Abstract
Background
A history of atopy is associated with respiratory morbidities in term-born children; however, little is known about how allergies/atopy affect respiratory outcomes in children with bronchopulmonary dysplasia (BPD). This study aims to describe the prevalence of reported allergies/atopy in young children with BPD and assess whether allergies/atopy are associated with outpatient outcomes.
Methods
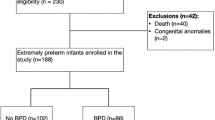
A retrospective longitudinal cohort study of children between 0 and 36 months of age followed at outpatient BPD clinics was performed using data from questionnaires administered during routine clinical encounters. The presence of allergy/atopy was defined by caregiver questionnaires. Generalized estimating equations were used to adjust associations between allergy/atopy and respiratory outcomes.
Results
Rates of reported allergy/atopy in a cohort of infants and children with BPD (21.6%) were similar to previously published rates in healthy children. Children with atopy/allergy were more likely to be born at earlier gestational ages, have pulmonary hypertension, and be non-white and non-Hispanic compared to their non-atopic peers and to experience trouble breathing, nighttime symptoms, activity limitations, and rescue medication use during the first three years of life.
Conclusions
In children with BPD, allergy/atopy was more common among those born at earlier gestational ages and was significantly associated with increased respiratory symptoms during the first 3 years of life. Further studies are needed to assess whether the association between allergy/atopy and increased respiratory morbidity persists throughout childhood and affects later lung function and whether potential interventions, including inhaled steroids, may modify this risk.
Impact
-
There is limited data on the prevalence of atopy/allergy in children with bronchopulmonary dysplasia (BPD) and the association between allergy/atopy and respiratory outcomes in this population.
-
Our findings demonstrate that in children with BPD, allergy/atopy was more common among those born at earlier gestational ages and was associated with increased respiratory symptoms and rescue medication use during the first 3 years of life.
-
Further studies are needed to determine whether this association persists throughout childhood and affects later lung function and whether potential interventions may modify this risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data supporting this study’s findings are available from the BPD Collaborative. However, restrictions apply to the availability of these data, and so they are not publicly available. Data are available from the authors upon reasonable request and with permission of the BPD Collaborative.
References
Collaco, J. M. & McGrath-Morrow, S. A. Respiratory phenotypes for preterm infants, children, and adults: bronchopulmonary dysplasia and more. Ann. Am. Thorac. Soc. 15, 530–538 (2018).
Aoyama, B. C., Rice, J. L., McGrath-Morrow, S. A. & Collaco, J. M. Mortality in outpatients with bronchopulmonary dysplasia. J. Pediatr. 241, 48–53.e1 (2022).
Baker, C. D., Abman, S. H. & Mourani, P. M. Pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Pediatr. Allergy Immunol. Pulmonol. 27, 8–16 (2014).
Bhandari, A. & Bhandari, V. Pitfalls, problems, and progress in bronchopulmonary dysplasia. Pediatrics 123, 1562–1573 (2009).
Gerner, T. et al. Differences in occurrence, risk factors and severity of early-onset atopic dermatitis among preterm and term children. Acta Derm. Venereol. 102, adv00737 (2022).
Tronnes, H. et al. Associations of maternal atopic diseases with adverse pregnancy outcomes: a national cohort study. Paediatr. Perinat. Epidemiol. 28, 489–497 (2014).
Ronkainen, E., Kaukola, T., Marttila, R., Hallman, M. & Dunder, T. School-age children enjoyed good respiratory health and fewer allergies despite having lung disease after preterm birth. Acta Paediatr. 105, 1298–1304 (2016).
Astle, V. et al. Respiratory outcomes study (RESPOS) for preterm infants at primary school age. J. Asthma 52, 40–45 (2015).
Brostrom, E. B., Thunqvist, P., Adenfelt, G., Borling, E. & Katz-Salamon, M. Obstructive lung disease in children with mild to severe BPD. Respir. Med 104, 362–370 (2010).
Vollsaeter, M. et al. Adult respiratory outcomes of extreme preterm birth. A regional cohort study. Ann. Am. Thorac. Soc. 12, 313–322 (2015).
Vom Hove, M., Prenzel, F., Uhlig, H. H. & Robel-Tillig, E. Pulmonary outcome in former preterm, very low birth weight children with bronchopulmonary dysplasia: a case-control follow-up at school age. J. Pediatr. 164, 40–5 e4 (2014).
Landry, J. S. et al. Lung function and bronchial hyperresponsiveness in adults born prematurely. A cohort study. Ann. Am. Thorac. Soc. 13, 17–24 (2016).
Guimarães, H. et al. Respiratory outcomes and atopy in school-age children who were preterm at birth, with and without bronchopulmonary dysplasia. Clin. (Sao Paulo) 66, 425–430 (2011).
Siltanen, M., Savilahti, E., Pohjavuori, M. & Kajosaari, M. Respiratory symptoms and lung function in relation to atopy in children born preterm. Pediatr. Pulmonol. 37, 43–49 (2004).
Malmberg, L. P. et al. Very low birth weight and respiratory outcome: association between airway inflammation and hyperresponsiveness. Ann. Allergy Asthma Immunol. 111, 96–101 (2013).
Smith, E. F. et al. Risk factors for poorer respiratory outcomes in adolescents and young adults born preterm. Thorax 78, 1223–1232 (2023).
Collaco, J. M. et al. Characteristics of infants or children presenting to outpatient bronchopulmonary dysplasia clinics in the United States. Pediatr. Pulmonol. 56, 1617–1625 (2021).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med 163, 1723–1729 (2001).
Collaco, J. M. et al. Validation of an outpatient questionnaire for bronchopulmonary dysplasia control. Pediatr. Pulmonol. 58, 1551–1561 (2023).
Zablotsky, B., Black, L. I., Akinbami, L. J. Diagnosed Allergic Conditions in Children Aged 0-17 Years: United States, 2021. NCHS Data Brief. 2023:1-8.
Cho, H. Y. et al. Prospective epigenome and transcriptome analyses of cord and peripheral blood from preterm infants at risk of bronchopulmonary dysplasia. Sci. Rep. 13, 12262 (2023).
Wang, L., Xiao, J., Zhang, B. & Hou, A. Epigenetic modifications in the development of bronchopulmonary dysplasia: A review. Pediatr. Res. 96, 632–642 (2024).
Wolska, M., Wypych, T. P. & Rodríguez-Viso, P. The influence of premature birth on the development of pulmonary diseases: Focus on the microbiome. Metabolites 14, 382 (2024).
Thomsen, S. F. Epidemiology and natural history of atopic diseases. Eur. Clin. Respir. J. 2, 24642 (2015).
He, H. et al. Preterm birth with childhood asthma: The role of degree of prematurity and asthma definitions. Am. J. Respir. Crit. Care Med 192, 520–523 (2015).
Qazi, K. R. et al. Extremely preterm infants have significant alterations in their conventional T cell compartment during the first weeks of life. J. Immunol. 204, 68–77 (2020).
Darrasse-Jèze, G., Marodon, G., Salomon, B. L., Catala, M. & Klatzmann, D. Ontogeny of CD4+CD25+ regulatory/suppressor T cells in human fetuses. Blood 105, 4715–4721 (2005).
Dirix, V., Vermeulen, F. & Mascart, F. Maturation of CD4+ regulatory T lymphocytes and of cytokine secretions in infants born prematurely. J. Clin. Immunol. 33, 1126–1133 (2013).
Szekeres-Bartho, J. Immunological relationship between the mother and the fetus. Int Rev. Immunol. 21, 471–495 (2002).
Moore, M. M. et al. Perinatal predictors of atopic dermatitis occurring in the first six months of life. Pediatrics 113, 468–474 (2004).
Johnson, A., Mason, T., Kirby, R. S., Ledford, D. & Salihu, H. M. Examining the association between maternal atopy and birth outcomes using a retrospective cohort in the southeastern region of the USA. BMJ Open 7, e017161 (2017).
Pagano, F. et al. Atopic manifestations in children born preterm: A long-term observational study. Children (Basel) 8, 843 (2021).
Gdalevich, M., Mimouni, D., David, M. & Mimouni, M. Breast-feeding and the onset of atopic dermatitis in childhood: A systematic review and meta-analysis of prospective studies. J. Am. Acad. Dermatol 45, 520–527 (2001).
Chiang, K. V., Sharma, A. J., Nelson, J. M., Olson, C. K. & Perrine, C. G. Receipt of breast milk by gestational age - United States, 2017. MMWR Morb. Mortal. Wkly Rep. 68(Jun), 489–493 (2019).
Acknowledgements
No financial assistance was received in support of this study.
Author information
Authors and Affiliations
Contributions
Contribution to conception and design, analysis, and interpretation of data: B.C. A., S.A.M.-M., J.M.C.; Acquisition of data: G.G.A., A.A., B.C.A., E.D.A., M.B., A.B., J.M.C., A. I.C., S.K.D., J.C.L., S.A.M.-M., P.E.M., C.A.S.; Drafting the manuscript: B.C.A., S.A.M.-M., J.M.C.; Revising the manuscript critically for intellectual content and final approval for version to be published: S.H.A., A.A., B.C.A., G.G.A., E.D.A., C.D.B., M.B., A.B., J.M. C., A. I.C., S.K.D., M.H.A., J.K.H., J.M.L., J.C.L., SA.M.-M., P.E.M., L.M.R., C.A.S., R.S., N. S., D.T..
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patient consent was required and obtained per local institutional IRBs.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aoyama, B.C., Collaco, J.M., Agarwal, A. et al. Allergy and atopic phenotype are associated with earlier gestation and severity of respiratory symptoms in bronchopulmonary dysplasia. Pediatr Res 99, 209–214 (2026). https://doi.org/10.1038/s41390-025-04277-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-04277-6
This article is cited by
-
Preterm birth, bronchopulmonary dysplasia and the risk of allergic diseases
Pediatric Research (2025)