Abstract
Background
High average total fluid intakes in the first week after birth are linked to adverse outcomes in preterm infants, including necrotizing enterocolitis (NEC) and bronchopulmonary dysplasia (BPD). Relative contributions of enteral and parenteral fluids remain unclear.
Objective
Evaluate associations between average enteral, parenteral, and total fluid intake in the first postnatal week and morbidity and mortality in preterm newborns.
Methods
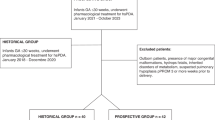
In this retrospective study of 185 infants born ≤30 weeks or ≤1250 g who survived seven days in a level IV NICU, we assessed relationships between fluid intake and adverse outcomes, including mortality, length of stay (LOS), NEC, and BPD.
Results
Each 10 mL/kg/day increase in enteral intake averaged over the first postnatal week was associated with 30% lower odds of BPD, 35% lower odds of mortality (aOR 0.70, 95% CI 0.58–0.85; aOR 0.65, 95% CI 0.46–0.93), and shorter LOS (−4.77 days, 95% CI −7.26, −2.29). Higher average enteral feeds were not associated with adverse outcomes. Higher average parenteral and total fluid intakes were associated with increased odds of BPD, mortality, and prolonged LOS.
Conclusion
Higher average enteral intake in the first week is associated with improved outcomes in preterm infants.
Impact
-
Previous research on extremely low birthweight infants reported that high total fluid intake within the first week after birth is associated with increased risk of adverse outcomes
-
The relative contributions of parenteral fluid versus enteral feeding volumes have not been evaluated.
-
Among neonates born at ≤30 gestational weeks or ≤1250 g, higher enteral intake was associated with decreased odds of mortality, bronchopulmonary dysplasia, and a shorter length of stay.
-
Higher parenteral fluid intake and higher total fluid intake were associated with increased odds of adverse outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data described in the manuscript and/or analyzed during the current study will be made available upon reasonable request to the corresponding author.
References
Stephens, B. E. et al. Fluid regimens in the first week of life may increase risk of patent ductus arteriosus in extremely low birth weight infants. J. Perinatol. 28, 123–128 (2008).
Oh, W. et al. Association between fluid intake and weight loss during the first ten days of life and risk of bronchopulmonary dysplasia in extremely low birth weight infants. J. Pediatr. 147, 786–790 (2005).
Soullane, S. et al. Fluid status in the first 10 days of life and death/bronchopulmonary dysplasia among preterm infants. Pediatr. Res. 90, 353–358 (2021).
Lin, B. et al. Enteral feeding/total fluid intake ratio is associated with risk of bronchopulmonary dysplasia in extremely preterm infants. Front. Pediatr. 10, 899785 (2022).
Abrams, S. A., Schanler, R. J., Lee, M. L. & Rechtman, D. J. Greater mortality and morbidity in extremely preterm infants fed a diet containing cow milk protein products. Breastfeed. Med. 9, 281–285 (2014).
Meinzen-Derr, J. et al. Role of human milk in extremely low birth weight infants’ risk of necrotizing enterocolitis or death. J. Perinatol. 29, 57–62 (2009).
Walsh V. et al. Early full enteral feeding for preterm or low birth weight infants. Cochrane Database Syst. Rev. 12, CD013542 (2020).
Nangia, S., Vadivel, V., Thukral, A. & Saili, A. Early total enteral feeding versus conventional enteral feeding in stable very-low-birth-weight infants: a randomised controlled trial. Neonatology 115, 256–262 (2019).
Young, L., Oddie, S. J. & McGuire, W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst. Rev. 1, CD001970 (2022).
Morgan, J., Bombell, S. & McGuire, W. Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants. Cochrane Database Syst. Rev. 2013, CD000504 (2013).
Henderson, G., Craig, S., Brocklehurst, P. & McGuire, W. Enteral feeding regimens and necrotising enterocolitis in preterm infants: a multicentre case–control study. Arch. Dis. Child. Fetal Neonatal Ed. 94, F120–F123 (2009).
Patole, S. & De Klerk, N. Impact of standardised feeding regimens on incidence of neonatal necrotising enterocolitis: a systematic review and meta-analysis of observational studies. Arch. Dis. Child. Fetal Neonatal Ed. 90, F147–F151 (2005).
Viswanathan, S. et al. Standardized slow enteral feeding protocol and the incidence of necrotizing enterocolitis in extremely low birth weight infants. J. Parenter. Enter. Nutr. 39, 644–654 (2015).
Walsh, V. & McGuire, W. Immunonutrition for preterm infants. Neonatology 115, 398–405 (2019).
Chitale, R. et al. Early enteral feeding for preterm or low birth weight infants: a systematic review and meta-analysis. Pediatrics 150, e2022057092E (2022).
Alshaikh, B., Dharel, D., Yusuf, K. & Singhal, N. Early total enteral feeding in stable preterm infants: a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 34, 1479–1486 (2021).
Leaf, A. et al. Early or delayed enteral feeding for preterm growth-restricted infants: a randomized trial. Pediatrics 129, e1260–e1268 (2012).
Sullivan, S. et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J. Pediatr. 156, 562–567.e1 (2010).
Cristofalo, E. A. et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J. Pediatr. 163, 1592–1595.e1 (2013).
Schanler, R. J., Lau, C., Hurst, N. M. & Smith, E. O. Randomized trial of donor human milk versus preterm formula as substitutes for mothers’ own milk in the feeding of extremely premature infants. Pediatrics 116, 400–406 (2005).
Lucas, A. & Cole, T. J. Breast milk and neonatal necrotising enterocolitis. Lancet 336, 1519–1523 (1990).
Valentine, G. C., Umoren, R. A. & Perez, K. M. Early inadequate or excessive weight loss: a potential contributor to mortality in premature newborns in resource-scarce settings? Pediatr. Neonatol. 62, 237–239 (2021).
Ågren, J., Sjörs, G. & Sedin, G. Transepidermal water loss in infants born at 24 and 25 weeks of gestation. Acta Paediatr. 87, 1185–1190 (1998).
Abiramalatha, T., Thomas, N. & Thanigainathan, S. High versus standard volume enteral feeds to promote growth in preterm or low birth weight infants. Cochrane Database Syst. Rev. 3, CD012413 (2021).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Ann. Surg. 187, 1–7 (1978).
Walsh, M. C. & Kliegman, R. M. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr. Clin. North Am. 33, 179–201 (1986).
Huber, P. J. & Ronchetti E. M. Robust Statistics. (Wiley, 2009).
Tukey, J. W. The future of data analysis. Ann. Math. Stat. 33, 1–67 (1962).
Vardhelli, V. et al. Comparison of CRIB-II with SNAPPE-II for predicting survival and morbidities before hospital discharge in neonates with gestation ≤ 32 weeks: a prospective multicentric observational study. Eur. J. Pediatr. 181, 2831–2838 (2022).
Reid, S., Bajuk, B., Lui, K. & Sullivan, E. A. Comparing CRIB-II and SNAPPE-II as mortality predictors for very preterm infants. J. Paediatr. Child Health 51, 524–528 (2015).
Youssef, M. R. L. Clinical Risk Index for Babies (CRIB II) scoring system in prediction of mortality in premature babies. J. Clin. Diagn. Res. (2015).
Valentine, G. C. et al. Postnatal maximal weight loss, fluid administration, and outcomes in extremely preterm newborns. J. Perinatol. 42, 1008–1016 (2022).
Adrogué, H. J. & Madias, N. E. Hypernatremia. N. Engl. J. Med. 342, 1493–1499 (2000).
Rozance, P. J. & Hay, W. W. Neonatal hyperglycemia. Neoreviews 11, e632–e639 (2010).
R Core Team. R: A language and environment for statistical computing. (2019).
Razzaghy, J. et al. Early and exclusive enteral nutrition in infants born very preterm. Arch. Dis. Child Fetal Neonatal Ed. 109, 378–383 (2024).
Nangia, S. et al. Early total enteral feeding in stable very low birth weight infants: a before and after study. J. Trop. Pediatr. 64, 24–30 (2018).
Quigley, M., Embleton, N. D. & McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 7, CD002971 (2019).
Wiechers, C. et al. Optimizing early neonatal nutrition and dietary pattern in premature infants. Int. J. Environ. Res. Public Health 18, 7544 (2021).
Hermansen, M. C. & Goetz Hermansen, M. Intravascular catheter complications in the neonatal intensive care unit. Clin. Perinatol. 32, 141–156 (2005).
Colacchio, K., Deng, Y., Northrup, V. & Bizzarro, M. J. Complications associated with central and non-central venous catheters in a neonatal intensive care unit. J. Perinatol. 32, 941–946 (2012).
Alobaidi, R. et al. Association between fluid balance and outcomes in critically Ill children. JAMA Pediatr. 172, 257 (2018).
Author information
Authors and Affiliations
Contributions
GV and KP designed research; O.B., G.V., and S.K. conducted research; O.B. and T.W. analyzed data; O.B., G.V., and K.P. wrote the paper; O.B., G.V., S.K., S.J., T.W., and K.P. had responsibility for final content. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
Patient consent was not required as this is a retrospective clinical study approved using a de-identified database and approved through the University of Washington Institutional Review Board (STUDY00006091). The study was performed in accordance with the Declaration of Helsinki (revised 2013).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brandon, O.C., Valentine, G.C., Kolnik, S.E. et al. Early feeding and fluid volume associations with adverse in-hospital outcomes among premature newborns. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04494-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04494-z