Abstract
Background
Intradialytic hypotension (IDH) leads to inadequate organ perfusion and occurs frequently after continuous renal replacement therapy (CRRT) connection. Unsupervised learning can enhance our understanding of how clinical trajectories impact outcomes. We aim to investigate the association between IDH during CRRT connection and outcomes, while also identifying hemodynamic trajectory-based phenotypes.
Methods
A single center retrospective observational study of children (<18 years) undergoing CRRT from 9/2016 to 10/2018. IDH was defined as a sustained >20% decrease in mean arterial pressure (MAP) from baseline for ≥2 consecutive minutes. IDH burden was calculated by dividing connections with IDH by total observed connections. The primary outcome was major adverse kidney events at 30 days (MAKE30). K-means clustering was used to identify MAP trajectory-based phenotypes.
Results
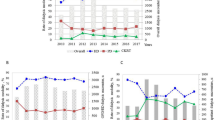
59 patients, 232 connections, and 13,920 minutes were included. Median age was 59 months (IQR 8-152). In multivariable analysis, higher IDH burden [β 4.35 (CI: 0.01–8.70)] was associated with MAKE30. Two distinct MAP trajectories phenotypes were identified, with differing incidence of MAKE30 [21 (100%) vs. 29 (76%), p < 0.01].
Conclusions
IDH within the first hour of CRRT connection is associated with poor outcomes, and time-series clustering is feasible and could improve our understanding of the impact of CRRT in children.
Impact
-
Repeated episodes of intradialytic hypotension within the first hour of continuous renal replacement therapy connection are associated with increased morbidity and mortality.
-
Our findings suggest that intradialytic hypotension in the hour following CRRT connection in children is associated with poor outcomes.
-
Unsupervised machine learning, an underutilized approach in pediatric research, identified two significantly different mean arterial pressure trajectory-based phenotypes with differing anthropometric features and outcomes.
-
Leveraging unsupervised machine learning, we can identify trajectory-based subgroups that can provide insights into the impact of continuous renal replacement therapy in critically ill children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Due to the small size of the cohort, the data are not publicly available as individual participants could be easily identifiable, posing a risk to patient privacy.
References
Kaddourah, A., Basu, R. K., Bagshaw, S. M. & Goldstein, S. L. & AWARE Investigators. Epidemiology of Acute Kidney Injury in Critically Ill Children and Young Adults. N. Engl. J. Med. 376, 11–20 (2017).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–194 (2017).
Chanchlani, R. et al. Secular trends in incidence, modality and mortality with dialysis receiving AKI in children in Ontario: A Population-Based Cohort Study. Clin. J. Am. Soc. Nephrol. 14, 1288–1296 (2019).
Robinson, C. et al. Long-term kidney outcomes following childhood acute kidney injury receiving dialysis: a population-based cohort study. JASN Asn. 2020111665 https://doi.org/10.1681/ASN.2020111665 (2021).
Elbahlawan, L. & Morrison, R. R. Continuous renal replacement therapy in children post-hematopoietic stem cell transplantation: the present and the future. Curr. Stem Cell Res Ther. 7, 381–387 (2012).
Starr, M. C. et al. Continuous Kidney Replacement Therapy and Survival in Children and Young Adults: Findings From the Multinational WE-ROCK Collaborative. Am. J. Kidney Dis. S0272-6386(24)00610–3 (2024) https://doi.org/10.1053/j.ajkd.2023.12.017.
Fuhrman, D. Y. et al. Major adverse kidney events in pediatric continuous kidney replacement therapy. JAMA Netw. Open 7, e240243 (2024).
Thadani, S. et al. Patterns of multiple organ dysfunction and renal recovery in critically ill children and young adults receiving continuous renal replacement therapy. Crit. Care Explor 6, e1084 (2024).
Sutherland, S. M. et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am. J. Kidney Dis. 55, 316–325 (2010).
Gist, K. M. et al. Time to continuous renal replacement therapy initiation and 90-day major adverse kidney events in children and young adults. JAMA Netw. Open 7, e2349871 (2024).
Santiago, M. J. et al. Complications of continuous renal replacement therapy in critically ill children: a prospective observational evaluation study. Crit. Care 13, R184 (2009).
Meng, L. Heterogeneous impact of hypotension on organ perfusion and outcomes: a narrative review. Br. J. Anaesth. 127, 845–861 (2021).
Flythe, J. E., Xue, H., Lynch, K. E., Curhan, G. C. & Brunelli, S. M. Association of Mortality Risk with Various Definitions of Intradialytic Hypotension. J. Am. Soc. Nephrol. 26, 724–734 (2015).
Shawwa, K. et al. Hypotension within one-hour from starting CRRT is associated with in-hospital mortality. J. Crit. Care 54, 7–13 (2019).
Uchino, S. et al. Continuous renal replacement therapy: A worldwide practice survey: The Beginning and Ending Supportive Therapy for the Kidney (B.E.S.T. Kidney) Investigators. Intensive Care Med. 33, 1563–1570 (2007).
Akhoundi, A. et al. Incidence of adverse events during continuous renal replacement therapy. Blood Purif. 39, 333–339 (2015).
Raina, R. et al. Pediatric intradialytic hypotension: recommendations from the Pediatric Continuous Renal Replacement Therapy (PCRRT) Workgroup. Pediatr. Nephrol. 34, 925–941 (2019).
Thadani, S. et al. Hemodynamic instability during connection to continuous kidney replacement therapy in critically ill pediatric patients. Pediatr. Nephrol. 37, 2167–2177 (2022).
Fernandez Lafever, S. N. et al. Hemodynamic effects of connection to continuous renal replacement therapy in a pediatric animal model. Artif. Organs 42, 640–646 (2018).
Alzubi, J., Nayyar, A. & Kumar, A. Machine learning from theory to algorithms: an overview. J. Phys.: Conf. Ser. 1142, 012012 (2018).
Eckhardt, C. M. et al. Unsupervised machine learning methods and emerging applications in healthcare. Knee Surg. Sports Traumatol. Arthrosc. 31, 376–381 (2023).
Jiang, T., Gradus, J. L. & Rosellini, A. J. Supervised machine learning: a brief primer. Behav. Ther. 51, 675–687 (2020).
Thadani, S. et al. Machine learning-based prediction model for ICU mortality after continuous renal replacement therapy initiation in children. Crit. Care Explor.6, e1188 (2024).
Dowrick, J. M. et al. Unsupervised machine learning highlights the challenges of subtyping disorders of gut-brain interaction. Neurogastroenterol. Motil e14898 (2024) https://doi.org/10.1111/nmo.14898.
Aghabozorgi, S., Seyed Shirkhorshidi, A. & Ying Wah, T. Time-series clustering – A decade review. Inf. Syst. 53, 16–38 (2015).
McIntosh, A. M., Tong, S., Deakyne, S. J., Davidson, J. A. & Scott, H. F. Validation of the vasoactive-inotropic score in pediatric sepsis*. Pediatr. Crit. Care Med. 18, 750–757 (2017).
Gaies, M. G. et al. Vasoactive–inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass*. Pediatr. Crit. Care Med. 11, 234–238 (2010).
Leteurtre, S. et al. Daily estimation of the severity of organ dysfunctions in critically ill children by using the PELOD-2 score. Crit. Care 19, 324 (2015).
Leteurtre, S. et al. PELOD-2: an update of the PEdiatric logistic organ dysfunction score. Crit. Care Med. 41, 1761–1773 (2013).
Schwartz, G. J., Haycock, G. B., Edelmann, C. M. & Spitzer, A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58, 259–263 (1976).
Billings, F. T. IV & Shaw, A. D. Clinical trial endpoints in acute kidney injury. Nephron Clin. Pr. 127, 89–93 (2014).
Carrell, D. S. et al. A general framework for developing computable clinical phenotype algorithms. J. Am. Med. Inform. Assoc. 31, 1785–1796 (2024).
Desai, R. J. et al. Process guide for inferential studies using healthcare data from routine clinical practice to evaluate causal effects of drugs (PRINCIPLED): considerations from the FDA Sentinel Innovation Center. BMJ e076460 (2024) https://doi.org/10.1136/bmj-2023-076460.
Lee, J. Y. & Styczynski, M. P. N. S. - kNN: a modified k-nearest neighbors approach for imputing metabolomics data. Metabolomics 14, 153 (2018).
Lee, J. H. & Huber, J. C. Evaluation of multiple imputation with large proportions of missing data: how much is too much?. Iran. J. Public Health 50, 1372–1380 (2021).
Roberts, J. S., Yanay, O. & Barry, D. Age-based percentiles of measured mean arterial pressure in pediatric patients in a hospital setting. Pediatr. Crit. Care Med. 21, e759–e768 (2020).
Haque, I. U. & Zaritsky, A. L. Analysis of the evidence for the lower limit of systolic and mean arterial pressure in children. Pediatr. Crit. Care Med. 8, 138–144 (2007).
Subasi, A. Clustering examples. In Practical Machine Learning for Data Analysis Using Python 465–511 (Elsevier, 2020). https://doi.org/10.1016/B978-0-12-821379-7.00007-2.
Niennattrakul, V. & Ratanamahatana, C. A. Clustering multimedia data using time series. In 2006 International Conference on Hybrid Information Technology 372–379 (IEEE, Cheju Island, 2006). https://doi.org/10.1109/ICHIT.2006.253514.
Steinley, D., Brusco, M. J. & Hubert, L. The variance of the adjusted Rand index. Psychol. Methods 21, 261–272 (2016).
Kanbay, M. et al. An update review of intradialytic hypotension: concept, risk factors, clinical implications and management. Clin. Kidney J. 13, 981–993 (2020).
Sars, B., van der Sande, F. M. & Kooman, J. P. Intradialytic hypotension: mechanisms and outcome. Blood Purif. 49, 158–167 (2020).
Selby, N. M. & McIntyre, C. W. The acute cardiac effects of dialysis. Semin Dial. 20, 220–228 (2007).
Gubb, S. et al. Acute kidney injury in children based on electronic alerts. J. Pediatr.220, 14–20.e4 (2020).
Kong, X. et al. Acute renal injury after aortic arch reconstruction with cardiopulmonary bypass for children: prediction models by machine learning of a retrospective cohort study. Eur. J. Med. Res. 28, 499 (2023).
Dong, J. et al. Machine learning model for early prediction of acute kidney injury (AKI) in pediatric critical care. Crit. Care 25, 288 (2021).
Fragasso, T. et al. Predicting acute kidney injury with an artificial intelligence-driven model in a pediatric cardiac intensive care unit. J. Anesth. Analg. Crit. Care 3, 37 (2023).
Cama-Olivares, A. et al. Systematic review and meta-analysis of machine learning models for acute kidney injury risk classification. J. Am. Soc. Nephrol. (2025) https://doi.org/10.1681/ASN.0000000702.
Zhu, S. et al. Machine learning-aided decision-making model for the discontinuation of continuous renal replacement therapy. Blood Purif. 53, 704–715 (2024).
Kang, M. W. et al. Machine learning model to predict hypotension after starting continuous renal replacement therapy. Sci. Rep. 11, 17169 (2021).
Hung, P.-S. et al. Explainable machine learning-based risk prediction model for in-hospital mortality after continuous renal replacement therapy initiation. Diagnostics 12, 1496 (2022).
Kang, M. W. et al. Machine learning algorithm to predict mortality in patients undergoing continuous renal replacement therapy. Crit. Care 24, 42 (2020).
Dahiya, A., Pannu, N. & Soranno, D. E. Sex as a biological variable in acute kidney injury. Curr. Opin. Crit. Care 29, 529–533 (2023).
Peikari, M., Salama, S., Nofech-Mozes, S. & Martel, A. L. A cluster-then-label semi-supervised learning approach for pathology image classification. Sci. Rep. 8, 7193 (2018).
Liu, L. J., Takeuchi, T., Chen, J. & Neyra, J. A. Artificial Intelligence in Continuous Kidney Replacement Therapy. Clin. J. Am. Soc. Nephrol. 18, 671–674 (2023).
Murugan, R. et al. Association of net ultrafiltration rate with mortality among critically ill adults with acute kidney injury receiving continuous venovenous hemodiafiltration: a secondary analysis of the Randomized Evaluation of Normal vs Augmented Level (RENAL) of renal replacement therapy trial. JAMA Netw. Open 2, e195418 (2019).
Funding
No extramural financial assistance was provided for this study.
Author information
Authors and Affiliations
Contributions
S.T., C.S., P.S., T.F., A.A.A., J.C., J.A.N.: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. S.T., C.S., C.H., P.S., A.A.A., J.C., J.A.N.: Drafting the article or revising it critically for important intellectual content. S.T., C.S., C.H., K.D., P.S., T.F., A.A.A., J.C., J.A.N.: Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Given the retrospective nature of the study, the Institutional Review Board approved the protocol and waived the requirement for informed patient consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thadani, S., Silos, C., Horvat, C. et al. Intradialytic hypotension and hemodynamic phenotypes in children following continuous renal replacement therapy initiation. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04368-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04368-4