Abstract
Objectives
To investigate the correlation between serum uric acid/creatinine ratio (SUA/Cr) and Metabolic-associated fatty liver disease (MAFLD) in children.
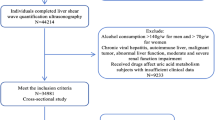
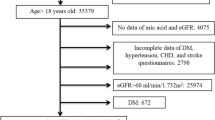
Methods
1387 participants aged 4–15 who underwent health examinations from 1/2020–12/2023 were included. Clinical indicators were compared and analyzed.
Results
Overweight/obese group had elevated levels compared to non-overweight/obese group in male proportion, uric acid (UA), serum uric acid/creatinine ratio (SUA/Cr), systolic blood pressure (SBP), diastolic blood pressure (DBP), alanine aminotransferase (ALT), gamma-glutamyltransferase(GGT), total protein(TP), albumin(ALB), globulin(GLO), and serum creatinine(SCr) (p < 0.001, Kruskal–Wallis test). As SUA/Cr increased, UA, ALT, ALP, TP, GGT levels and the prevalence rates of overweight/obesity rose, while SCr levels fell (p < 0.05, Jonckheere-Terpstra test), and positively related to body mass index (BMI) (p < 0.05). The OR for overweight/obesity increased in higher SUA/Cr quartile groups, as Q3 (OR = 2.399, 95% confidence interval CI = 1.554–3.703) and Q4 (OR = 5.044, 95% CI = 3.281–7.754). The SUA/Cr exhibited an AUC of 0.828 (95% CI = 0.764–0.892, p < 0.001) in predicting overweight/obesity and elevated ALT levels, with a specificity of 0.764 and sensitivity of 0. 805.
Conclusions
Children with overweight/obesity have higher liver enzymes, and elevated SUA/Cr levels may predict an increased incidence of overweight/obesity and hepatic injury.
Impact
-
This study found a close association between serum uric acid/creatinine ratio (SUA/Cr) and risk factors for Metabolic-associated fatty liver disease (MAFLD) in children.
-
SUA/Cr may be an indicator of risk factors for MAFLD in children.
-
Elevated SUA/Cr levels may predict an increased incidence of overweight/obesity and hepatic injury.
-
Providing an easily accessible non-invasive biomarker for predicting and preventing MAFLD in children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gofton, C., Upendran, Y., Zheng, M. H. & George, J. MAFLD: how is it different from NAFLD?. Clin. Mol. Hepatol. 29, S17–S31 (2023).
Rinella, M. E. et al. AASLD Practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 77, 1797–1835 (2023).
Lim, G. E. H. et al. An observational data meta-analysis on the differences in prevalence and risk factors between MAFLD vs NAFLD. Clin. Gastroenterol. Hepatol. 21, 619–629 (2023).
Chen, Y. L. et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: a cross-sectional comparative study. BMC Gastroenterol. 21, 212 (2021).
Le Garf, S., Nègre, V., Anty, R. & Gual, P. Metabolic fatty liver disease in children: a growing public health problem. Biomedicines 9, 1915 (2021).
Dikaiou, P. et al. Obesity, overweight and risk for cardiovascular disease and mortality in young women. Eur. J. Prev. Cardiol. 28, 1351–1359 (2021).
Collaboration, N. C. D. R. F. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 403, 1027–1050 (2024).
Lister, N. B. et al. Child and adolescent obesity. Nat. Rev. Dis. Prim. 9, 24 (2023).
Carrasquilla, G. D., Ängquist, L., Sørensen, T. I. A., Kilpeläinen, T. O. & Loos, R. J. F. Child-to-adult body size change and risk of type 2 diabetes and cardiovascular disease. Diabetologia 67, 864–873 (2024).
Di Cesare, M. et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 17, 212 (2019).
Okunogbe, A. et al. Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ Glob. Health 7, e009773 (2022).
Pan, X. F., Wang, L. & Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 9, 373–392 (2021).
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J. Hepatol. 73, 202–209 (2020).
Spiga, R. et al. Uric Acid Is Associated with inflammatory biomarkers and induces inflammation via activating the NF-κB signaling pathway in HepG2 cells. Arterioscler Thromb. Vasc. Biol. 37, 1241–1249 (2017).
Russo, E. et al. Fructose and uric acid: major mediators of cardiovascular disease risk starting at pediatric age. Int. J. Mol. Sci. 21, 4473 (2020).
Zeng, J. et al. Association between serum uric acid and obesity in Chinese adults: a 9-year longitudinal data analysis. BMJ Open 11, e041919 (2021).
Wang, A. et al. Metabolic Factors Mediate the Association between serum uric acid to serum creatinine ratio and cardiovascular disease. J. Am. Heart Assoc. 10, e023054 (2021).
Zeng, J. et al. Prevalence and incidence of MAFLD and associated anthropometric parameters among prepubertal children of the Shanghai Birth Cohort. Hepatol. Int. 17, 1416–1428 (2023).
Bergmann, K. et al. Diagnostic performance of biomarker-based scores as predictors of metabolic dysfunction-associated fatty liver disease risk in healthy children. Nutrients 15, 3667 (2023).
Deng, F. et al. Association between body mass index and serum uric acid: mediation analysis involving liver enzymes indicators. BMC Public Health 24, 3007 (2024).
She, D. et al. Serum uric acid to creatinine ratio and risk of metabolic syndrome in patients with overweight/obesity. Diabetes Metab. Syndr. Obes. 16, 3007–3017 (2023).
van Dam, M., Pottel, H., Delanaye, P. & Vreugdenhil, A. C. E. The evaluation of kidney function estimation during lifestyle intervention in children with overweight and obesity. Pediatr. Nephrol. 39, 3271–3278 (2024).
Miake, J. et al. Impact of hyper- and hypo-uricemia on kidney function. Biomedicines 11, 1258 (2023).
Su, M. et al. Metformin alleviates hyperuricaemia-induced serum FFA elevation and insulin resistance by inhibiting adipocyte hypertrophy and reversing suppressed white adipose tissue beiging. Clin. Sci. 134, 1537–1553 (2020).
Jiao, L. et al. The impact of chrysanthemi indici flos-enriched flavonoid part on the model of hyperuricemia based on inhibiting synthesis and promoting excretion of uric acid. J. Ethnopharmacol. 333, 118488 (2024).
Kawamoto, R., Kikuchi, A., Ninomiya, D., Tokumoto, Y. & Kumagi, T. Serum uric acid to creatinine ratio is a useful predictor of all-cause mortality among hypertensive patients. Clin. Hypertens. 29, 10 (2023).
Gill, D. et al. Urate, blood pressure, and cardiovascular disease: evidence from Mendelian randomization and meta-analysis of clinical trials. Hypertension 77, 383–392 (2021).
Sookoian, S. & Pirola, C. J. The serum uric acid/creatinine ratio is associated with nonalcoholic fatty liver disease in the general population. J. Physiol. Biochem. 79, 891–899 (2023).
Chen, L., Zhu, Z., Ye, S. & Zheng, M. The serum uric acid to serum creatinine ratio is an independent risk factor for diabetic kidney disease. Diabetes Metab. Syndr. Obes. 15, 3693–3703 (2022).
Acknowledgements
We thank Miaosang Xu and Chunsheng Wu for proving software support and development.
Author information
Authors and Affiliations
Contributions
Bi Chen collected data, drafted the initial manuscript, and critically reviewed and revised the manuscript for important intellectual content. Xiaoning Qu conceptualized the study, collected data, carried out the initial analyses, and critically reviewed and revised the manuscript for important intellectual content. Ting Li carried out the initial statistical analyses and critically reviewed and revised the manuscript. Minghua Jiang conceptualized and designed the study, reviewed, and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, B., Qu, X., Li, T. et al. Serum uric acid/creatinine ratio and metabolic-associated fatty liver disease risks in children. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04219-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04219-2