Abstract
Background
The perinatal period has been postulated to be a window of opportunities in preventing atopic disorders. Accumulating studies suggested that an association exists between gestational age (GA) and allergic diseases.
Methods
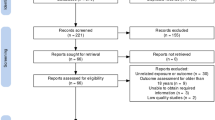
The meta-analysis of observational studies was conducted through a search of relevant literature until 31 December 2023 from PubMed, Embase, and Web of Science databases. Subgroup analyses and sensitivity analyses were performed to test the robustness and consistency of the observed associations.
Results
Thirty observational studies comprising 5,410,969 participants were included in the meta-analysis. The pooled estimates (odds ratio [OR]) of atopic dermatitis (AD) risk for early preterm, preterm and post-term birth were 0.75 (95% confidence interval [CI]: 0.68–0.82), 0.86 (95% CI: 0.81–0.93), 1.08 (95% CI: 1.03–1.14), respectively. Additionally, early preterm birth was suggestively associated with reduced risk of allergic rhinitis (AR) (OR: 0.84, 95% CI: 0.73–0.97).
Conclusion
Our study demonstrated that early preterm and preterm births were associated with a reduced risk of AD, while post-term birth was linked to an increased risk, with early preterm birth also suggestively associated with a reduced risk of AR.
Impact
-
This large-scale meta-analysis demonstrates that early preterm and preterm births are associated with a significantly reduced risk of atopic dermatitis (AD), while post-term birth is linked to an increased risk.
-
Early preterm birth is also suggestively associated with a lower risk of allergic rhinitis (AR), highlighting the nuanced role of gestational age in the development of allergic diseases.
-
These findings underscore the importance of the perinatal period as a critical window for allergy risk stratification and early prevention strategies in pediatric populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are publicly available and accessible.
References
Shin, Y. H. et al. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Allergy 78, 2232–2254 (2023).
Barker, D. J. The origins of the developmental origins theory. J. Intern Med 261, 412–417 (2007).
Siltanen, M., Kajosaari, M., Pohjavuori, M. & Savilahti, E. Prematurity at birth reduces the long-term risk of atopy. J. Allergy Clin. Immunol. 107, 229–234 (2001).
Siltanen, M. et al. Preterm birth reduces the incidence of atopy in adulthood. J. Allergy Clin. Immunol. 127, 935–942 (2011).
Korhonen, P. et al. Asthma and atopic dermatitis after early-, late-, and post-term birth. Pediatr. Pulmonol. 53, 269–277 (2018).
Haataja, P. et al. Asthma and atopic dermatitis in children born moderately and late preterm. Eur. J. Pediatr. 175, 799–808 (2016).
Mitselou, N. et al. Preterm birth reduces the risk of IgE sensitization up to early adulthood: A population-based birth cohort study. Allergy 77, 1570–1582 (2022).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339, b2700 (2009).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25, 603–605 (2010).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Chen, B. & Benedetti, A. Quantifying heterogeneity in individual participant data meta-analysis with binary outcomes. Syst. Rev. 6, 243 (2017).
Yuan, S. et al. Homocysteine, folate, and nonalcoholic fatty liver disease: a systematic review with meta-analysis and Mendelian randomization investigation. Am. J. Clin. Nutr. 116, 1595–1609 (2022).
Hamling, J., Lee, P., Weitkunat, R. & Ambuhl, M. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat. Med 27, 954–970 (2008).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101 (1994).
Olesen, A. B., Ellingsen, A. R., Olesen, H., Juul, S. & Thestrup-Pedersen, K. Atopic dermatitis and birth factors: historical follow up by record linkage. BMJ 314, 1003–1008 (1997).
Steffensen, F. H. et al. Low birth weight and preterm delivery as risk factors for asthma and atopic dermatitis in young adult males. Epidemiology 11, 185–188 (2000).
Katz, K. A., Pocock, S. J. & Strachan, D. P. Neonatal head circumference, neonatal weight, and risk of hayfever, asthma and eczema in a large cohort of adolescents from Sheffield, England. Clin. Exp. Allergy 33, 737–745 (2003).
Kerkhof, M. et al. Risk factors for atopic dermatitis in infants at high risk of allergy: the PIAMA study. Clin. Exp. Allergy 33, 1336–1341 (2003).
Mai, X. M. et al. Asthma, lung function and allergy in 12-year-old children with very low birth weight: a prospective study. Pediatr. Allergy Immunol. 14, 184–192 (2003).
Bernsen, R. M., de Jongste, J. C., Koes, B. W., Aardoom, H. A. & van der Wouden, J. C. Perinatal characteristics and obstetric complications as risk factors for asthma, allergy and eczema at the age of 6 years. Clin. Exp. Allergy 35, 1135–1140 (2005).
Linneberg, A., Simonsen, J. B., Petersen, J., Stensballe, L. G. & Benn, C. S. Differential effects of risk factors on infant wheeze and atopic dermatitis emphasize a different etiology. J. Allergy Clin. Immunol. 117, 184–189 (2006).
Mallen, C. D., Mottram, S., Wynne-Jones, G. & Thomas, E. Birth-related exposures and asthma and allergy in adulthood: a population-based cross-sectional study of young adults in North Staffordshire. J. Asthma 45, 309–312 (2008).
Govaere, E. et al. The prevalence, characteristics of and risk factors for eczema in Belgian schoolchildren. Pediatr. Dermatol 26, 129–138 (2009).
Kumar, R. et al. Gestational diabetes, atopic dermatitis, and allergen sensitization in early childhood. J. Allergy Clin. Immunol. 124, 1031–8.e1-4 (2009).
Kvenshagen, B., Jacobsen, M. & Halvorsen, R. Atopic dermatitis in premature and term children. Arch. Dis. Child 94, 202–205 (2009).
Lundholm, C., Ortqvist, A. K., Lichtenstein, P., Cnattingius, S. & Almqvist, C. Impaired fetal growth decreases the risk of childhood atopic eczema: a Swedish twin study. Clin. Exp. Allergy 40, 1044–1053 (2010).
Sonnenschein-van der Voort, A. M. et al. Fetal and infant growth and asthma symptoms in preschool children: the Generation R Study. Am. J. Respir. Crit. Care Med 185, 731–737 (2012).
Barbarot, S. et al. Lower risk of atopic dermatitis among infants born extremely preterm compared with higher gestational age. Br. J. Dermatol 169, 1257–1264 (2013).
Miyake, Y. & Tanaka, K. Lack of relationship between birth conditions and allergic disorders in Japanese children aged 3 years. J. Asthma 50, 555–559 (2013).
Tronnes, H., Wilcox, A. J., Lie, R. T., Markestad, T. & Moster, D. The association of preterm birth with severe asthma and atopic dermatitis: a national cohort study. Pediatr. Allergy Immunol. 24, 782–787 (2013).
Vrijlandt, E. J., Kerstjens, J. M., Duiverman, E. J., Bos, A. F. & Reijneveld, S. A. Moderately preterm children have more respiratory problems during their first 5 years of life than children born full term. Am. J. Respir. Crit. Care Med 187, 1234–1240 (2013).
Egeberg, A., Andersen, Y. M., Gislason, G., Skov, L. & Thyssen, J. P. Neonatal risk factors of atopic dermatitis in Denmark - Results from a nationwide register-based study. Pediatr. Allergy Immunol. 27, 368–374 (2016).
Yrjana, J. M. S., Koski, T., Torola, H., Valkama, M. & Kulmala, P. Very early introduction of semisolid foods in preterm infants does not increase food allergies or atopic dermatitis. Ann. Allergy Asthma Immunol. 121, 353–359 (2018).
Morata-Alba, J., Romero-Rubio, M. T., Castillo-Corullon, S. & Escribano-Montaner, A. Respiratory morbidity, atopy and asthma at school age in preterm infants aged 32-35 weeks. Eur. J. Pediatr. 178, 973–982 (2019).
Monir, R. L., Schoch, J. J., Garvan, C. W., Neu, J. & Lemas, D. J. Association between atopic dermatitis and race from infancy to early childhood: a retrospective cohort study. Int J. Dermatol 61, 727–732 (2022).
Gerner, T. et al. Differences in Occurrence, Risk Factors and Severity of Early-onset Atopic Dermatitis among Preterm and Term Children. Acta Derm. Venereol. 102, adv00737 (2022).
Braback, L. & Hedberg, A. Perinatal risk factors for atopic disease in conscripts. Clin. Exp. Allergy 28, 936–942 (1998).
Bager, P., Melbye, M., Rostgaard, K., Benn, C. S. & Westergaard, T. Mode of delivery and risk of allergic rhinitis and asthma. J. Allergy Clin. Immunol. 111, 51–56 (2003).
Crump, C., Sundquist, K., Sundquist, J. & Winkleby, M. A. Gestational age at birth and risk of allergic rhinitis in young adulthood. J. Allergy Clin. Immunol. 127, 1173–1179 (2011).
Mitselou, N. et al. Adverse pregnancy outcomes and risk of later allergic rhinitis-Nationwide Swedish cohort study. Pediatr. Allergy Immunol. 31, 471–479 (2020).
Li, Y. et al. Pre- and Postnatal Risk Factors in Relation to Allergic Rhinitis in School-Aged Children in China. Plos One 10, e0114022 (2015).
Loid, P. et al. A persistently high body mass index increases the risk of atopic asthma at school age. Acta Paediatr. 104, 707–712 (2015).
Zhu, T., Zhao, J., Qu, Y., Zhang, L. & Mu, D. Association of very preterm birth with decreased risk of eczema: A systematic review and meta-analysis. J. Am. Acad. Dermatol 78, 1142–1148 (2018).
Herberth, G. et al. Maternal immune status in pregnancy is related to offspring’s immune responses and atopy risk. Allergy 66, 1065–1074 (2011).
Strachan, D. P. Hay fever, hygiene, and household size. BMJ 299, 1259–1260 (1989).
Halling, A. S. et al. Skin TARC/CCL17 increase precedes the development of childhood atopic dermatitis. J. Allergy Clin. Immunol. 151, 1550–1557 (2023).
Garn, H. & Renz, H. Epidemiological and immunological evidence for the hygiene hypothesis. Immunobiology 212, 441–452 (2007).
Mitselou, N. et al. Cesarean delivery, preterm birth, and risk of food allergy: Nationwide Swedish cohort study of more than 1 million children. J. Allergy Clin. Immunol. 142, 1510–1514 (2018).
Pekkanen, J., Xu, B. & Jarvelin, M. R. Gestational age and occurrence of atopy at age 31-a prospective birth cohort study in Finland. Clin. Exp. Allergy 31, 95–102 (2001).
Acknowledgements
The authors sincerely thank the researchers and participants of the original articles for their collection and management of data resources.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82204843), the Medical and Health Science and Technology Program of Zhejiang Province (2023KY845), the Traditional Chinese Medicine Science and Technology Program of Zhejiang Province (2023ZR084), Youth Talent Support Program of Zhejiang Provincial Science and Technology Association (2024-HT-334), and Natural Science Youth Exploration Program of Zhejiang Chinese Medicine University (2023JKZKTS12).
Author information
Authors and Affiliations
Contributions
XZ, KL, DY, JC, and XJ were responsible for the statistical analysis. YM, JL, and XS contributed to the conceptualization and methodology. XZ, KL, DY, and YM were responsible for writing, reviewing, and editing the subsequent and final drafts of the manuscript. All authors had full access to the study data and held final responsibility for the decision to submit the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study is based on secondary analyses of previously published individual participant data (IPD). All original studies included had been independently registered and received ethics approval in accordance with the regulations of their respective countries and institutions.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, X., Liu, K., Chen, J. et al. Gestational age and the risk of allergic diseases: a systematic review and meta-analysis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04439-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04439-6
This article is cited by
-
From preterm protection to post-term predisposition: gestational age and the allergy spectrum
Pediatric Research (2025)