Abstract
Over the last two decades, significant progress has been made in the management of neonatal encephalopathy due to presumed hypoxic-ischemic encephalopathy. One key area that requires improvement is timely and accurate neuroprognostication in this population to identify infants who may benefit from early interventions and harness the maximum neuroplastic capacity of the developing brain. Improved neuroprognostication also has the potential to foster more effective communication of findings to caregivers. In this review, we explore whether improved neuroprognostication is possible by assessing clinical, biochemical, electrographic, neurophysiological, and neuroimaging biomarkers and their role in neuroprognostication.
Impact statement
-
Over the last two decades, significant progress has been made in the management of neonatal encephalopathy due to presumed hypoxic-ischemic encephalopathy. One key area that requires improvement is timely and accurate neuroprognostication in this population to identify infants who may benefit from early interventions and harness the maximum neuroplastic capacity of the developing brain.
-
In this review article, we discuss general concepts and principles of neuroprognostication and the role of each prognostic marker.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Branagan, A., Molloy, E. J., Badawi, N. & Nelson, K. B. Causes and terminology in neonatal encephalopathy: what is in a name? Neonatal encephalopathy, hypoxic-ischemic encephalopathy or perinatal asphyxia. Clin. Perinatol. 51, 521–534 (2024).
Collaborators, G. B. D. S. R. F. Global, regional, and national burden of stroke and its risk factors, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 23, 973–1003 (2024).
Gunn, A. J. & Thoresen, M. Neonatal encephalopathy and hypoxic-ischemic encephalopathy. Handb. Clin. Neurol. 162, 217–237 (2019).
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. 2013, CD003311 (2013).
Douglas-Escobar, M. & Weiss, M. D. Hypoxic-ischemic encephalopathy: a review for the clinician. JAMA Pediatr. 169, 397–403 (2015).
Steinman, K. J. et al. Neonatal watershed brain injury on magnetic resonance imaging correlates with verbal IQ at 4 years. Pediatrics 123, 1025–1030 (2009).
Lee-Kelland, R. et al. School-age outcomes of children without cerebral palsy cooled for neonatal hypoxic-ischaemic encephalopathy in 2008-2010. Arch. Dis. Child Fetal Neonatal Ed. 105, 8–13 (2020).
Robertsson Grossmann, K., Eriksson Westblad, M., Blennow, M. & Lindstrom, K. Outcome at early school age and adolescence after hypothermia-treated hypoxic-ischaemic encephalopathy: an observational, population-based study. Arch. Dis. Child Fetal Neonatal Ed. 108, 295–301 (2023).
Lee, K. S. et al. Practice variations for therapeutic hypothermia in neonates with hypoxic-ischemic encephalopathy: an international survey. J. Pediatr. 274, 114181 (2024).
Beltempo, M. et al. Variations in practices and outcomes of neonates with hypoxic ischemic encephalopathy treated with therapeutic hypothermia across tertiary nicus in Canada. J. Perinatol. 42, 898–906 (2022).
Cawley, P. & Chakkarapani, E. Fifteen-minute consultation: therapeutic hypothermia for infants with hypoxic ischaemic encephalopathy-translating jargon, prognosis and uncertainty for parents. Arch. Dis. Child Educ. Pr. Ed. 105, 75–83 (2020).
Christensen, R., de Vries, L. S. & Cizmeci, M. N. Neuroimaging to guide neuroprognostication in the neonatal intensive care unit. Curr. Opin. Pediatr. 36, 190–197 (2024).
Goswami, I., Guillot, M. & Tam, E. W. Y. Predictors of long-term neurodevelopmental outcome of hypoxic-ischemic encephalopathy treated with therapeutic hypothermia. Semin Neurol. 40, 322–334 (2020).
Einspieler, C. et al. Cerebral palsy: early markers of clinical phenotype and functional outcome. J. Clin. Med. 8, 1–27 (2019).
Romeo, D. M. et al. Hammersmith infant neurological examination in infants born at term: predicting outcomes other than cerebral palsy. Dev. Med. Child Neurol. 64, 871–880 (2022).
Christensen, R., Miller, S. P. & Gomaa, N. A. Home-ICS: how experiences of the home impact biology and child neurodevelopmental outcomes. Pediatr. Res. 96, 1475–1483 (2024).
Merchant, N. & Azzopardi, D. Early predictors of outcome in infants treated with hypothermia for hypoxic-ischaemic encephalopathy. Dev. Med. Child Neurol. 57 (Suppl 3), 8–16 (2015).
Bonifacio, S. L. & Hutson, S. The term newborn: evaluation for hypoxic-ischemic encephalopathy. Clin. Perinatol. 48, 681–695 (2021).
Glass, H. C. et al. Predictors of death or severe impairment in neonates with hypoxic-ischemic encephalopathy. JAMA Netw. Open 7, e2449188 (2024).
Laptook, A. R. et al. Outcome of term infants using Apgar scores at 10 min following hypoxic-ischemic encephalopathy. Pediatrics 124, 1619–1626 (2009).
Natarajan, G. et al. Apgar scores at 10 min and outcomes at 6-7 years following hypoxic-ischaemic encephalopathy. Arch. Dis. Child Fetal Neonatal Ed. 98, F473–F479 (2013).
Kasdorf, E., Laptook, A., Azzopardi, D., Jacobs, S. & Perlman, J. M. Improving infant outcome with a 10 min Apgar of 0. Arch. Dis. Child Fetal Neonatal Ed. 100, F102–F105 (2015).
Shibasaki, J. et al. Outcomes related to 10-min Apgar scores of zero in Japan. Arch. Dis. Child Fetal Neonatal Ed. 105, 64–68 (2020).
Shah, P., Anvekar, A., McMichael, J. & Rao, S. Outcomes of infants with Apgar score of zero at 10 min: the West Australian Experience. Arch. Dis. Child Fetal Neonatal Ed. 100, F492–F494 (2015).
Natarajan, G. et al. Prediction of 18 to 22 month neurodevelopmental outcomes using the numerical Sarnat score compared with modified Sarnat staging in infants with moderate to severe hypoxic-ischemic encephalopathy. J. Pediatr. 281, 114522 (2025).
Gunn, A. J. et al. Therapeutic hypothermia changes the prognostic value of clinical evaluation of neonatal encephalopathy. J. Pediatr. 152, 55–58.e51 (2008).
Rutherford, M. et al. Assessment of brain tissue injury after moderate hypothermia in neonates with hypoxic-ischaemic encephalopathy: a nested substudy of a randomised controlled trial. Lancet Neurol. 9, 39–45 (2010).
Shankaran, S. et al. Evolution of encephalopathy during whole body hypothermia for neonatal hypoxic-ischemic encephalopathy. J. Pediatr. 160, 567–572.e563 (2012).
Lally, P. J. et al. Magnetic resonance spectroscopy assessment of brain injury after moderate hypothermia in neonatal encephalopathy: a prospective multicentre cohort study. Lancet Neurol. 18, 35–45 (2019).
Al Balushi, A. et al. Hypotension and brain injury in asphyxiated newborns treated with hypothermia. Am. J. Perinatol. 35, 31–38 (2018).
More, K. S. et al. Cardiovascular associations with abnormal brain magnetic resonance imaging in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia and rewarming. Am. J. Perinatol. 35, 979–989 (2018).
Agarwal, P. et al. Outcomes of infants with hypoxic ischemic encephalopathy and persistent pulmonary hypertension of the newborn: results from three NICHD studies. J. Perinatol. 41, 502–511 (2021).
Pappas, A. et al. Hypocarbia and adverse outcome in neonatal hypoxic-ischemic encephalopathy. J. Pediatr. 158, 752–758.e751 (2011).
Beken, S. et al. Can biochemical markers predict the severity of hypoxic-ischemic encephalopathy? Turk. J. Pediatr. 56, 62–68 (2014).
Murray, D. M. et al. Persistent lactic acidosis in neonatal hypoxic-ischaemic encephalopathy correlates with EEG grade and electrographic seizure burden. Arch. Dis. Child Fetal Neonatal Ed. 93, F183–F186 (2008).
Michniewicz, B. et al. Biomarkers in newborns with hypoxic-ischemic encephalopathy treated with therapeutic hypothermia. Childs Nerv. Syst. 36, 2981–2988 (2020).
Kamino, D. et al. Severity and duration of dysglycemia and brain injury among patients with neonatal encephalopathy. EClinicalMedicine 58, 101914 (2023).
Basu, S. K. et al. Hypoglycaemia and hyperglycaemia are associated with unfavourable outcome in infants with hypoxic ischaemic encephalopathy: a post hoc analysis of the coolcap study. Arch. Dis. Child Fetal Neonatal Ed. 101, F149–F155 (2016).
Lagace, M. & Tam, E. W. Y. Neonatal dysglycemia: a review of dysglycemia in relation to brain health and neurodevelopmental outcomes. Pediatr. Res. 96, 1429–1437 (2024).
Graham, E. M., Burd, I., Everett, A. D. & Northington, F. J. Blood biomarkers for evaluation of perinatal encephalopathy. Front. Pharmacol. 7, 196 (2016).
Graham, E. M., Everett, A. D., Delpech, J. C. & Northington, F. J. Blood biomarkers for evaluation of perinatal encephalopathy: state of the art. Curr. Opin. Pediatr. 30, 199–203 (2018).
Del Rio et al. Amplitude integrated electroencephalogram as a prognostic tool in neonates with hypoxic-ischemic encephalopathy: a systematic review. PLoS ONE 11, e0165744 (2016).
Chandrasekaran, M., Chaban, B., Montaldo, P. & Thayyil, S. Predictive value of amplitude-integrated EEG (AEEG) after rescue hypothermic neuroprotection for hypoxic ischemic encephalopathy: a meta-analysis. J. Perinatol. 37, 684–689 (2017).
Thoresen, M., Hellstrom-Westas, L., Liu, X. & de Vries, L. S. Effect of hypothermia on amplitude-integrated electroencephalogram in infants with asphyxia. Pediatrics 126, e131–e139 (2010).
Meder, U. et al. Longitudinal analysis of amplitude-integrated electroencephalography for outcome prediction in hypoxic-ischemic encephalopathy. J. Pediatr. 246, 19–25.e15 (2022).
Rondagh, M. et al. Longitudinal analysis of amplitude-integrated electroencephalography for outcome prediction in infants with hypoxic-ischemic encephalopathy: a validation study. J. Pediatr. 277, 114407 (2024).
Fitzgerald, M. P., Massey, S. L., Fung, F. W., Kessler, S. K. & Abend, N. S. High electroencephalographic seizure exposure is associated with unfavorable outcomes in neonates with hypoxic-ischemic encephalopathy. Seizure 61, 221–226 (2018).
Kharoshankaya, L. et al. Seizure burden and neurodevelopmental outcome in neonates with hypoxic-ischemic encephalopathy. Dev. Med. Child Neurol. 58, 1242–1248 (2016).
Alharbi, H. M. et al. Seizure burden and neurologic outcomes after neonatal encephalopathy. Neurology 100, e1976–e1984 (2023).
Toet, M. C., Lemmers, P. M., van Schelven, L. J. & van Bel, F. Cerebral oxygenation and electrical activity after birth asphyxia: their relation to outcome. Pediatrics 117, 333–339 (2006).
Nakamura, S. et al. Simultaneous measurement of cerebral hemoglobin oxygen saturation and blood volume in asphyxiated neonates by near-infrared time-resolved spectroscopy. Brain Dev. 37, 925–932 (2015).
Goeral, K. et al. Prediction of outcome in neonates with hypoxic-ischemic encephalopathy II: role of amplitude-integrated electroencephalography and cerebral oxygen saturation measured by near-infrared spectroscopy. Neonatology 112, 193–202 (2017).
Lemmers, P. M. et al. Cerebral oxygenation and brain activity after perinatal asphyxia: does hypothermia change their prognostic value? Pediatr. Res. 74, 180–185 (2013).
Niezen, C. K., Bos, A. F., Sival, D. A., Meiners, L. C. & Ter Horst, H. J. Amplitude-integrated EEG and cerebral near-infrared spectroscopy in cooled, asphyxiated infants. Am. J. Perinatol. 35, 904–910 (2018).
Agudelo-Perez, S. et al. Cerebral rScO2 measured by near-infrared spectroscopy (NIRS) during therapeutic hypothermia in neonates with hypoxic-ischemic encephalopathy: a systematic review. J. Mother Child 28, 33–44 (2024).
Nevalainen, P. et al. Towards multimodal brain monitoring in asphyxiated newborns with amplitude-integrated EEG and simultaneous somatosensory evoked potentials. Early Hum. Dev. 153, 105287 (2021).
Vanhatalo, S. & Lauronen, L. Neonatal sep - back to bedside with basic science. Semin. Fetal Neonatal Med. 11, 464–470 (2006).
Lagace, M. et al. Automated assessment of EEG background for neurodevelopmental prediction in neonatal encephalopathy. Ann. Clin. Transl. Neurol. 11, 3267–3279 (2024).
Groenendaal, F. & de Vries, L. S. Fifty years of brain imaging in neonatal encephalopathy following perinatal asphyxia. Pediatr. Res. 81, 150–155 (2017).
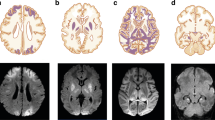
Wisnowski, J. L. et al. Neuroimaging in the term newborn with neonatal encephalopathy. Semin. Fetal Neonatal Med. 26, 101304 (2021).
Chau, V. et al. Comparison of computer tomography and magnetic resonance imaging scans on the third day of life in term newborns with neonatal encephalopathy. Pediatrics 123, 319–326 (2009).
Barnette, A. R. et al. Neuroimaging in the evaluation of neonatal encephalopathy. Pediatrics 133, e1508–e1517 (2014).
Eken, P., Jansen, G. H., Groenendaal, F., Rademaker, K. J. & de Vries, L. S. Intracranial lesions in the fullterm infant with hypoxic ischaemic encephalopathy: ultrasound and autopsy correlation. Neuropediatrics 25, 301–307 (1994).
Cizmeci, M. N. et al. Neonatal hypoxic-ischemic encephalopathy spectrum: severity-stratified analysis of neuroimaging modalities and association with neurodevelopmental outcomes. J. Pediatr. 266, 113866 (2024).
Annink, K. V. et al. The development and validation of a cerebral ultrasound scoring system for infants with hypoxic-ischaemic encephalopathy. Pediatr. Res. 87, 59–66 (2020).
Fox, A. et al. Utility of cranial ultrasound to investigate brain injury in hypoxic-ischemic encephalopathy. Pediatr. Neurol. 163, 15–20 (2024).
Parmentier, C. E. J., de Vries, L. S. & Groenendaal, F. Magnetic resonance imaging in (near-)term infants with hypoxic-ischemic encephalopathy. Diagnostics 12, 1–18 (2022).
Liu, W. et al. Prognostic value of clinical tests in neonates with hypoxic-ischemic encephalopathy treated with therapeutic hypothermia: a systematic review and meta-analysis. Front. Neurol. 11, 133 (2020).
Goergen, S. K. et al. Early MRI in term infants with perinatal hypoxic-ischaemic brain injury: interobserver agreement and MRI predictors of outcome at 2 years. Clin. Radio. 69, 72–81 (2014).
Calabrese, E. et al. Correlating quantitative MRI-based apparent diffusion coefficient metrics with 24-month neurodevelopmental outcomes in neonates from the heal trial. Radiology 308, e223262 (2023).
Lambing, H. et al. Using neonatal magnetic resonance imaging to predict gross motor disability at four years in term-born children with neonatal encephalopathy. Pediatr. Neurol. 144, 50–55 (2023).
Martinez-Biarge, M., Diez-Sebastian, J., Rutherford, M. A. & Cowan, F. M. Outcomes after central grey matter injury in term perinatal hypoxic-ischaemic encephalopathy. Early Hum. Dev. 86, 675–682 (2010).
Lee, B. L. et al. Long-term cognitive outcomes in term newborns with watershed injury caused by neonatal encephalopathy. Pediatr. Res 92, 505–512 (2022).
Martinez-Biarge, M. et al. White matter and cortical injury in hypoxic-ischemic encephalopathy: antecedent factors and 2-year outcome. J. Pediatr. 161, 799–807 (2012).
Harteman, J. C. et al. Diffusion-weighted imaging changes in cerebral watershed distribution following neonatal encephalopathy are not invariably associated with an adverse outcome. Dev. Med. Child Neurol. 55, 642–653 (2013).
Inder, T. E. et al. Neuroimaging of the preterm brain: review and recommendations. J. Pediatr. 237, 276–287.e274 (2021).
Hayman, M. et al. Punctate white-matter lesions in the full-term newborn: underlying aetiology and outcome. Eur. J. Paediatr. Neurol. 23, 280–287 (2019).
Wu, Y. W. et al. How well does neonatal neuroimaging correlate with neurodevelopmental outcomes in infants with hypoxic-ischemic encephalopathy? Pediatr. Res. 94, 1018–1025 (2023).
Wu, Y. W. et al. Advancing brain MRI as a prognostic indicator in hypoxic-ischemic encephalopathy. Pediatr. Res. 95, 587–589 (2024).
Li, A. M. et al. White matter injury in term newborns with neonatal encephalopathy. Pediatr. Res. 65, 85–89 (2009).
Lemmon, M. E. et al. Diffusion tensor imaging detects occult cerebellar injury in severe neonatal hypoxic-ischemic encephalopathy. Dev. Neurosci. 39, 207–214 (2017).
Annink, K. V. et al. Cerebellar injury in term neonates with hypoxic-ischemic encephalopathy is underestimated. Pediatr. Res. 89, 1171–1178 (2021).
Raghu, K. et al. Prognostic indicators of reorientation of care in perinatal hypoxic-ischemic encephalopathy spectrum. J. Pediatr. 276, 114273 (2024).
Barkovich, A. J. et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR Am. J. Neuroradiol. 19, 143–149 (1998).
Shankaran, S. et al. Brain injury following trial of hypothermia for neonatal hypoxic-ischaemic encephalopathy. Arch. Dis. Child Fetal Neonatal Ed. 97, F398–F404 (2012).
Shankaran, S. et al. Nichd magnetic resonance brain imaging score in term infants with hypoxic-ischemic encephalopathy: a secondary analysis of a randomized clinical trial. JAMA Pediatr. (2025). Online ahead of print.
Trivedi, S. B. et al. A validated clinical MRI injury scoring system in neonatal hypoxic-ischemic encephalopathy. Pediatr. Radio. 47, 1491–1499 (2017).
Weeke, L. C. et al. A novel magnetic resonance imaging score predicts neurodevelopmental outcome after perinatal asphyxia and therapeutic hypothermia. J. Pediatr. 192, 33–40.e32 (2018).
Ni Bhroin, M. et al. Relationship between MRI scoring systems and neurodevelopmental outcome at two years in infants with neonatal encephalopathy. Pediatr. Neurol. 126, 35–42 (2022).
Molavi, M., Vann, S. D., de Vries, L. S., Groenendaal, F. & Lequin, M. Signal change in the mammillary bodies after perinatal asphyxia. AJNR Am. J. Neuroradiol. 40, 1829–1834 (2019).
Spencer, A. P. C. et al. Mammillary body abnormalities and cognitive outcomes in children cooled for neonatal encephalopathy. Dev. Med. Child Neurol. 65, 792–802 (2023).
Cizmeci, M. N., Martinez-Biarge, M. & Cowan, F. M. The predictive role of brain magnetic resonance imaging in neonates with hypoxic-ischemic encephalopathy. Pediatr. Res. 95, 601–602 (2024).
Ward, P. et al. Reduced fractional anisotropy on diffusion tensor magnetic resonance imaging after hypoxic-ischemic encephalopathy. Pediatrics 117, e619–e630 (2006).
Porter, E. J., Counsell, S. J., Edwards, A. D., Allsop, J. & Azzopardi, D. Tract-based spatial statistics of magnetic resonance images to assess disease and treatment effects in perinatal asphyxial encephalopathy. Pediatr. Res. 68, 205–209 (2010).
Van Steenis, A. et al. Individualized neuroprognostication in neonates with hypoxic-ischemic encephalopathy treated with hypothermia. Neurol. Clin. Pract. 15, e200370 (2025).
Chalak, L. F. et al. Mild hie and therapeutic hypothermia: gaps in knowledge with under-powered trials. Pediatr. Res. (2024). Online ahead of print.
Chalak, L. F., Slaughter, J. L., King, W. C., Sepulveda, P. & Wisniewski, S. R. A new horizon for understanding the comparative effectiveness for cooling prospectively infants with mild encephalopathy. Clin. Perinatol. 51, 605–616 (2024).
Pappas, A., Milano, G. & Chalak, L. F. Hypoxic-ischemic encephalopathy: changing outcomes across the spectrum. Clin. Perinatol. 50, 31–52 (2023).
Funding
No funding was secured for this study. M.N.C. is supported by the Dr. Karen Pape Program in Neuroplasticity for neuroprognostication research.
Author information
Authors and Affiliations
Contributions
MNC conceptualized the review article, designed the manuscript, analyzed and interpreted the data in the literature, drafted the article, and approved the final version to be published. RC critically reviewed the article and approved the final version to be published. AvS critically reviewed the article and approved the final version to be published. LSdV analyzed and interpreted the data in the literature, critically reviewed the article, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cizmeci, M.N., Christensen, R., van Steenis, A. et al. Neuroprognostication in neonatal encephalopathy due to presumed hypoxic-ischemic encephalopathy. Pediatr Res 98, 2459–2470 (2025). https://doi.org/10.1038/s41390-025-04058-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-04058-1
This article is cited by
-
The future of neurodevelopmental disabilities
Pediatric Research (2025)
-
Beyond brain injury: rethinking neurodevelopment in neonatal encephalopathy
Pediatric Research (2025)
-
From differential to definitive: diagnosing and treatment of neonatal encephalopathy
Pediatric Research (2025)
-
Advancing neuroprognostication in neonatal encephalopathy: promise and limitations of diffusion kurtosis imaging
Pediatric Research (2025)