Abstract
Background
The role of emergency medical services (EMS) in out-of-hospital cardiac arrest (OHCA) among children and young adults remains understudied. This study evaluated EMS utilization and its association with outcomes in non-traumatic pediatric and young adult OHCA.
Methods
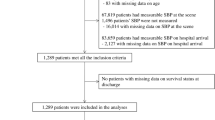
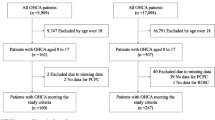
Patients aged <35 years with non-traumatic OHCA treated at a tertiary center between 1995 and 2019 were analyzed. Exclusion criteria included referrals and newborns <24 hours old. EMS use was defined as public-ambulance transport to the emergency department. The primary outcome was return of spontaneous circulation (ROSC).
Results
Of 195 OHCAs, 109 (55.9%) were pediatric. EMS use increased with age, from 38.0% (0–5 years) to 82.6% (18 to <35 years). EMS was associated with higher ROSC and survival to hospital discharge (41.7% vs. 24.6%, p = 0.06, and 25.0% vs. 6.6%, p = 0.007, respectively) in pediatric group but not in the young adult group. However, EMS improved the ROSC rate in young adults from 30.8% during 1995–2002 to 65.7% during 2011–2019. The impact of EMS was not significant after multivariable adjustment.
Conclusion
EMS utilization and clinical outcomes in pediatric and young adults OHCA remained suboptimal over the 25-year study period. Targeted advocacy and education are essential to strengthen the chain of survival in these population.
Impact
-
Pediatric OHCA patients had significantly lower EMS use than young adults. EMS was associated with higher ROSC and survival to hospital discharge in the pediatric group but not in the young adult group.
-
While EMS-transported young adults showed improved outcomes over time, pediatric outcomes remained unchanged.
-
Pediatric OHCA patients transported by EMS had shorter scene times and received fewer prehospital interventions than young adults.
-
Educating caregivers on the importance of EMS activation is crucial. Emergency departments must be prepared for unannounced pediatric cases. There is an urgent need for protocols specifically tailored to pediatric OHCA care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, Wei-Chieh Tseng, upon reasonable request.
References
Engdahl, J., Axelsson, A., Bång, A., Karlson, B. W. & Herlitz, J. The epidemiology of cardiac arrest in children and young adults. Resuscitation 58, 131–138 (2003).
Atkins, D. L. et al. Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation 119, 1484–1491 (2009).
Nehme, Z. et al. Trends in the incidence and outcome of paediatric out-of-hospital cardiac arrest: A 17-year observational study. Resuscitation 128, 43–50 (2018).
Tseng, W. C. et al. Cumulative postnatal risk of pediatric sudden death and all-cause mortality in nationwide birth cohorts of Taiwan and the United States. J. Formos. Med Assoc. 119, 1842–1853 (2020).
Okubo, M., Chan, H. K., Callaway, C. W., Mann, N. C. & Wang, H. E. Characteristics of paediatric out-of-hospital cardiac arrest in the United States. Resuscitation 153, 227–233 (2020).
Chia, M. Y. et al. PAROS Clinical Research Network. Characteristics and outcomes of young adults who suffered an out-of-hospital cardiac arrest (OHCA). Resuscitation 111, 34–40 (2017).
Fovaeus, H. et al. Out-of-hospital cardiac arrest: Survival in children and young adults over 30 years, a nationwide registry-based cohort study. Resuscitation 195, 110103 (2024).
Tham, L. P. et al. Pan-Asian Resuscitation Outcomes Study Clinical Research Network. Pre-hospital airway management and survival outcomes after paediatric out-of-hospital cardiac arrests. Resuscitation 176, 9–18 (2022).
Kitamura, T. et al. Japanese Circulation Society Resuscitation Science Study Group. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation 126, 2834–2843 (2012).
Young, K. D., Gausche-Hill, M., McClung, C. D. & Lewis, R. J. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics 114, 157–164 (2004).
Deasy, C. et al. Epidemiology of paediatric out-of-hospital cardiac arrest in Melbourne, Australia. Resuscitation 81, 1095–1100 (2010).
Liu, H. M. et al. The postnatal risk, resuscitation success rate and outcomes of pediatric sudden death in Taiwan. Acta Cardiol. Sin. 37, 296–304 (2021).
Tham, L. P. et al. Epidemiology and outcome of paediatric out-of-hospital cardiac arrests: A paediatric sub-study of the Pan-Asian resuscitation outcomes study (PAROS). Resuscitation 125, 111–117 (2018).
Topjian, A. A. et al. Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142, S469–S523 (2020).
Allan, K. S., Morrison, L. J., Pinter, A., Tu, J. V. & Dorian, P. Rescu Epistry Investigators. “Presumed cardiac” arrest in children and young adults: A misnomer?. Resuscitation 117, 73–79 (2017).
Bagnall, R. D. et al. A prospective study of sudden cardiac death among children and young adults. N. Engl. J. Med 23 374, 2441–2452 (2016).
Ackerman, M., Atkins, D. L. & Triedman, J. K. Sudden cardiac death in the young. Circulation 133, 1006–1026 (2016).
Lin, H. Y. et al. Taipei City Fire Department Quality Assurance Team. Outcomes of out-of-hospital cardiac arrests after a decade of system-wide initiatives optimising community chain of survival in Taipei city. Resuscitation 172, 149–158 (2022).
Chua, I. S. Y. et al. Singapore PAROS investigators. The association between mode of transport and out-of-hospital cardiac arrest outcomes in Singapore. Resuscitation 173, 136–143 (2022).
Chiang, W. C. et al. EMS in Taiwan: past, present, and future. Resuscitation 80, 9–13 (2009).
Huan, T. L. et al. Emergency medical services in Taiwan: past, present, and future. J. Acute Med 13, 91–103 (2023).
Bray, J. E. et al. International Liaison Committee on Resuscitation. Cardiac arrest and cardiopulmonary resuscitation outcome reports: 2024 Update of the Utstein Out-of-Hospital Cardiac Arrest Registry Template. Circulation 150, e203–e223 (2024).
Phelps, R., Dumas, F., Maynard, C., Silver, J. & Rea, T. Cerebral performance category and long-term prognosis following out-of-hospital cardiac arrest. Crit. Care Med 41, 1252–1257 (2013).
Pollack, M. M. et al. Relationship between the functional status scale and the pediatric overall performance category and pediatric cerebral performance category scales. JAMA Pediatr. 168, 671–676 (2014).
Fukuda, T. et al. Public access defibrillation and outcomes after pediatric out-of-hospital cardiac arrest. Resuscitation 111, 1–7 (2017).
Lee, J. et al. Clinical survey and predictors of outcomes of pediatric out-of-hospital cardiac arrest admitted to the emergency department. Sci. Rep. 9, 7032 (2019).
Berg, K. M. et al. Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, and Resuscitation Education Science Writing Groups. Part 7: Systems of Care: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142, S580–S604 (2020).
Brady, W. J., Mattu, A. & Slovis, C. M. Lay responder care for an adult with out-of-hospital cardiac arrest. N. Engl. J. Med 381, 2242–2251 (2019).
Li, C. J. et al. Factors associated with sustained return of spontaneous circulation in children after out-of-hospital cardiac arrest of noncardiac origin. Am. J. Emerg. Med 28, 310–317 (2010).
Bahr, N., Meckler, G., Hansen, M. & Guise, J. M. Evaluating pediatric advanced life support in emergency medical services with a performance and safety scoring tool. Am. J. Emerg. Med 48, 301–306 (2021).
Fukuda, T. et al. Type of advanced airway and survival after pediatric out-of-hospital cardiac arrest. Resuscitation 150, 145–153 (2020).
Hansen, M., Eriksson, C., Skarica, B., Meckler, G. & Guise, J. M. Safety events in pediatric out-of-hospital cardiac arrest. Am. J. Emerg. Med 36, 380–383 (2018).
Acknowledgements
The authors thank the staff of the National Taiwan University Hospital Statistical Consulting Unit for their assistance with the statistical analysis. This study was supported by grants from Taiwan Ministry of Science and Technology [106-2314-B-002-204, 107-2314-B-002-007, 108-2314-B-002-005, 112-2314-B-002-177]. The funding sources had no role in the design, conduct, or reporting of the study.
Author information
Authors and Affiliations
Contributions
Szu-Han Chen - Contributing to data curation, formal analysis, visualization, and writing - original draft. Meng-Chang Lee - Contributing to data curation, formal analysis, and writing - review & editing. Po-Yuan Wang, Yen-Ju Chu, Hsin-Ming Liu, Jhong-Lin Wu, Ming-Ju Hsieh, Matthew Huei-Ming Ma - Contributing to the data curation, supervision, and writing - review & editing. Wen-Chu Chiang - Contributing to the data curation, methodology, supervision, validation, and writing - review & editing. Wei-Chieh Tseng - Contributing to conceptualization, data curation, formal analysis, funding acquisition, methodology, project administration, resources, supervision, writing – review & editing. All authors have given their final approval of the version to be published and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Consent to participate
The requirement for patient and parental consent was waived due to the anonymous and retrospective nature of the data.
Ethics approval
This study was approved by the Institutional Research Ethics Review Board of National Taiwan University Hospital (NTUH-202208063RINA).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, SH., Lee, MC., Wang, PY. et al. Impact of emergency medical services transport on non-traumatic out-of-hospital cardiac arrest in pediatric and young adult: 25-year single-center experience. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04295-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04295-4