Abstract
Background
Preterm birth (PTB) etiology remains poorly understood. Our aim was to investigate the relation of environmental factors and specific gene polymorphisms involved in PTB in the context of stressful life events during pregnancy.
Methods
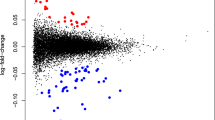
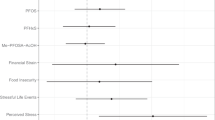
Parental sociodemographic and obstetric data as well as genetic variants of 1263 preterm newborns were analyzed. Logistic regressions were used to identify shared environmental and genetic risk factors for PTB and stressful life events. A Lasso Ridge logistic regression with cross-validation was used to select the best predictors of maternal stress. Associations were evidenced through Bayesian networks.
Results
Starting from a great number of variables, our model was processed and reduced until it allowed to visualize only two environmental factors (alcohol intake and chronic hypertension) along with three SNPs rs66911171 (CR1), rs854552 (PON1), rs4966038 (IGF1R) and two interactions rs854552 x rs4966038 (PON1xIGFR1) and rs5742612 x rs1942386 (IGF1xPGR) related to PTB and maternal stress.
Conclusion
Machine learning techniques allow us to identify two environmental factors, three genetic markers, and two interactions related to PTB in the context of stressful life events. Findings of this exploratory study contribute to the understanding of the complex pathways relating maternal stress and PTB.
Impact
-
An analysis of environmental factors and preterm birth specific gene polymorphisms in the context of stressful life events during pregnancy is presented.
-
Alcohol intake and chronic hypertension along with SNPs of CR1, PON1, IGF1R and two interactions PON1xIGFR1 and IGF1xPGR are shown as related to preterm birth in the context of stressful life events.
-
This research could help in developing targeted interventions and preventive strategies for at-risk populations.
-
The study emphasizes the potential of machine learning to interpret biological and social interactions affecting health outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Christian, L. M. Physiological reactivity to psychological stress in human pregnancy: Current knowledge and future directions. Prog. Neurobiol. 99, 106–116 (2012).
Lobel, M., DeVincent, C. J., Kaminer, A. & Meyer, B. A. The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychol. 19, 544–553 (2000).
Staneva, A., Bogossian, F., Pritchard, M. & Wittkowski, A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 28, 179–193 (2015).
Wadhwa, P. D., Entringer, S., Buss, C. & Lu, M. C. The contribution of maternal stress to preterm birth: issues and considerations. Clin. Perinatol. 38, 351–384 (2011).
Bream, E. N. A. et al. Candidate gene linkage approach to identify DNA variants that predispose to preterm birth. Pediatr. Res 73, 135–141 (2013).
Mann, P. C. et al. Polymorphisms in the fetal progesterone receptor and a calcium-activated potassium channel isoform are associated with preterm birth in an Argentinian population. J. Perinatol. 33, 336–340 (2013).
Ryckman, K. K. et al. Maternal and fetal genetic associations of PTGER3 and PON1 with preterm birth. PLoS One 5, e9040 (2010).
Romero, R. et al. Identification of fetal and maternal single nucleotide polymorphisms in candidate genes that predispose to spontaneous preterm labor with intact membranes. Am. J. Obstet. Gynecol. 202, 431.e1–34 (2010).
Romero, R. et al. A genetic association study of maternal and fetal candidate genes that predispose to preterm prelabor rupture of membranes (PROM). Am. J. Obstet. Gynecol. 203, 361.e1–361.e30 (2010).
Strauss, J. F. et al. Spontaneous preterm birth: advances toward the discovery of genetic predisposition. Am. J. Obstet. Gynecol. 218, 294–314.e2 (2018).
Krupitzki, H. B. et al. Environmental risk factors and perinatal outcomes in preterm newborns, according to family recurrence of prematurity. Am. J. Perinatol. 30, 451–461 (2013).
Gimenez, L. G. et al. Maternal and neonatal epidemiological features in clinical subtypes of preterm birth. J. Matern Fetal Neonatal Med 29, 3153–3161 (2016).
Gimenez, L. G. et al. Association of candidate gene polymorphisms with clinical subtypes of preterm birth in a Latin American population. Pediatr. Res 82, 554–559 (2017).
Elias, D. et al. Preterm birth and genitourinary tract infections: assessing gene-environment interaction. Pediatr. Res 90, 678–683 (2021).
Elias, D. et al. Preterm birth etiological pathways: a Bayesian networks and mediation analysis approach. Pediatr. Res 91, 1882–1889 (2022).
Elias, D. E. et al. Genes, exposures, and interactions on preterm birth risk: an exploratory study in an Argentine population. J. Community Genet 13, 557–565 (2022).
Dunkel-Schetter, C. & Glynn, L. Stress in pregnancy: empirical evidence and theoretical issues to guide interdisciplinary researchers. In Handbook of Stress Science (Contrada, R., Baum. A., eds) 321–343 (Springer, New York: 2011).
Glynn, L. M., Schetter, C. D., Hobel, C. J. & Sandman, C. A. Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychol. 27, 43–51 (2008).
Pearce, B. D. et al. Interrelationship of cytokines, hypothalamic-pituitary-adrenal axis hormones, and psychosocial variables in the prediction of preterm birth. Gynecol. Obstet. Invest 70, 40–46 (2010).
Zietlow, A.-L., Nonnenmacher, N., Reck, C., Ditzen, B. & Müller, M. Emotional Stress During Pregnancy - Associations With Maternal Anxiety Disorders, Infant Cortisol Reactivity, and Mother-Child Interaction at Pre-school Age. Front Psychol. 10, 2179 (2019).
Alfaro, E. L., Dipierri, J. E., Gutiérrez, N. I. & Vullo, C. M. Genetic structure and admixture in urban populations of the Argentine North-West. Ann. Hum. Biol. 32, 724–737 (2005).
Khashan, A. S. et al. Rates of preterm birth following antenatal maternal exposure to severe life events: a population-based cohort study. Hum. Reprod. 24, 429–437 (2009).
Castilla, E. E. & Orioli, I. M. ECLAMC: the Latin-American collaborative study of congenital malformations. Community Genet 7, 76–94 (2004).
Manetti, G. et al. Continuous quality improvement through use of perinatal clinical record and AGUSTINA database. Stud. Health Technol. Inf. 52, 824–826 (1998).
Wang, J. et al. High-throughput single nucleotide polymorphism genotyping using nanofluidic Dynamic Arrays. BMC Genomics 10, 561 (2009).
Esper, L. H. & Furtado, E. F. Stressful life events and alcohol consumption in pregnant women: A cross-sectional survey. Midwifery 71, 27–32 (2019).
Morgan, N., Christensen, K., Skedros, G., Kim, S. & Schliep, K. Life stressors, hypertensive disorders of pregnancy, and preterm birth. J. Psychosom. Obstet. Gynaecol. 43, 42–50 (2022).
Christian, L. M. & Porter, K. Longitudinal changes in serum proinflammatory markers across pregnancy and postpartum: effects of maternal body mass index. Cytokine 70, 134–140 (2014).
Gillespie, S. L., Porter, K. & Christian, L. M. Adaptation of the inflammatory immune response across pregnancy and postpartum in Black and White women. J. Reprod. Immunol. 114, 27–31 (2016).
Mead, E. C. et al. The Role of Genetics in Preterm Birth. Reprod. Sci. 30, 3410–3427 (2023).
Di Renzo, G. C., Tosto, V. & Giardina, I. The biological basis and prevention of preterm birth. Best. Pr. Res Clin. Obstet. Gynaecol. 52, 13–22 (2018).
Kullo, I. J. et al. Complement Receptor 1 Gene Variants Are Associated with Erythrocyte Sedimentation Rate. Am. J. Hum. Genet. 89, 131–138 (2011).
Soto, E. et al. Anaphylatoxins in preterm and term labor. J. Perinat. Med 33, 306–313 (2005).
Vaisbuch, E. et al. Activation of the alternative pathway of complement is a feature of preterm parturition but not of spontaneous labor at term. Am. J. Reprod. Immunol. 63, 318–330 (2010).
Jiang, C. et al. Longitudinal changes of oxidative stress and PON1 lactonase activity and status in older pregnant women undergoing assisted reproductive technology: a prospective nested case-control study. Reprod. Biol. Endocrinol. 21, 97 (2023).
Byrns, M. C. Regulation of progesterone signaling during pregnancy: implications for the use of progestins for the prevention of preterm birth. J. Steroid Biochem Mol. Biol. 139, 173–181 (2014).
Wetendorf, M. & DeMayo, F. J. Progesterone receptor signaling in the initiation of pregnancy and preservation of a healthy uterus. Int J. Dev. Biol. 58, 95–106 (2014).
Yellon, S. M. et al. Loss of progesterone receptor-mediated actions induce preterm cellular and structural remodeling of the cervix and premature birth. PLoS One 8, e81340 (2013).
Du, S., Trakooljul, N., Schoen, J. & Chen, S. Does Maternal Stress Affect the Early Embryonic Microenvironment? Impact of Long-Term Cortisol Stimulation on the Oviduct Epithelium. Int J. Mol. Sci. 21, 443 (2020).
Sferruzzi-Perri, A. N. et al. Early pregnancy maternal endocrine insulin-like growth factor I programs the placenta for increased functional capacity throughout gestation. Endocrinology 148, 4362–4370 (2007).
Demendi, C. et al. Gene expression patterns of insulin-like growth factor 1, 2 (IGF-1, IGF-2) and insulin-like growth factor binding protein 3 (IGFBP-3) in human placenta from preterm deliveries: influence of additional factors. Eur. J. Obstet. Gynecol. Reprod. Biol. 160, 40–44 (2012).
Lo, H. C. et al. Relation of cord serum levels of growth hormone, insulin-like growth factors, insulin-like growth factor binding proteins, leptin, and interleukin-6 with birth weight, birth length, and head circumference in term and preterm neonates. Nutrition 18, 604–608 (2002).
Nwachukwu, C. U., Robinson, R. S. & Woad, K. J. Effect of insulin-like growth factor system on luteinising angiogenesis. Reprod. Fertil. 4, e220057 (2023).
Mazziotti, G. & Giustina, A. Glucocorticoids and the regulation of growth hormone secretion. Nat. Rev. Endocrinol. 9, 265–276 (2013).
Mackness, M. I., Arrol, S., Abbott, C. & Durrington, P. N. Protection of low-density lipoprotein against oxidative modification by high-density lipoprotein associated paraoxonase. Atherosclerosis 104, 129–135 (1993).
Mackness, M. I., Mackness, B., Durrington, P. N., Connelly, P. W. & Hegele, R. A. Paraoxonase: biochemistry, genetics and relationship to plasma lipoproteins. Curr. Opin. Lipido. 7, 69–76 (1996).
Chen, D. et al. Polymorphisms of the paraoxonase gene and risk of preterm delivery. Epidemiology 15, 466–470 (2004).
Acknowledgements
The authors would like to thank the health care team at Maternidad Nuestra Señora de la Merced, Tucumán, Argentina, for their hard work and support and to Mariana Piola and Alejandra Mariona at ECLAMC who provided technical support.
Funding
The research program was supported by Agencia Nacional de Promoción Científica y Tecnológica (ANPCyT-MINCyT), grant numbers PICT-2018-4275 (PI: López Camelo JS) and PICT-2018-4285 (PI: Lucas G. Gimenez), Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), and INAGEMP [Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq)] grant 465549/2014-4, Brazil.
Author information
Authors and Affiliations
Contributions
S.L.H., M.R.S., J.S.L.C., and L.G.G. made substantial contributions to design, acquisition of data, analysis and interpretation of data, drafting the article and approving the final manuscript as submitted. H.K., S.M.M., M.L.R., G.L., J.S.L.C., and L.G.G. made substantial contributions to design, acquisition of data, critical manuscript revision for important intellectual content, and approving of the final version as submitted. S.L.H., M.R.S., M.N.M., H.K., S.M.M., M.L.R., G.L., J.S.L.C., and L.G.G. made contributions to data analysis and interpretation, drafting and editing of the article, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Before enrollment, signed informed consent was obtained from all participating families. Parents provided consent for themselves and for the neonates.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heisecke, S.L., Santos, M.R., Malbrán, M.N. et al. Environmental and genetic risk factors for preterm birth: interplays with stressful events during pregnancy. Pediatr Res 98, 2153–2159 (2025). https://doi.org/10.1038/s41390-025-04047-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-04047-4