Abstract
Background
Perinatal intimate partner violence (IPV) poses significant health risks for victims and their children. While maternal IPV victimization has been extensively studied, research on paternal IPV victimization remains limited. This study examines the prevalence of paternal perinatal IPV victimization and its association with child abuse and paternal psychological distress.
Methods
We analyzed cross-sectional data from 1248 postnatal fathers whose partners had given birth within 1 year in August 2021. IPV victimization was assessed across physical, psychological, economic, and sexual abuse subtypes. Outcomes included child abuse (physical, psychological, neglect, or any abuse) and paternal psychological distress. Modified Poisson regression was used to compute risk ratios (RR).
Results
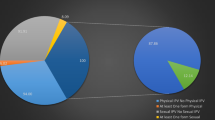
Among fathers surveyed, 13.6% reported IPV victimization. Paternal IPV was associated with increased risk of child abuse, including physical (RR 2.04; 95% CI, 1.33–3.14), psychological (RR 2.08; 95% CI, 1.52–2.84), neglect (RR 3.10; 95% CI, 1.70–5.66), and any abuse (RR 1.98; 95% CI, 1.50–2.61).
Conclusions
Paternal perinatal IPV victimization is a significant public health concern associated with an increased risk of child abuse and psychological distress. These findings highlight the importance of considering fathers in IPV-related research and suggest the need for further study on inclusive approaches to family violence prevention.
Impact
-
Perinatal IPV victimization leads to adverse health outcomes for both victims and their children.
-
Our study found that 14% of postnatal fathers experienced perinatal IPV victimization, highlighting its prevalence.
-
Paternal perinatal IPV victimization is associated with an increased risk of child abuse within the household.
-
Additionally, paternal IPV victimization is linked to higher levels of paternal psychological distress.
-
These findings highlight the need for targeted support for affected fathers to protect child well-being.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, E.O., upon reasonable request.
References
Alhusen, J. L., Ray, E., Sharps, P. & Bullock, L. Intimate partner violence during pregnancy: maternal and neonatal outcomes. J. Women’s Health 24, 100–106 (2015).
Paulson, J. L. Intimate partner violence and perinatal post-traumatic stress and depression symptoms: a systematic review of findings in longitudinal studies. Trauma Violence Abus. 23, 733–747 (2022).
Palladino, C. L., Singh, V., Campbell, J., Flynn, H. & Gold, K. J. Homicide and suicide during the perinatal period: findings from the national violent death reporting system. Obstet. Gynecol. 118, 1056–1063 (2011).
Chiesa, A. E. et al. Intimate partner violence victimization and parenting: a systematic review. Child Abuse Negl. 80, 285–300 (2018).
Kelleher, K. J. et al. Self-reported disciplinary practices among women in the child welfare system: association with domestic violence victimization. Child Abuse Negl. 32, 811–818 (2008).
Lannert, B. K. et al. Relational trauma in the context of intimate partner violence. Child Abuse Negl. 38, 1966–1975 (2014).
Taylor, C. A., Guterman, N. B., Lee, S. J. & Rathouz, P. J. Intimate partner violence, maternal stress, nativity, and risk for maternal maltreatment of young children. Am. J. Public Health 99, 175–183 (2009).
Casanueva, C. E. & Martin, S. L. Intimate partner violence during pregnancy and mothers’ child abuse potential. J. Interpers. Violence 22, 603–622 (2007).
Chang, J. J., Theodore, A. D., Martin, S. L. & Runyan, D. K. Psychological abuse between parents: associations with child maltreatment from a population-based sample. Child Abus. Negl. 32, 819–829 (2008).
Coohey, C. Battered mothers who physically abuse their children. J. Interpers. Violence 19, 943–952 (2004).
Gustafsson, H. C. et al. Family violence and children’s behavior problems: independent contributions of intimate partner and child-directed physical aggression. J. Fam. Violence 29, 773–781 (2014).
Pence, E., & Paymar, M. Creating a Process of Change for Men Who Batter: An Education Curriculum. Duluth, MN: Domestic Abuse Intervention Project (2003).
Schwartz, M. D. & DeKeseredy, W. S. Interpersonal violence against women: the role of men. J. Contemp. Crim. Justice 24, 178–185 (2008).
Archer, J. Sex differences in aggression between heterosexual partners: a meta-analytic review. Psychol. Bull. 126, 651–680 (2000).
Breiding, M. J. et al. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization-national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill. Summ. 63, 1–18 (2014).
Capaldi, D. M., Kim, H. K. & Shortt, J. W. Observed initiation and reciprocity of physical aggression in young, at-risk couples. J. Fam. Violence 22, 101–111 (2007).
Dutton, D. G., Nicholls, T. L. & Spidel, A. in Women Who Perpetrate Relationship Violence 1–31 (Routledge, 2014).
Straus, M. A. Dominance and symmetry in partner violence by male and female university students in 32 nations. Child. Youth Serv. Rev. 30, 252–275 (2008).
Leemis, R. W. et al. The National Intimate Partner and Sexual Violence Survey: 2016/2017 Report on Intimate Partner Violence. (2022).
Lysova, A. & Dim, E. E. Severity of victimization and formal help seeking among men who experienced intimate partner violence in their ongoing relationships. J. Interpers. Violence 37, 1404–1429 (2022).
Taylor, J. C., Bates, E. A., Colosi, A. & Creer, A. J. Barriers to men’s help seeking for intimate partner violence. J. Interpers. Violence 37, Np18417–np18444 (2022).
Terada, S., Fujiwara, T., Obikane, E. & Tabuchi, T. Association of paternity leave with impaired father-infant bonding: findings from a nationwide online survey in Japan. Int. J. Environ. Res. Public Health 19, 4251 (2022).
Isumi, A., Fujiwara, T., Nawa, N., Ochi, M. & Kato, T. Mediating effects of parental psychological distress and individual-level social capital on the association between child poverty and maltreatment in Japan. Child Abus. Negl. 83, 142–150 (2018).
Furukawa, T. A. et al. The performance of the japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 17, 152–158 (2008).
Sakurai, K., Nishi, A., Kondo, K., Yanagida, K. & Kawakami, N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin. Neurosci. 65, 434–441 (2011).
Kessler, R. C. et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med 32, 959–976 (2002).
Fujiwara, T. Impact of adverse childhood experience on physical and mental health: a life-course epidemiology perspective. Psychiatry Clin. Neurosci. 76, 544–551 (2022).
Krishnakumar, A. & Buehler, C. Interparental conflict and parenting behaviors: a meta-analytic review. Fam. Relat. 49, 25–44 (2000).
Erel, O. & Burman, B. Interrelatedness of marital relations and parent-child relations: a meta-analytic review. Psychol. Bull. 118, 108–132 (1995).
Lannert, B. K., Levendosky, A. A. & Bogat, G. A. The interaction of maternal personality traits and intimate partner violence as influences on maternal representations. Infant Ment. Health J. 34, 222–233 (2013).
Obikane, E., Nishi, D., Morisaki, N. & Tabuchi, T. Risk factors of paternal perinatal depression during the Covid-19 pandemic in Japan. J. Psychosom. Obstet. Gynaecol. 44, 2245556 (2023).
Kiely, M., El-Mohandes, A. A. E., El-Khorazaty, M. N. & Gantz, M. G. An integrated intervention to reduce intimate partner violence in pregnancy: a randomized controlled trial. Obstet. Gynecol. 115, 273–283 (2010).
Bair-Merritt, M., Zuckerman, B., Augustyn, M. & Cronholm, P. F. Silent victims-an epidemic of childhood exposure to domestic violence. N. Engl. J. Med. 369, 1673–1675 (2013).
Sharps, P. W. et al. Domestic violence enhanced perinatal home visits: the Dove randomized clinical trial. J. Women’s Health 25, 1129–1138 (2016).
Acknowledgements
We thank all the participants for their time and engagement in the JACSIS study.
Funding
The work is funded by Ready for COVID-19 Relief Fund [grant number: 5th period 2nd term 001]; the Japan Society for the Promotion of Science (JSPS) KAKENHIKAKENHI Grants, [grant number: 21H04856; 23K16345; 21K21131]; the Health and Labour Sciences Research Grants [grant number: 23DA0701].
Author information
Authors and Affiliations
Contributions
E.O. conceptualized and designed the study, conducted the statistical analysis, and drafted the initial manuscript. D.N. and T.T. conceptualized and designed the study. All authors critically reviewed and revised the manuscript, approved the final manuscript as submitted, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
D.N. reports personal fees outside of the submitted work from Startia, Inc., MD.net, and Takeda Pharmaceutical Company, Ltd. Other authors have no conflicts of interest relevant to this article to disclose.
Ethics approval
This study is approved by the Osaka International Cancer Institute’s Research Ethics Committee (approval number: 20084) and the Research Ethics Committee of the Graduate School of Medicine/Faculty of Medicine, The University of Tokyo (approval number: 2020336NI).
Patient consent
Informed consent was obtained electronically from all participants included in this study. Participants were provided with detailed information regarding the study’s purpose, procedures, potential risks, and confidentiality measures before giving their consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obikane, E., Nishi, D., Kato, T. et al. Paternal perinatal intimate partner violence victimization and child abuse. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04296-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04296-3