Abstract
Background
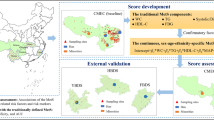
This study developed and validated a continuous metabolic syndrome (MetS) risk score (msRS) for adolescents and evaluated its clinical utility in identifying multiple clinical cardiovascular markers (CCMs) using dual adolescent populations.
Methods
Adolescents aged 12‒18 from two stratified random samples were used: the nationwide Nutrition and Health Survey in Taiwan (NAHSIT, n = 1920) for development and the Adiposity‒Cardiovascular Disease Axis study in Southern Taiwan (adiCards, n = 3295) for validation. Four sex-and-age-specific msRS were developed through confirmatory factor analysis (CFA) utilizing five MetS components—waist circumference, high-density lipoprotein cholesterol, triglycerides, fasting glucose, and mean arterial pressure. Their discriminatory ability for clinical outcomes was validated using the area under receiver operating characteristic (AU-ROC) curve.
Results
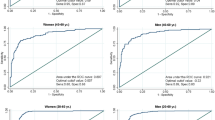
The msRS demonstrated exceptional capability in detecting MetS in NAHSIT and adiCards cohorts (AU-ROCs: 0.954‒0.969). Adjusted for covariates, msRS explained higher variability in body-fat percentage, apolipoproteins B/A1, and homeostatic model assessment of insulin resistance (HOMA-IR) than binary MetS and abnormal components count (partial R2, 23.7‒26.8% vs 4.1‒20.7%) in the validation dataset. An increase in msRS was associated with a 1.9-, 2.7-, 3.4-, and 14.4-fold risk of elevated low-density lipoprotein cholesterol, hyperuricemia, high HOMA-IR, and ≥3 CCMs.
Conclusion
The CFA-derived sex-and-age-adjusted msRS scheme provides an improving measure to assess and manage adolescent cardiometabolic health.
Impact
-
Adolescent MetS components share a latent metabolic construct.
-
A scoring system through confirmatory factor analysis captures sex-and-age specific metabolic heterogeneity.
-
Continuous risk score accurately discriminates pediatric MetS.
-
MetS risk score effectively detects pediatric cardiovascular risk.
-
Consideration of population characteristics is essential when developing a continuous MetS score.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The findings of this study are based on data analyzed under institutional confidentiality agreements and are not available for public access. All data are anonymized to ensure participant privacy. For specific data inquiries, please contact the corresponding author, Chien-Hung Lee.
References
Jacobs, D. R. Jr. et al. Childhood cardiovascular risk factors and adult cardiovascular events. N. Engl. J. Med. 386, 1877–1888 (2022).
Shulman, G. I. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N. Engl. J. Med. 371, 1131–1141 (2014).
Morrison, J. A., Friedman, L. A. & Gray-McGuire, C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the princeton lipid research clinics follow-up study. Pediatrics 120, 340–345 (2007).
Morrison, J. A., Friedman, L. A., Wang, P. & Glueck, C. J. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J. Pediatrics 152, 201–206 (2008).
Noubiap, J. J. et al. Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc. Health 6, 158–170 (2022).
Goodman, E., Daniels, S. R., Meigs, J. B. & Dolan, L. M. J. C. Instability in the diagnosis of metabolic syndrome in adolescents. Circulation 115, 2316–2322 (2007).
Wu, P. W. et al. Stability and transformation of metabolic syndrome in adolescents: a prospective assessment in relation to the change of cardiometabolic risk factors. Nutrients 14, 744 (2022).
Zimmet, P. et al. The Metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr. Diab. 8, 299–306 (2007).
Chin, Y. T. et al. Characteristic-grouped adiposity indicators for identifying metabolic syndrome in adolescents: develop and valid risk screening tools using dual population. Nutrients 12, 3165 (2020).
Magge, S. N. et al. The metabolic syndrome in children and adolescents: shifting the focus to cardiometabolic risk factor clustering. Pediatrics 140, e20171603 (2017).
Reinehr, T., de Sousa, G., Toschke, A. M. & Andler, W. Comparison of metabolic syndrome prevalence using eight different definitions: a critical approach. Arch. Dis. Child. 92, 1067–1072 (2007).
Cook, S., Weitzman, M., Auinger, P., Nguyen, M. & Dietz, W. H. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third national health and nutrition examination survey, 1988-1994. Arch. Pediatrics Adolesc. Med. 157, 821–827 (2003).
de Ferranti, S. D. et al. Prevalence of the metabolic syndrome in american adolescents: findings from the third national health and nutrition examination survey. Circulation 110, 2494–2497 (2004).
Vukovic, R. et al. Pediatric sims score: a new, simple and accurate continuous metabolic syndrome score for everyday use in pediatrics. PloS one 12, e0189232 (2017).
Eisenmann, J. C. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc. Diabetol. 7, 17 (2008).
Okosun, I. S., Lyn, R., Davis-Smith, M., Eriksen, M. & Seale, P. Validity of a continuous metabolic risk score as an index for modeling metabolic syndrome in adolescents. Ann. Epidemiol. 20, 843–851 (2010).
Gurka, M. J., Ice, C. L., Sun, S. S. & Deboer, M. D. A confirmatory factor analysis of the metabolic syndrome in adolescents: an examination of sex and racial/ethnic differences. Cardiovasc. Diabetol. 11, 1–10 (2012).
Luong, R. & Flake, J. K. Measurement invariance testing using confirmatory factor analysis and alignment optimization: a tutorial for transparent analysis planning and reporting. Psychol. Methods 28, 905–924 (2023).
Steinberger, J. et al. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the american heart association atherosclerosis, hypertension, and obesity in the young committee of the council on cardiovascular disease in the young; council on cardiovascular nursing; and council on nutrition, physical activity, and metabolism. Circulation 119, 628–647 (2009).
Lorenzo, C., Williams, K., Hunt, K. J. & Haffner, S. M. The national cholesterol education program–adult treatment panel III, international diabetes federation, and world health organization definitions of the metabolic syndrome as predictors of incident cardiovascular disease and diabetes. Diab. Care 30, 8–13 (2007).
Reaven, G. M. Role of insulin resistance in human disease. Diabetes 37, 1595–1607 (1988).
Gurka, M. J. et al. Independent associations between a metabolic syndrome severity score and future diabetes by sex and race: the atherosclerosis risk in communities study and jackson heart study. Diabetologia 60, 1261–1270 (2017).
Guo, Y. et al. Assessing the added predictive ability of a metabolic syndrome severity score in predicting incident cardiovascular disease and type 2 diabetes: the atherosclerosis risk in communities study and jackson heart study. Diabetol. Metab. Syndr. 10, 42 (2018).
Chuang, H. H. et al. Correlation between body composition and risk factors for cardiovascular disease and metabolic syndrome. Biofactors 38, 284–291 (2012).
Deng, F. et al. Association between apolipoprotein B/A1 ratio and coronary plaque vulnerability in patients with atherosclerotic cardiovascular disease: an intravascular optical coherence tomography study. Cardiovasc. Diabetol. 20, 1–13 (2021).
Ference, B. A. et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. a consensus statement from the european atherosclerosis society consensus panel. Eur. heart J. 38, 2459–2472 (2017).
Sheng, L. et al. Glycemic variability evaluated by Hba1c rather than fasting plasma glucose is associated with adverse cardiovascular events. Front. Endocrinol. 15, 1323571 (2024).
Maloberti, A. et al. The results of the urrah (Uric Acid Right for Heart Health) project: a focus on hyperuricemia in relation to cardiovascular and kidney disease and its role in metabolic dysregulation. High. Blood Press. Cardiovasc. Prev. 30, 411–425 (2023).
Taiwan National Health Research Institutes. 2010-2011 Nutrition and Health Survey in Taiwan: Materials and Methods. [(Accessed on 1 August 2024)]; Available Online: https://www.Hpa.Gov.Tw/Pages/List.Aspx?Nodeid=1773.
Lin, W. T. et al. Clustering of metabolic risk components and associated lifestyle factors: a nationwide adolescent study in Taiwan. Nutrients 11, 584 (2019).
Taiwan National Health Research Institutes. Nutrition and Health Survey in Taiwan. Survey Research Data Archive.[(Accessed on 1 August 2024)]; Available Online: https://Srda.Sinica.Edu.Tw/Browsingbydatatype_Result.Php?Category=Surveymethod&Type=1&Csid=4.
Taiwan Pediatric Association. The Statement of Taiwan Pediatric Association for Child and Adolescent Metabolic Syndrome, https://www.pediatr.org.tw/people/edu_info.asp?id=33 (2016).
Sachs, L., Batra, K. L. & Zimmermann, B. Medical implications of hyperuricemia. Med. Health R. I 92, 353–355 (2009).
Expert Panel on Integrated Guidelines for Cardiovascular, H. R. R. i., Children Adolescents, National Heart, Lung Blood, Institute Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128, S213–S256 (2011).
American Diabetes Association Professional Practice, C. 2 Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diab. Care 45, S17–S38 (2022).
Prince, R. L., Kuk, J. L., Ambler, K. A., Dhaliwal, J. & Ball, G. D. Predictors of metabolically healthy obesity in children. Diab. Care 37, 1462–1468 (2014).
Hooper, D., Coughlan, J. & Mullen, M. Structural equation modelling: guidelines for determining model fit. Electron J. Bus. Res. Methods 6, 53–60 (2008).
Kelly, A. S. et al. Predicting cardiovascular risk in young adulthood from the metabolic syndrome, its component risk factors, and a cluster score in childhood. Int. J. Pediatr. Obes. 6, e283–e289 (2011).
Moran, A. et al. Changes in insulin resistance and cardiovascular risk during adolescence: establishment of differential risk in males and females. Circulation 117, 2361–2368 (2008).
Tara, M. et al. Estrogen regulation of adiposity and fuel partitioning: evidence of genomic and non-genomic regulation of lipogenic and oxidative pathways. J. Biol. Chem. 280, 35983–35991 (2005).
Reue, K. & Wiese, C. B. Illuminating the mechanisms underlying sex differences in cardiovascular disease. Circul. Res. 130, 1747–1762 (2022).
O’Keeffe, L. M. et al. Sex-specific trajectories of molecular cardiometabolic traits from childhood to young adulthood. Heart 109, 674–685 (2023).
Meloni, A. et al. Gender differences and cardiometabolic risk: the importance of the risk factors. Int. J. Mol. Sci. 24, 1588 (2023).
DeBoer, M. D., Gurka, M. J., Woo, J. G. & Morrison, J. A. Severity of metabolic syndrome as a predictor of cardiovascular disease between childhood and adulthood: the princeton lipid research cohort study. J. Am. Coll. Cardiol. 66, 755–757 (2015).
DeBoer, M. D., Filipp, S. L. & Gurka, M. J. Use of a metabolic syndrome severity Z score to track risk during treatment of prediabetes: an analysis of the diabetes prevention program. Diab. Care 41, 2421–2430 (2018).
Acknowledgements
The adolescent NAHSIT survey data were obtained from the Nutrition and Health Survey in Taiwan (NAHSIT) on Junior and Senior High School Students, 2010–2011. This NAHSIT project was sponsored by the Food and Drug Administration, Department of Health, Executive Yuan (99TFDA-FS-408 and 100TFDA-FS-406). This nationwide survey was conducted by the Division of Preventive Medicine and Health Services Research, the Institute of Population Health Sciences of the National Health Research Institutes (NHRI). We thank the director Wen-Harn Pan and all members of the office of Nutrition Survey, the Division of Preventive Medicine and Health Services Research, the Institute of Population Health Sciences of NHRI for providing the dataset. The views expressed here are solely those of the authors. This research work was supported by the Taiwan Ministry of Science and Technology [MOST 103-2314-B-037-019-MY3, MOST 106-2314-B-037-021-MY3, and MOST 109-2314-B-037-070-MY3], the Taiwan National Science and Technology Council [NSTC-112-2314-B-037-083-MY3], and the Research Center for Precision Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan and by Kaohsiung Medical University Research Center Grant [KMU-TC113A01], and College Featured Research Projects (KMU-TB114007).
Author information
Authors and Affiliations
Contributions
C.H.L. and Y.T.C. conceived and designed the study. Y.T.C. and P.W.W. led the Project administration. Data curation and investigation were conducted by all authors (Y.T.C., P.W.W., P.R.H., S.T., W.T.L., C.Y.L., and W.C.T.). Y.T.C. and C.H.L. performed the formal analysis. The first draft of the manuscript was written by Y.T.C. and C.H.L., with all authors contributing to review and editing. C.H.L. supervised the study and obtained funding. All authors discussed the results and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent Statement
Informed assent and consent were collected from all student participants and their guardians to ensure voluntary participation and compliance with ethical standards in both studies. The Institutional Review Board of Kaohsiung Medical University Hospital approved the study protocol (approval no. KMUHIRB-20120103).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chin, YT., Wu, PW., Huang, PR. et al. Confirmatory-factor-analysis-derived metabolic syndrome risk score: development, validation, and clinical utility in dual adolescent populations. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04419-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04419-w