Abstract
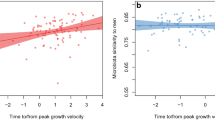
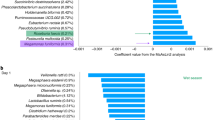
Central precocious puberty (CPP) is a condition that affects prepubertal children, particularly girls. Recent evidence suggests an association between the gut microbiome (GM) and CPP. This study aims to explore this association. We analyzed data from studies investigating the association between GM and CPP. Various databases were searched for relevant articles published from database inception to December 31, 2023. Standardized mean difference values were calculated and depicted in forest plots. Furthermore, subgroup analyses by type of study subject (animals vs. humans) were performed. The final analysis included 9 studies. Five were human studies, whereas the remaining four were animal (rats or mice) studies. In the precocious puberty group, the abundances (at the genus level) of Holdemania, Roseburia, Alistipes, Dialister, Enterococcus, Ruminococcus, Bilophila, and Lachnoclostridium increased significantly, whereas those of Bacteroides, Anaerostipes, Megamonas, and Gemella decreased significantly. Furthermore, for this group, the Shannon index for alpha diversity was increased in human studies and decreased in animal studies compared to the control group. Notably, the levels of major short-chain fatty acids, butyric and propionic acids, were significantly reduced in the precocious puberty group. There was an association between CPP and GM. Both subgroups revealed that microbiome profiles vary across individuals with precocious puberty.
Impact
-
To our knowledge, this is the first systematic review and meta-analysis to explore the association between the gut microbiome and precocious puberty in both human and animal models.
-
Our findings reveal distinct microbial patterns in individuals with CPP, including consistent alterations in 12 bacterial genera and significant changes in short-chain fatty acid levels.
-
By identifying reproducible microbial signatures and metabolites associated with CPP, this study lays the groundwork for microbiome-targeted interventions alongside traditional hormonal therapies.
-
The study addresses key methodological inconsistencies in existing literature, highlighting the need for standardized protocols in future research on the gut-puberty axis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data were extracted from papers and supplementary information published online. All data are available online. The data sets used in the present study are also available from the corresponding author upon reasonable request.
References
Léger, J. & Carel, J. C. Central precocious puberty - management and long-term outcomes. Eur. Endocrinol. 11, 45–46 (2015).
Aguirre, R. S. & Eugster, E. A. Central precocious puberty: from genetics to treatment. Best. Pr. Res. Clin. Endocrinol. Metab. 32, 343–354 (2018).
Latronico, A. C., Brito, V. N. & Carel, J. C. Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol. 4, 265–274 (2016).
Huang, X. et al. Gut microbiome combined with metabolomics reveals biomarkers and pathways in central precocious puberty. J. Transl. Med. 21, 316 (2023).
Yue, M. & Zhang, L. Exploring the mechanistic interplay between gut microbiota and precocious puberty: a narrative review. Microorganisms 12, 323 (2024).
Shi, L., Jiang, Z. & Zhang, L. Childhood obesity and central precocious puberty. Front. Endocrinol.13, 1056871 (2022).
Shim, Y. S., Lee, H. S. & Hwang, J. S. Genetic factors in precocious puberty. Clin. Exp. Pediatr. 65, 172–181 (2022).
Bo, T. et al. Effects of high-fat diet during childhood on precocious puberty and gut microbiota in mice. Front. Microbiol. 13, 930747 (2022).
Carel, J. C. & Léger, J. Clinical practice. Precocious puberty. N. Engl. J. Med. 358, 2366–2377 (2008).
Hou, K. et al. Microbiota in health and diseases. Signal. Transduct. Target. Ther. 7, 135 (2022).
Ursell, L. K. et al. The intestinal metabolome: an intersection between microbiota and host. Gastroenterology 146, 1470–1476 (2014).
Sisk-Hackworth, L., Kelley, S. T. & Thackray, V. G. Sex, puberty, and the gut microbiome. Reproduction 165, R61–R74 (2023).
Bistoletti, M., Bosi, A., Banfi, D., Giaroni, C. & Baj, A. The microbiota-gut-brain axis: focus on the fundamental communication pathways. Prog. Mol. Biol. Transl. Sci. 176, 43–110 (2020).
Dinan, T. G. & Cryan, J. F. The microbiome-gut-brain axis in health and disease. Gastroenterol. Clin. North Am. 46, 77–89 (2017).
Wang, L., Xu, H., Tan, B. & Tian, J. Gut microbiota and its derived scfas regulate the hpga to reverse obesity-induced precocious puberty in female rats. Front. Endocrinol. 13, 1051797 (2022).
Nguyen, N. N. et al. Natural sweetener glycyrrhizin protects against precocious puberty by modulating the gut microbiome. Life Sci. 350, 122789–122789 (2024).
Wang, M. et al. Microbial reconstitution reverses early female puberty induced by maternal high-fat diet during lactation. Endocrinology 161, bqz041 (2020).
Yuan, X., Shangguan, H., Zhang, Y., Lin, X. & Chen, R. Intervention effect of probiotics on the early onset of puberty induced by daidzein in female mice. Mol. Nutr. Food Res. 67, 2200501 (2023).
Li, Y. et al. Altered nitric oxide induced by gut microbiota reveals the connection between central precocious puberty and obesity. Clin. Transl. Med. 11, e299 (2021).
Huang, C. et al. Distinct gut microbiota structure and function of children with idiopathic central and peripheral precocious puberty. Int. J. Endocrinol. 2022, 7175250 (2022).
Huang, L. et al. Critical body fat percentage required for puberty onset: the Taiwan pubertal longitudinal study. J. Endocrinol. Investig. 46, 1177–1185 (2023).
Wang, J. S. et al. Evaluation of a technological image-based dietary assessment tool for children during pubertal growth: a pilot study. Nutrients 11, 2527 (2019).
Nguyen, N. T. K. et al. Lipidomics reveals ceramide biomarkers for detecting central precocious puberty in girls. Obes. Res. Clin. Pr. 18, 269–279 (2024).
Gunawan, S. P. et al. Sleep deprivation alters pubertal timing in humans and rats: the role of the gut microbiome. Sleep 47, zsad308 (2024).
Dong, G. et al. The association of gut microbiota with idiopathic central precocious puberty in girls. Front. Endocrinol. 10, 941 (2019).
Hooijmans, C. R. et al. Syrcle’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 14, 43 (2014).
Calcaterra, V. et al. Precocious puberty and microbiota: the role of the sex hormone-gut microbiome axis. Front. Endocrinol. 13, 1000919 (2022).
Yoon, K. & Kim, N. Roles of sex hormones and gender in the gut microbiota. J. Neurogastroenterol. Motil. 27, 314 (2021).
Yuan, X., Chen, R., Zhang, Y., Lin, X. & Yang, X. Sexual dimorphism of gut microbiota at different pubertal status. Micro. Cell Fact. 19, 152 (2020).
Qian, H. et al. Impact of exercise training on gut microbiome imbalance in obese individuals: a study based on Mendelian randomization analysis. Front. Physiol. 14, 1264931 (2024).
Valsamakis, G., Arapaki, A., Balafoutas, D., Charmandari, E. & Vlahos, N. F. Diet-induced hypothalamic inflammation, phoenixin, and subsequent precocious puberty. Nutrients 13, 3460 (2021).
Lladó Fernández, S., Větrovský, T. & Baldrian, P. The concept of operational taxonomic units revisited: genomes of bacteria that are regarded as closely related are often highly dissimilar. Folia Microbiol. 64, 19–23 (2019).
He, Y. et al. Comparison of microbial diversity determined with the same variable tag sequence extracted from two different PCR amplicons. BMC Microbiol. 13, 208 (2013).
Yuan, X., Chen, R., Zhang, Y., Lin, X. & Yang, X. Gut microbiota: effect of pubertal status. BMC Microbiol. 20, 334 (2020).
Murugesan, S. et al. Study of the diversity and short-chain fatty acids production by the bacterial community in overweight and obese Mexican children. Eur. J. Clin. Microbiol. Infect. Dis. 34, 1337–1346 (2015).
Vital, M., Karch, A. & Pieper, D. H. Colonic butyrate-producing communities in humans: an overview using omics data. Msystems 2, https://doi.org/10.1128/msystems.00130-00117 (2017).
Heimesaat, M. M. et al. Comprehensive postmortem analyses of intestinal microbiota changes and bacterial translocation in human flora associated mice. PLoS ONE 7, e40758 (2012).
Nakayama, J. et al. Diversity in gut bacterial community of school-age children in Asia. Sci. Rep. 5, 8397 (2015).
Stearns, J. C. et al. Ethnic and diet-related differences in the healthy infant microbiome. Genome Med. 9, 32 (2017).
Acknowledgements
This manuscript was edited by Wallace Academic Editing. We acknowledge the use of ChatGPT for refining the manuscript.
Funding
This study was supported by the National Science and Technology Council (grant numbers: MOST110-2628-B-038-014–111, NSTC 112-2628-B-038-005, NSTC 114-2622-B-038-003 [from Yang-Ching Chen]), as well as by the Taipei Medical University and National Defense University Medical Joint Research Program (114_T&N_04).
Author information
Authors and Affiliations
Contributions
Yang-Ching Chen: Conceptualization, Design, Manuscript revision, and Supervision. José Roberto Rodríguez Mazariegos: Systematic search, Study selection, Risk-of-bias assessment, Data extraction, Data analysis, Data interpretation, and Manuscript preparation—writing. Nguyen Nhat Nam: Systematic search, Study selection, Risk-of-bias assessment, Data extraction, and Manuscript revision. Tingbei Bo and Dehua Wang: Data collection. Jhih-Wei Hsu: Manuscript revision. All authors have reviewed and approved the final version of the manuscript and agreed to take responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related to directly or indirectly to the subject of this article.
Consent statement
This study synthesizes data from previously published research, no new data were collected from human participants. Specifically, no new data were collected from the TPLS for this meta-analysis. The data used from the TPLS were previously gathered as part of earlier IRB-approved studies. As a result, informed consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodríguez Mazariegos, J.R., Nam, N.N., Bo, T. et al. Precocious puberty and gut microbiome: a systematic review and meta-analysis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04180-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04180-0
This article is cited by
-
Too soon to grow: linking gut health to early puberty onset
Pediatric Research (2025)