Abstract
Background and objective
Neonates with fetal inflammatory response (FIR) are at increased risk of early-onset sepsis and death. We aimed to determine whether FIR and its severity are associated with brain abnormalities on MRI at term-equivalent age in extremely preterm infants.
Methods
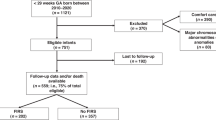
A prospective cohort study of extremely preterm infants born between 2018 to 2021 with MRI scans completed at term equivalent age. Brain injury was assessed using the Kidokoro scoring, with MRIs independently scored by two blinded readers and adjudicated by a third. FIR severity was classified per the Amsterdam Placental Workshop Group Consensus Statement.
Results
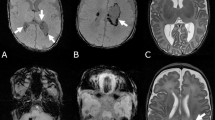
Among 141 infants, FIR was present in 59 (42%), with 46 (78%) having severe FIR ( ≥ stage 2). FIR was significantly associated with abnormal Kidokoro scores (P < 0.01), specifically white matter (P < 0.01) and cerebellar abnormalities (P = 0.01), but not cortical or deep gray matter abnormalities. Increasing FIR severity correlated with worse Kidokoro scores in both white and gray matter (P < 0.01). Other placental lesions showed no significant association. Inter-rater reliability was high (intraclass correlation coefficient >0.7).
Conclusion
This study is the first to link FIR severity to MRI brain abnormalities in extremely preterm infants, highlighting FIR as a risk factor for brain injury and delayed maturation.
Impact
-
Fetal Inflammatory Response (FIR) is associated with white matter and cerebellar injury by term-equivalent gestational age (TEA).
-
There is significant relationship between severity and progression of FIR and brain abnormalities by TEA.
-
This is the first study demonstrating the impact of progression and severity of FIR on abnormalities on MRI brain at term-equivalent gestational age.
-
These observations provide additional insight into understanding the impact of intrauterine exposure to inflammation on the brain injury in extremely preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Purisch, S. E. & Gyamfi-Bannerman, C. Epidemiology of preterm birth. Semin Perinatol. 41, 387–391 (2017).
Morgan, A. S., Mendonca, M., Thiele, N. & David, A. L. Management and outcomes of extreme preterm birth. BMJ 376, e055924 (2022).
Hillier, S. L., Krohn, M. A., Kiviat, N. B., Watts, D. H. & Eschenbach, D. A. Microbiologic causes and neonatal outcomes associated with chorioamnion infection. Am. J. Obstet. Gynecol. 165, 955–961 (1991).
Stinson, L. F. & Payne, M. S. Infection-mediated preterm birth: Bacterial origins and avenues for intervention. Aust. N. Z. J. Obstet. Gynaecol. 59, 781–790 (2019).
Klein, L. L. & Gibbs, R. S. Infection and preterm birth. Obstet. Gynecol. Clin. North Am. 32, 397–410 (2005).
Romero, R. et al. A fetal systemic inflammatory response is followed by the spontaneous onset of preterm parturition. Am. J. Obstet. Gynecol. 179, 186–193 (1998).
Jung, E. et al. The fetal inflammatory response syndrome: the origins of a concept, pathophysiology, diagnosis, and obstetrical implications. Semin Fetal Neonatal Med. 25, 101146 (2020).
Salas, A. A. et al. Histological characteristics of the fetal inflammatory response associated with neurodevelopmental impairment and death in extremely preterm infants. J. Pediatr. 163, 652–657.e651-652 (2013)
Patra, A., Huang, H., Bauer, J. A. & Giannone, P. J. Neurological consequences of systemic inflammation in the premature neonate. Neural Regen. Res. 12, 890–896 (2017).
Malaeb, S. & Dammann, O. Fetal inflammatory response and brain injury in the preterm newborn. J. Child Neurol. 24, 1119–1126 (2009).
Parikh, N. A. Advanced neuroimaging and its role in predicting neurodevelopmental outcomes in very preterm infants. Semin Perinatol. 40, 530–541 (2016).
Hintz, S. R. et al. Neuroimaging and neurodevelopmental outcome in extremely preterm infants. Pediatrics 135, e32–e42 (2015).
He, L. & Parikh, N. A. Atlas-guided quantification of white matter signal abnormalities on term-equivalent age MRI in very preterm infants: findings predict language and cognitive development at two years of age. PLoS One 8, e85475 (2013).
Kline, J. E. et al. Early cortical maturation predicts neurodevelopment in very preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 105, 460–465 (2020).
Van’t Hooft, J. et al. Predicting developmental outcomes in premature infants by term equivalent MRI: systematic review and meta-analysis. Syst. Rev. 4, 71 (2015).
Woodward, L. J., Anderson, P. J., Austin, N. C., Howard, K. & Inder, T. E. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N. Engl. J. Med 355, 685–694 (2006).
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M. & Anand, K. J. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA 288, 728–737 (2002).
Anderson, P. J., Cheong, J. L. & Thompson, D. K. The predictive validity of neonatal MRI for neurodevelopmental outcome in very preterm children. Semin Perinatol. 39, 147–158 (2015).
Chau, V. et al. Abnormal brain maturation in preterm neonates associated with adverse developmental outcomes. Neurology 81, 2082–2089 (2013).
He, L. et al. Early prediction of cognitive deficits in very preterm infants using functional connectome data in an artificial neural network framework. Neuroimage Clin. 18, 290–297 (2018).
Kidokoro, H., Neil, J. J. & Inder, T. E. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. AJNR Am. J. Neuroradiol. 34, 2208–2214 (2013).
Anderson, P. J. et al. Associations of Newborn Brain Magnetic Resonance Imaging with Long-Term Neurodevelopmental Impairments in Very Preterm Children. J. Pediatr. 187, 58–65.e51 (2017).
Thompson, D. K. et al. Tracking regional brain growth up to age 13 in children born term and very preterm. Nat. Commun. 11, 696 (2020).
Logan, J. W. et al. Adverse effects of perinatal illness severity on neurodevelopment are partially mediated by early brain abnormalities in infants born very preterm. J. Perinatol. 41, 519–527 (2021).
Jain, V. G. et al. Acute histologic chorioamnionitis independently and directly increases the risk for brain abnormalities seen on magnetic resonance imaging in very preterm infants. Am. J. Obstet. Gynecol. 227, 623.e621–623.e613 (2022).
Khong, T. Y. et al. Sampling and Definitions of Placental Lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab Med 140, 698–713 (2016).
Ibrahim, J., Mir, I. & Chalak, L. Brain imaging in preterm infants <32 weeks gestation: a clinical review and algorithm for the use of cranial ultrasound and qualitative brain MRI. Pediatr. Res 84, 799–806 (2018).
Greer, L. G. et al. An immunologic basis for placental insufficiency in fetal growth restriction. Am. J. Perinatol. 29, 533–538 (2012).
Mir, I. N. et al. Placental pathology is associated with severity of neonatal encephalopathy and adverse developmental outcomes following hypothermia. Am. J. Obstet. Gynecol. 213, 849.e841–847 (2015).
Redline, R. W., Heller, D., Keating, S. & Kingdom, J. Placental diagnostic criteria and clinical correlation-a workshop report. Placenta 26, S114–S117 (2005).
Alayli, Y. et al. Neurodevelopmental outcomes in extremely preterm infants with placental pathologic evidence of fetal inflammatroy response. Pediatr Res https://doi.org/10.1038/s41390-024-03391-1 (2024).
Para, R. et al. The Distinct Immune Nature of the Fetal Inflammatory Response Syndrome Type I and Type II. Immunohorizons 5, 735–751 (2021).
Lee, J. et al. Characterization of the fetal blood transcriptome and proteome in maternal anti-fetal rejection: evidence of a distinct and novel type of human fetal systemic inflammatory response. Am. J. Reprod. Immunol. 70, 265–284 (2013).
Olsen, I. E., Groveman, S. A., Lawson, M. L., Clark, R. H. & Zemel, B. S. New intrauterine growth curves based on United States data. Pediatrics 125, e214–e224 (2010).
Olsen, I. E. et al. BMI curves for preterm infants. Pediatrics 135, e572–e581 (2015).
Rezaie, P. & Dean, A. Periventricular leukomalacia, inflammation and white matter lesions within the developing nervous system. Neuropathology 22, 106–132 (2002).
Murphy, D. J., Sellers, S., MacKenzie, I. Z., Yudkin, P. L. & Johnson, A. M. Case-control study of antenatal and intrapartum risk factors for cerebral palsy in very preterm singleton babies. Lancet 346, 1449–1454 (1995).
Yoon, B. H. et al. Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. Am. J. Obstet. Gynecol. 177, 19–26 (1997).
Grether, J. K. & Nelson, K. B. Maternal infection and cerebral palsy in infants of normal birth weight. JAMA 278, 207–211 (1997).
Wu, Y. W. et al. Chorioamnionitis and cerebral palsy in term and near-term infants. JAMA 290, 2677–2684 (2003).
Polam, S., Koons, A., Anwar, M., Shen-Schwarz, S. & Hegyi, T. Effect of chorioamnionitis on neurodevelopmental outcome in preterm infants. Arch. Pediatr. Adolesc. Med. 159, 1032–1035 (2005).
Soraisham, A. S., Trevenen, C., Wood, S., Singhal, N. & Sauve, R. Histological chorioamnionitis and neurodevelopmental outcome in preterm infants. J. Perinatol. 33, 70–75 (2013).
Shi, Z. et al. Chorioamnionitis in the Development of Cerebral Palsy: A Meta-analysis and Systematic Review. Pediatrics 139 https://doi.org/10.1542/peds.2016-3781 (2017).
Elimian, A. et al. Histologic chorioamnionitis, antenatal steroids, and perinatal outcomes. Obstet. Gynecol. 96, 333–336 (2000).
Been, J. V., Degraeuwe, P. L., Kramer, B. W. & Zimmermann, L. J. Antenatal steroids and neonatal outcome after chorioamnionitis: a meta-analysis. BJOG 118, 113–122 (2011).
Xing, L. et al. Is chorioamnionitis associated with neurodevelopmental outcomes in preterm infants? A systematic review and meta-analysis following PRISMA. Med. (Baltim.) 98, e18229 (2019).
Maisonneuve, E., Ancel, P. Y., Foix-L’Helias, L., Marret, S. & Kayem, G. Impact of clinical and/or histological chorioamnionitis on neurodevelopmental outcomes in preterm infants: A literature review. J. Gynecol. Obstet. Hum. Reprod. 46, 307–316 (2017).
Nosaka, R. et al. Intrauterine exposure to chorioamnionitis and neuroanatomical alterations at term-equivalent age in preterm infants. Arch. Gynecol. Obstet. 309, 1909–1918 (2024).
Kim, C. J. et al. Umbilical arteritis and phlebitis mark different stages of the fetal inflammatory response. Am. J. Obstet. Gynecol. 185, 496–500 (2001).
Hecht, J. L. et al. Relationship Between Neonatal Blood Protein Concentrations and Placenta Histologic Characteristics in Extremely Low GA Newborns. Pediatr. Res. 69, 68–73 (2011).
Oh, J. W., Park, C. W., Moon, K. C., Park, J. S. & Jun, J. K. Fetal inflammatory response is positively correlated with the progress of inflammation in chorionic plate. Placenta 97, 6–17 (2020).
Tang, Q., Zhang, L., Li, H. & Shao, Y. The fetal inflammation response syndrome and adverse neonatal outcomes: a meta-analysis. J. Matern Fetal Neonatal Med 34, 3902–3914 (2021).
Burd, I., Balakrishnan, B. & Kannan, S. Models of fetal brain injury, intrauterine inflammation, and preterm birth. Am. J. Reprod. Immunol. 67, 287–294 (2012).
Kuypers, E. et al. White matter injury following fetal inflammatory response syndrome induced by chorioamnionitis and fetal sepsis: lessons from experimental ovine models. Early Hum. Dev. 88, 931–936 (2012).
Yap, V. & Perlman, J. M. Mechanisms of brain injury in newborn infants associated with the fetal inflammatory response syndrome. Semin Fetal Neonatal Med. 25, 101110 (2020).
Oh, K. J. et al. The combined exposure to intra-amniotic inflammation and neonatal respiratory distress syndrome increases the risk of intraventricular hemorrhage in preterm neonates. J. Perinat. Med. 46, 9–20 (2018).
Yanni, D. et al. Both antenatal and postnatal inflammation contribute information about the risk of brain damage in extremely preterm newborns. Pediatr. Res. 82, 691–696 (2017).
van Tilborg, E. et al. Combined fetal inflammation and postnatal hypoxia causes myelin deficits and autism-like behavior in a rat model of diffuse white matter injury. Glia 66, 78–93 (2018).
Marin-Padilla, M. Developmental neuropathology and impact of perinatal brain damage. II: white matter lesions of the neocortex. J. Neuropathol. Exp. Neurol. 56, 219–235 (1997).
Van Essen, D. C. A tension-based theory of morphogenesis and compact wiring in the central nervous system. Nature 385, 313–318 (1997).
Duan, J. et al. Histological chorioamnionitis and pathological stages on very preterm infant outcomes. Histopathology 84, 1024–1037 (2024).
Han, V. X., Patel, S., Jones, H. F. & Dale, R. C. Maternal immune activation and neuroinflammation in human neurodevelopmental disorders. Nat. Rev. Neurol. 17, 564–579 (2021).
Acknowledgements
We wish to thank several people who participated in data collection: Patti J Burchfield, RN, and Pollieanna M Sepulveda, RN. This work was supported by Children’s Clinical Research Advisory Council (CCRAC) grant awarded to Dr. Imran N. Mir.
Author information
Authors and Affiliations
Contributions
Imran N. Mir wrote the first version of the manuscript. Steven Brown performed statistical analyses. All authors participated in the study design, data collection, data interpretation, and revision and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The Institutional Review Board of University of Texas Southwestern Medical Center and Parkland Health approved the study and waived the need for individual consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mir, I.N., Machie, M., Clarke, R. et al. Impact of fetal inflammatory response on brain MRI abnormalities in extremely preterm infants. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04230-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04230-7