Abstract
Background
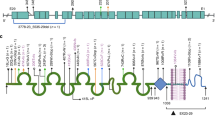
Nucleoporin nephropathy, a rare genetic kidney disorder, is not well-characterized despite its early onset in childhood.
Method
We analyzed the clinical and genetic data of pediatric patients diagnosed with nucleoporin nephropathy at a southern Chinese pediatric nephrology center, and reviewed global cases reported up until July 2024.
Results
In our center, five pediatric patients (aged 10 months to 8 years) were diagnosed with nucleoporin nephropathy. Three presented with steroid-resistant nephrotic syndrome, and one had initial extrarenal symptoms. All patients progressed to end-stage kidney disease. Global data shows 111 cases of nucleoporin nephropathy; 76.6% of patients initially presented with nephrotic syndrome, unresponsive to steroids or immunosuppressive therapy. 89.4% progressed to end-stage kidney disease in adolescence. Among the 37 transplant recipients, only 2 had proteinuria recurrence. Neurological symptoms were observed in a significant portion of patients, with variation across genotypes. East Asian patients, who account for 40.4% of the cases, often exhibit compound heterozygous missense, early renal involvement, and fewer extrarenal symptoms.
Conclusion
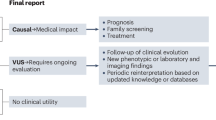
Routine nucleoporin gene testing is advised for Asian children with steroid-resistant nephrotic syndrome or end-stage kidney disease to prevent unnecessary treatments. While kidney transplantation has a favorable outlook, managing extrarenal symptoms of nucleoporin pehropathy is challenging.
Impact
-
Explore the link between nucleoporin gene mutations and disease phenotypes for a new understanding of NUP nephropathy.
-
The renal phenotypes associated with NUP mutations display a remarkably consistent pattern as early-onset SRNS and progression to ESKD in adolescence.
-
Highlight the importance in finding and managing the extrarenal symptoms associated with nucleoporin nephropathy.
-
Regional specificities in NUP gene mutations are becoming apparent, with East Asian patients often presenting compound heterozygous mutations, early onset, rapid progression to end-stage kidney disease, and fewer extrarenal symptoms.
-
Emphasize the necessity of nucleoporin gene testing for Asian children to prevent ineffective treatments.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available within the article and its supplementary materials. Additional data related to this research can be requested from the corresponding author upon reasonable request.
References
Knockenhauer, K. E. & Schwartz, T. U. The Nuclear Pore Complex as a Flexible and Dynamic Gate. Cell 164, 1162–1171 (2016).
Nofrini, V., Di Giacomo, D. & Mecucci, C. Nucleoporin genes in human diseases. Eur. J. Hum. Genet 24, 1388–1395 (2016).
Miyake, N. et al. Biallelic Mutations in Nuclear Pore Complex Subunit NUP107 Cause Early-Childhood-Onset Steroid-Resistant Nephrotic Syndrome. Am. J. Hum. Genet. 97, 555–566 (2015).
Lipska-Zietkiewicz, B. S. & Schaefer, F. NUP Nephropathy: When Defective Pores Cause Leaky Glomeruli. Am. J. Kidney Dis. 73, 890–892 (2019).
Park, E. et al. NUP107 mutations in children with steroid-resistant nephrotic syndrome. Nephrol. Dial. Transpl. 32, 1013–1017 (2017).
Gambadauro, A. et al. NUP85 as a Neurodevelopmental Gene: From Podocyte to Neuron. Genes 14, 2143 (2023).
Rao, J. et al. Genetic spectrum of renal disease for 1001 Chinese children based on a multicenter registration system. Clin. Genet. 96, 402–410 (2019).
Nagano, C. et al. Comprehensive genetic diagnosis of Japanese patients with severe proteinuria. Sci. Rep. 10, 270 (2020).
Rosti, R. O. et al. Homozygous mutation in NUP107 leads to microcephaly with steroid-resistant nephrotic condition similar to Galloway-Mowat syndrome. J. Med. Genet. 54, 399–403 (2017).
Bierzynska, A. et al. Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management. Kidney Int. 91, 937–947 (2017).
Braun, D. A. et al. Mutations in multiple components of the nuclear pore complex cause nephrotic syndrome. J. Clin. Invest. 128, 4313–4328 (2018).
Hashimoto, T. et al. In Vivo Expression of NUP93 and Its Alteration by NUP93 Mutations Causing Focal Segmental Glomerulosclerosis. Kidney Int. Rep. 4, 1312–1322 (2019).
Sandokji, I. et al. Identification of novel mutations and phenotype in the steroid resistant nephrotic syndrome gene NUP93: a case report. Bmc Nephrol. 20, 271 (2019).
Warejko, J. K. et al. Whole Exome Sequencing of Patients with Steroid-Resistant Nephrotic Syndrome. Clin. J. Am. Soc. Nephro 13, 53–62 (2018).
Bierzynska et al. Exploring the Relevance of NUP93 Variants in Steroid-Resistant Nephrotic Syndrome Using next Generation Sequencing and a Fly Kidney Model. Pediatr. Nephrol. 37, 2643–2656 (2022).
Bezdicka, M. et al. Genetic diagnosis of steroid-resistant nephrotic syndrome in a longitudinal collection of Czech and Slovak patients: a high proportion of causative variants in NUP93. Pediatr. Nephrol. 33, 1347–1363 (2018).
Braun, D. A. et al. Mutations in nuclear pore genes NUP93, NUP205 and XPO5 cause steroid-resistant nephrotic syndrome. Nat. Genet. 48, 457–465 (2016).
Wasilewska, A., Rybi-Szuminska, A. & Dubiela, P. Steroid-Resistant Nephrotic Syndrome Caused by NUP93 Pathogenic Variants. J. Clin. Med. 12, 5810 (2023).
Zhao, B. et al. Steroid-resistant nephrotic syndrome in infants caused by a novel compound heterozygous mutation of the NUP93: A CARE case report. Medicine 100, e24627 (2021).
Acharya, R. & Upadhyay, K. End-stage renal disease in a child with focal segmental glomerulosclerosis associated with a homozygous NUP93 variant. Clin. Case Rep. 9, e05111 (2021).
Park, E. et al. Genetic Study in Korean Pediatric Patients with Steroid-Resistant Nephrotic Syndrome or Focal Segmental Glomerulosclerosis. J. Clin. Med. 2020, 9 (2013).
Han, Y. et al. Mutations in the NUP93, NUP107 and NUP160 Genes Cause Steroid-Resistant Nephrotic Syndrome in Chinese Children. Ital. J. Pediatr. 50, 81 (2024).
Wang, Q. et al. Steroid-Resistant Nephrotic Syndrome Caused by Nuclear Pore Gene NUP133 Variation. Clin. Genet. 104, 272–274 (2023).
Zhao, F. et al. Mutations in NUP160 Are Implicated in Steroid-Resistant Nephrotic Syndrome. J. Am. Soc. Nephrol. 30, 840–853 (2019).
Warejko, J. K. et al. Whole Exome Sequencing of Patients with Steroid-Resistant Nephrotic Syndrome. Clin. J. Am. Soc. Nephrol. 13, 53–62 (2018).
Park, E., et al. Genetic Study in Korean Pediatric Patients with Steroid-Resistant Nephrotic Syndrome or Focal Segmental Glomerulosclerosis. J. Clin. Med. 2020, 9 (2013).
Wang, F. et al. Spectrum of mutations in Chinese children with steroid-resistant nephrotic syndrome. Pediatr. Nephrol. 32, 1181–1192 (2017).
Trautmann, A. et al. Spectrum of steroid-resistant and congenital nephrotic syndrome in children: the PodoNet registry cohort. Clin. J. Am. Soc. Nephrol. 10, 592–600 (2015).
Wang, Y. et al. Mutation spectrum of genes associated with steroid-resistant nephrotic syndrome in Chinese children. Gene 625, 15–20 (2017).
Sadowski, C. E. et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J. AM Soc. Nephrol. 26, 1279–1289 (2015).
Seeman, T. & Vondrak, K. First Report of Recurrent Nephrotic Syndrome After Kidney Transplantation in a Patient With NUP93 Gene Mutations: A Case Report. Transpl. P 50, 3954–3956 (2018).
Acknowledgements
We thanks the patients and their families for their participation. We thank Dr. Liulu Xie for her assistance collecting the patients’ clinical data. We also thank for the assistance provided from all the members in Pediatric Nephrology Center and Kidney Transplantation Center of the First Affiliated Hospital of Sun Yat-sen University. This work was supported by The National Key Research and Development Program of China (2022YFC2705100, 2022YFC2705101), Guangdong Basic and Applied Basic Research Foundation (No. 2019A1515010694). The funding source helped to perform the literature search and patients’ follow up, but did not have any role in design, execution, analysis, interpretation, or writing of the report or the decision to submit this report for publication. The authors declare that they have no relevant financial interests.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. This subject was designed by X.J. and L.C. Data collection and literature review were performed by Y.P. and M.J.. Data analysis was re-checked by L.R. and Z.L. The first draft of the manuscript was written by Y.P. and all authors commented on previous versions of the manuscript. The corresponding authors had full access to all the study data and had final responsibility for the decision to submit.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Consent for publication was obtained from the institution and the parents of the patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pei, Y., Jiang, M., Zhilang, L. et al. Exploring genotype-phenotype correlation in nucleoporin nephropathy. Pediatr Res 98, 1876–1883 (2025). https://doi.org/10.1038/s41390-025-03977-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-03977-3