Affiliations
Consortia
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data was made by SAT, SH, KDG, SJK, RJS, EMA, and CLM. Drafting the article or revising it critically for important intellectual content was performed by SAT, SH, KML, JAB, CJ, PLV, RJS, EMA, and CLM. Final approval of the version to be published was completed by all authors: SAT, SH, KDG, VA, KML, JAB, CJ, KW, SH, PR, JT, PLV, VLN, SJK, RJS, EMA, and CLM.
Corresponding author
Ethics declarations
Competing interests
SAT serves as a consultant for Ipsen and Mirum Pharma. SH serves on the Data Safety Monitoring Board coordinated by Syneos Health for a therapeutic drug trial for biliary atresia. KML serves as a consultant for Ipsen and Mirum Pharma. PV serves on the Speaker’s Bureau for Mirum and is a consultant for Grifols. SJK serves as a consultant for Ipsen, Hemoshear, Intercept, Mirum, and Vertex. RJS serves as consultant for Ipsen and Mirum Pharma. All remaining coauthors declare no conflicts of interest for this manuscript.
Consent statement
Written informed consent was obtained for all participants. Institutional review board approval was obtained for the study and conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taylor, S.A., Harpavat, S., Gromer, K.D. et al. Increased serum GM-CSF at diagnosis of biliary atresia is associated with improved biliary drainage. Pediatr Res 98, 1386–1394 (2025). https://doi.org/10.1038/s41390-025-03804-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-03804-9
This article is cited by
-
Prognostic biomarkers of biliary atresia—are we there yet?
Pediatric Research (2025)