Abstract
Background
To investigate the prevalence of Celiac disease (CeD) in children and adolescents with SLE.
Methods
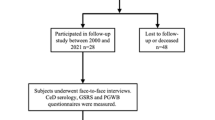
We completed a retrospective cohort study of children and adolescents with childhood-onset SLE (cSLE). We included patients who underwent CeD screening with tissue transglutaminase immunoglobulin A (tTG-IgA) serology within a year of cSLE diagnosis. Clinical and laboratory data were extracted from a dedicated lupus database, supplemented by chart review. CeD diagnosis was confirmed by duodenal histology. We calculated the prevalence of positive CeD serology, biopsy-confirmed CeD and CeD clinical features, and compared SLE features between CeD and non-CeD patients with Fisher’s exact tests.
Results
Three hundred children with SLE underwent CeD screening. Thirteen (4%) had positive tTG-IgA serology. Of those, ten (77%) underwent endoscopy and eight had histopathologic evidence of CeD (3% of cSLE cohort). Among patients with biopsy confirmed CeD, only 50% had gastrointestinal symptoms. There was no difference in prevalence of cSLE features between those with and without CeD.
Conclusion
Biopsy-confirmed CeD was three times prevalent in children and adolescents with cSLE than reported in the general pediatric population. Only half of cSLE patients with CeD had gastrointestinal symptoms, highlighting the importance of screening in the cSLE population.
Impact
-
The incidence of celiac disease has increased over the past decades, particularly in people with comorbid autoimmune diseases.
-
Celiac disease is three times more prevalent among children with systemic lupus erythematosus compared to the general pediatric population.
-
Half of childhood-onset SLE patients with biopsy confirmed celiac disease were asymptomatic, highlighting the importance of routine CeD screening in the cSLE population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and analyzed during this study are available from the corresponding author on reasonable request.
References
Tang, S. P., Lim, S. C. & Arkachaisri, T. Childhood-onset systemic lupus erythematosus: Southeast Asian perspectives. J. Clin. Med 10, 1–9 (2021).
Tian, X.-P., Zhang, X. & Lee, T.-Y. Gastrointestinal involvement in systemic lupus erythematosus: Insight into pathogenesis, diagnosis and treatment. World J. Gastroenterol. 16, 2971–2977 (2010).
Poddighe, D. et al. Celiac Disease in Juvenile Idiopathic Arthritis and Other Pediatric Rheumatic Disorders. J. Clin. Med 11, 1089 (2022).
Smith, A., Johnson, N., Luca, N., Veeramreddy, D. & Schmeling, H. Celiac Disease in Children Diagnosed with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 69, (2017). https://acrabstracts.org/abstract/celiac-disease-in-children-diagnosed-with-juvenile-idiopathic-arthritis/. Accessed October 12, 2025.
Rubio-Tapia, A., Hill, I. D., Kelly, C. P., Calderwood, A. H. & Murray, J. A. ACG clinical guidelines: Diagnosis and management of celiac disease. Am. J. Gastroenterol. 108, 656–676 (2013).
Oberhuber, G. Histopathology of Celiac Disease. Biomed. Pharmacother. 54 (2000).
Lebwohl, B. & Rubio-Tapia, A. Epidemiology, Presentation, and Diagnosis of Celiac Disease. Gastroenterology. 160, 63–75 (2021).
Sahin, Y. Celiac disease in children: A review of the literature. World J. Clin. Pediatr. 10, 53–71 (2021).
Esteve, M. et al. Case-finding in primary care for coeliac disease: Accuracy and cost-effectiveness of a rapid point-of-care test. U. Eur. Gastroenterol. J. 6, 855–865 (2018).
Smyth, D. J. et al. Shared and Distinct Genetic Variants in Type 1 Diabetes and Celiac Disease. N. Engl. J. Med. 359, 2767–2777 (2008).
Volta, U., Tovoli, F. & Caio, G. Clinical and immunological features of celiac disease in patients with Type 1 diabetes mellitus. Exp. Rev. Gastroenterol. Hepatol. 5, 479–487 (2011).
Dubé, C. et al. The prevalence of celiac disease in average-risk and at-risk Western European populations: A systematic review. Gastroenterology 128, (2005).
Fasano, A. et al. Prevalence of Celiac Disease in At-Risk and Not-At-Risk Groups in the United States A Large Multicenter Study. Arch. Intern. Med. 163, (2003).
Mäki, M. et al. Prevalence of Celiac Disease among Children in Finland. N Engl J Med. 25, (2003).
Pham-Short, A. et al. Screening for celiac disease in type 1 diabetes: A systematic review. Pediatrics 136, e170–e176 (2015).
Bingley, P. J. et al. Undiagnosed coeliac disease at age seven: Population based prospective birth cohort study. Br. Med J. 328, 322–323 (2004).
Geanina, I. et al. Coexistence of celiac disease and systemic lupus erythematosus in a 6-year-old girl-case report. Rev. Med Chir. Soc. Med Nat. Iasi 119, 78–91 (2015).
Shamseya, A. M., Elsayed, E. H. & Donia, H. M. Study of serology and genetics of celiac disease in patients with juvenile systemic lupus erythematosus ‘celiac in juvenile systemic lupus’. Eur. J. Gastroenterol. Hepatol. 32, 1322–1327 (2020).
AlEnzi, F. et al. The Value of Screening for Celiac Disease in Systemic Lupus Erythematosus: A Single Experience of a Tertiary Medical Center. Rheumatol. Ther. 7, 649–656 (2020).
Lupu, V. V. et al. Connection between Celiac Disease and Systemic Lupus Erythematosus in Children—A Development Model of Autoimmune Diseases Starting from What We Inherit to What We Eat. Nutrients. 15, 2535 (2023).
Husby, S. et al. European Society Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for Diagnosing Coeliac Disease 2020. J. Pediatr. Gastroenterol. Nutr. 70, 141–156 (2020).
Hill, I. D. et al. Guideline for the Diagnosis and Treatment of Celiac Disease in Children: Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 40, 1–19 (2005).
Sahin, Y. et al. Serological screening for celiac disease in children with systemic lupus erythematosus. Eur. J. Rheumatol. 6, 142–145 (2019).
Fonseca, A. R., Rodrigues, M. C. F., Sztajnbok, F. R., Land, M. G. P. & De Oliveira, S. K. F. Comparison among ACR1997, SLICC and the new EULAR/ACR classification criteria in childhood-onset systemic lupus erythematosus. Adv. Rheumatol. 59, 1–9 (2019).
Aringer, M. et al. 2019 European League Against Rheumatism/ American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 78, 1151–1159 (2019).
The Hospital For Sick Children, T. C Change in Methodology in the Autoimmune Laboratory/Division of Pathology. Bull. - ELISA CIA change Feb 29, 2016 (2016).
The Hospital For Sick Children, T. C. QUANTA Flash h-tTG IgA Directional Insert. QUANTA Flash h-tTG IgA Directional Insert - Since Feb, 2016 (2016).
Statistics Canada. Ethnic Origin Reference Guide, Census of Population, 2016. (Statistics Canada, 2017).
Singh, P. et al. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 16, 823–836.e2 (2018).
Wang, Q., Jia, S., Lu, Q. & Zhao, M. Systemic lupus erythematosus is associated with the risk of coeliac disease: a Mendelian randomisation study. Autoimmunity 56, 2250103 (2023).
Soltani, Z. et al. Celiac disease in patients with systemic lupus erythematosus. Reumatologia 59, 85–89 (2021).
Levy, D. M. et al. The 1000 Canadian Faces of Lupus: Influence of Ethnicity on Disease in the Pediatric Cohort. Arthritis Care Res 65, 152–160 (2013).
Rashid, M. et al. Celiac Disease: Evaluation of the Diagnosis and Dietary Compliance in Canadian Children. Pediatrics 116, e754–e759 (2005).
Khatib, M., Baker, R. D., Ly, E. K., Kozielski, R. & Baker, S. S. Presenting Pattern of Pediatric Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 62, 60–63 (2016).
Tapsas, D., Hollén, E., Stenhammar, L. & Fälth-Magnusson, K. The clinical presentation of coeliac disease in 1030 Swedish children: Changing features over the past four decades. Digestive Liver Dis. 48, 16–22 (2016).
Nurminen, S., Kivelä, L., Huhtala, H., Kaukinen, K. & Kurppa, K. Extraintestinal manifestations were common in children with coeliac disease and were more prevalent in patients with more severe clinical and histological presentation. Acta Paediatr. 108, 681–687 (2019).
Mauro, A. et al. Gastrointestinal Involvement in Children with Systemic Lupus Erythematosus. Children (Basel). 10, 309 (2023).
Mahmud, F. H. et al. Celiac Disease in Type 1 Diabetes Mellitus in a North American Community: Prevalence, Serologic Screening, and Clinical Features. Mayo Clin. Proc. 80, 1429–1434 (2005).
Sud, S. et al. Celiac Disease and Pediatric Type 1 Diabetes: Diagnostic and Treatment Dilemmas. Int J. Pediatr. Endocrinol. 2010, 161285 (2010).
Mollazadegan, K. et al. A Population-Based Study of the Risk of Diabetic Retinopathy in Patients With Type 1 Diabetes and Celiac Disease. Diabetes Care 36, 316–321 (2013).
Mollazadegan, K. et al. Risk of renal disease in patients with both type 1 diabetes and coeliac disease. Diabetologia 57, 1339–1345 (2014).
Nikniaz, Z., Abbasalizad Farhangi, M. & Nikniaz, L. Systematic Review With Meta-analysis of the Health-related Quality of Life in Children With Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 70, 468–477 (2020).
Coburn, S. S., Puppa, E. L. & Blanchard, S. Psychological comorbidities in childhood celiac disease: A systematic review. J. Pediatr. Gastroenterol. Nutr. 69, E25–E33 (2019).
Wagner, G. et al. Quality of life in adolescents with treated coeliac disease: influence of compliance and age at diagnosis. J. Pediatr. Gastroenterol. Nutr. 47, 555–561 (2008).
Whitaker, J. K. H., West, J., Holmes, G. K. T. & Logan, R. F. A. Patient perceptions of the burden of coeliac disease and its treatment in the UK. Aliment Pharm. Ther. 29, 1131–1136 (2009).
Kamphuis, S. & Silverman, E. D. Prevalence and burden of pediatric-onset systemic lupus erythematosus. Nat. Rev. Rheumatol. 6, 538-546 (2010).
Knight, A. et al. Depression and anxiety and their association with healthcare utilization in pediatric lupus and mixed connective tissue disease patients: A cross-sectional study. Pediatr. Rheumatol. 12, 1–12 (2014).
Roma, E. et al. Dietary compliance and life style of children with coeliac disease. J. Hum. Nutr. Dietetics 23, 176–182 (2010).
Dowhaniuk, J. K. et al. The Gluten Free Diet: Assessing Adherence in a Pediatric Celiac Disease Population. J. Can. Assoc. Gastroenterol. 3, 67–73 (2020).
Hall, N. J., Rubin, G. & Charnock, A. Systematic review: Adherence to a gluten-free diet in adult patients with coeliac disease. Aliment Pharm. Ther. 30, 315–330 (2009).
Högberg, L., Grodzinsky, E. & Stenhammar, L. Better dietary compliance in patients with coeliac disease diagnosed in early childhood. Scand. J. Gastroenterol. 38, 751–754 (2003).
Author contributors:
Oscar Mwizerwa, conceptualized and designed the study, collected data, drafted the initial manuscript, and critically reviewed and revised the manuscript. Andrea M. Knight, Deborah M. Levy and Holly Convery critically reviewed and revised the manuscript. Daniela Dominguez and Kendal Thompson collected data, critically reviewed and revised the manuscript. Nicholas Gold carried out data analysis and critically reviewed and revised the manuscript. Catharine M. Walsh critically reviewed and revised the manuscript for important intellectual content. Linda T. Hiraki conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed and revised the manuscript for important intellectual content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the institution Research Ethics Board (REB number: 1000079489). As participants were enrolled in other studies (i.e. either Lupus Biorepository and/or The 1000 Canadian Faces of Lupus Studies), a waiver of consent has been approved by Hospital REB for the chart review of the larger cohort. Consent was obtained only from participants with biopsy-confirmed CeD and who were still active patients in the Lupus clinic.
Competing interests
The authors declare no competing interests. L.T.H. holds a Canada Research Chair (Tier 2) in Genetics of Rare Systemic Inflammatory Diseases, and research is supported by Childhood Arthritis and Rheumatology Research Alliance (CARRA), Lupus Research Alliance (LRA), U.S. Department of Defense, Lupus Foundation of America, Gary Hurvitz Centre for Brain & Mental Health Catalyst Grant. A.M.K. is supported by a Canada Research Chair (Tier 2) in Mental Health and Chronic Disease of Childhood, and Lupus Research Alliance Career Development Award.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mwizerwa, O., Knight, A.M., Dominguez, D. et al. Celiac disease is more prevalent among children and adolescents with systemic lupus erythematosus. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04491-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04491-2