Abstract
Background
Premature birth can pose challenges to parent-infant attachment and increase parental anxiety. Music therapy has been proposed as an intervention, but its effectiveness remains unclear.
Methods
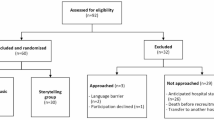
Six databases (Cochrane Library, Web of Science, EBSCO, Embase, PubMed, and Scopus) were searched until January 15, 2025. Eligible studies were randomized controlled trials that evaluated the effects of music intervention versus routine care on parental anxiety and parent-infant attachment in caring for premature infants. Quality assessment was conducted using the Cochrane Risk of Bias 2 tool. Random-effects meta-analyses were performed with heterogeneity assessed via I2 statistics and Q tests. The Grading of Recommendations, Assessment, Development and Evaluation approach evaluated overall evidence quality.
Results
After comprehensive screening, 13 randomized controlled trials published between 2014 and 2024 were included, encompassing 1034 participants with preterm infants. The meta-analysis revealed no statistically significant improvement in parent-infant attachment or parental anxiety with music therapy compared to conventional care. However, subgroup analysis indicated that frequent music therapy interventions (≥once daily) positively influenced parent-infant attachment (SMD = −1.08, 95% CI: [−1.92, −0.24], p = 0.01).
Conclusions
Overall, music therapy may not reduce parental anxiety or improve attachment, but frequent interventions demonstrated promising potential and warrant further investigation.
Registration number
PROSPERO CRD42025643424.
Impact statement
-
This review indicates that music therapy, compared to standard care, shows no significant effects on parent-infant attachment or parental anxiety in the care of premature infants.
-
However, more frequent (≥once daily) music therapy shows more promising results in improving parent-infant attachment, suggesting the importance of intervention intensity.
-
These insights inform the development of targeted daily therapy protocol to enhance preterm care outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All the sources of data are publicly available and referenced in the document.
References
Calvert, C. et al. Changes in preterm birth and stillbirth during COVID-19 lockdowns in 26 countries. Nat. Hum. Behav. 7, 529–544 (2023).
Chawanpaiboon, S. et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health 7, e37–e46 (2019).
Schetter, C. D. & Glynn, L. M. Stress in pregnancy: empirical evidence and theoretical issues to guide interdisciplinary research. Handb. Stress Sci. Biol. Psychol. Health 321, 343 (2011).
Bruce, L., Béland, D. & Bowen, A. MotherFirst: developing a maternal mental health strategy in Saskatchewan. Healthc. Policy 8, 46 (2012).
Bérard, A., Le Tiec, M. & De Vera, M. A. Study of the costs and morbidities of late-preterm birth. Arch. Dis. Child. Fetal Neonatal Ed. 97, F329–F334 (2012).
Singer, L. T. et al. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA 281, 799–805 (1999).
Korvenranta, E. et al. Impact of very preterm birth on health care costs at five years of age. Pediatrics 125, e1109–e1114 (2010).
Petrou, S., Abangma, G., Johnson, S., Wolke, D. & Marlow, N. Costs and health utilities associated with extremely preterm birth: evidence from the EPICure study. Value Health 12, 1124–1134 (2009).
Ukpong, D., Fatoye, F., Oseni, S. & Adewuya, A. Post partum emotional distress in mothers of preterm infants: a controlled study. East Afr. Med. J. 80, 289–292 (2003).
Schappin, R., Wijnroks, L., Uniken Venema, M. M. A. T. & Jongmans, M. J. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS ONE 8, 1–19 (2013).
Ionio, C. et al. Mothers and fathers in NICU: the impact of preterm birth on parental distress. Eur. J. Psychol. 12, 604 (2016).
Winter, L. et al. Depression, posttraumatic stress and relationship distress in parents of very preterm infants. Arch. Womens Ment. Health 21, 445–451 (2018).
Busse, M., Stromgren, K., Thorngate, L. & Thomas, K. A. Parents’ responses to stress in the neonatal intensive care unit. Crit. Care Nurse 33, 52–59 (2013).
Zelkowitz, P., Na, S., Wang, T., Bardin, C. & Papageorgiou, A. Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age. Acta Paediatr. 100, 700–704 (2011).
Evans, T., Whittingham, K. & Boyd, R. What helps the mother of a preterm infant become securely attached, responsive and well-adjusted?. Infant Behav. Dev. 35, 1–11 (2012).
Aktar, E. & Bögels, S. M. Exposure to parents’ negative emotions as a developmental pathway to the family aggregation of depression and anxiety in the first year of life. Clin. Child Fam. Psychol. Rev. 20, 369–390 (2017).
Groh, A. M., Fearon, R. P., van IJzendoorn, M. H., Bakermans-Kranenburg, M. J. & Roisman, G. I. Attachment in the early life course: meta-analytic evidence for its role in socioemotional development. Child Dev. Perspect. 11, 70–76 (2017).
Brumariu, L. E. Parent-child attachment and emotion regulation. New Dir. Child Adolesc. Dev. 148, 31–45 (2015).
Trumello, C. et al. Mothers’ depression, anxiety, and mental representations after preterm birth: a study during the infant’s hospitalization in a neonatal intensive care unit. Front. Public Health 6, 359 (2018).
Slomian, J., Honvo, G., Emonts, P., Reginster, J.-Y. & Bruyère, O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health 15, 1745506519844044 (2019).
Lutkiewicz, K., Bieleninik, Ł, Cieślak, M. & Bidzan, M. Maternal–infant bonding and its relationships with maternal depressive symptoms, stress and anxiety in the early postpartum period in a Polish sample. Int. J. Environ. Res. Public. Health 17, 5427 (2020).
Ghetti, C. M. et al. Effect of music therapy on parent-infant bonding among infants born preterm: a randomized clinical trial. JAMA Netw. Open 6, e2315750 (2023).
Amini, E., Rafiei, P., Zarei, K., Gohari, M. & Hamidi, M. Effect of lullaby and classical music on physiologic stability of hospitalized preterm infants: a randomized trial. J. Neonatal Perinat. Med. 6, 295–301 (2013).
Edwards, J. Music Therapy and Parent-Infant Bonding (Oxford University Press, 2011).
Haslbeck, F. B., Schmidli, L., Bucher, H. U. & Bassler, D. Music is life—follow-up qualitative study on parental experiences of creative music therapy in the neonatal period. Int. J. Environ. Res. Public. Health 18, 6678 (2021).
Hillecke, T., Nickel, A. & Bolay, H. V. Scientific perspectives on music therapy. Ann. N. Y. Acad. Sci. 1060, 271–282 (2005).
Haslbeck, F. B. et al. Creative music therapy to promote brain function and brain structure in preterm infants: a randomized controlled pilot study. NeuroImage Clin. 25, 102171 (2020).
Epstein, S. et al. Preterm infants with severe brain injury demonstrate unstable physiological responses during maternal singing with music therapy: a randomized controlled study. Eur. J. Pediatr. 180, 1403–1412 (2021).
Filippa, M. et al. Maternal singing sustains preterm hospitalized newborns’ autonomic nervous system maturation: an RCT. Pediatr. Res. 95, 1110–1116 (2024).
Nakata, T. & Trehub, S. E. Infants’ responsiveness to maternal speech and singing. Infant Behav. Dev. 27, 455–464 (2004).
Pavlicevic, M. Improvisation in music therapy: Human communication in sound. J. Music Ther. 37, 269–285 (2000).
Haslbeck, F. & Hugoson, P. Sounding together: family-centered music therapy as facilitator for parental singing during skin-to-skin contact. Early Vocal Contact Preterm Infant Brain Dev Bridg. Gaps Res. Pract. 217, 238 (2017).
Edwards, J. The use of music therapy to promote attachment between parents and infants. Arts Psychother. 38, 190–195 (2011).
Menke, B. M., Hass, J., Diener, C. & Pöschl, J. Family-centered music therapy—Empowering premature infants and their primary caregivers through music: Results of a pilot study. PLoS ONE 16, e0250071 (2021).
Xiao, W. & Luo, X. Observations on the clinical effects of music therapy on premature infants in neonatal intensive care units. Noise Health 26, 436–443 (2024).
Yakobson, D. et al. Effects of live music therapy on autonomic stability in preterm infants: a cluster-randomized controlled trial. Children 8, 1077 (2021).
Gaden, T. S. et al. Short-term music therapy for families with preterm infants: a randomized trial. Pediatrics 149, e2021052797 (2022).
Corrigan, M., Keeler, J., Miller, H., Naylor, C. & Diaz, A. Music therapy and family-integrated care in the NICU: using heartbeat-music interventions to promote mother–infant bonding. Adv. Neonatal Care 22, E159–E168 (2022).
Ettenberger, M. et al. Music therapy with premature infants and their caregivers in Colombia–A mixed methods pilot study including a randomized trial. Voices World Forum Music Ther. 14, (2014).
Kraft, K. E. et al. Maternal anxiety, infant stress, and the role of live-performed music therapy during NICU stay in The Netherlands. Int. J. Environ. Res. Public. Health 18, 7077 (2021).
Ribeiro, M. K. A. et al. Music therapy intervention in cardiac autonomic modulation, anxiety, and depression in mothers of preterms: randomized controlled trial. BMC Psychol. 6, 57 (2018).
Kostilainen, K., Mikkola, K., Erkkilä, J. & Huotilainen, M. Effects of maternal singing during kangaroo care on maternal anxiety, wellbeing, and mother-infant relationship after preterm birth: a mixed methods study. Nord. J. Music Ther. 30, 357–376 (2021).
Chandler, J., Cumpston, M., Li, T., Page, M. J. & Welch, V. Cochrane Handbook for Systematic Reviews of Interventions (Hoboken Wiley, 2019).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. risma Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int. J. Surg. 8, 336–341 (2010).
Locke, A. & Kanekar, S. Imaging of premature infants. Clin. Perinatol. 49, 641–655 (2022).
Haslbeck, F. Music therapy with preterm infants—theoretical approach and first practical experience. Music Ther. Today 5, 1–15 (2004).
Higgins, J. T., Li, T., Deeks, J. J. (eds) Chapter 6: Choosing Effect Measures and Computing Estimates of Effect 2nd edn 143–176 (Chichester, UK John Wiley Sons, 2019).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Prick, A.-E. J. et al. Effects of a music therapy and music listening intervention for nursing home residents with dementia: a randomized controlled trial. Front. Med. 11, 1304349 (2024).
Yue, W., Han, X., Luo, J., Zeng, Z. & Yang, M. Effect of music therapy on preterm infants in neonatal intensive care unit: systematic review and meta-analysis of randomized controlled trials. J. Adv. Nurs. 77, 635–652 (2021).
Schaefer, H.-E. Music-evoked emotions—current studies. Front. Neurosci. 11, 600 (2017).
Stegemöller, E. L. Exploring a neuroplasticity model of music therapy. J. Music Ther. 51, 211–227 (2014).
Chaudhury, S., Nag, T. C., Jain, S. & Wadhwa, S. Role of sound stimulation in reprogramming brain connectivity. J. Biosci. 38, 605–614 (2013).
Haslbeck, F. B. & Bassler, D. Music from the very beginning—a neuroscience-based framework for music as therapy for preterm infants and their parents. Front. Behav. Neurosci. 12, 112 (2018).
Riley, M., Colson, T. L. & Smothers, M. Music therapy’s role in the education system. Ky. Teach. Educ. J. J. Teach. Educ. Div. Ky. Counc. Except. Child. 6, 5 (2019).
Koelsch, S. A neuroscientific perspective on music therapy. Ann. N. Y. Acad. Sci. 1169, 374–384 (2009).
Gibson, E. J. Exploratory behavior in the development of perceiving, acting, and the acquiring of knowledge. Annu. Rev. Psychol. 39, 1–42 (1988).
Kisilevsky, B. S. et al. Effects of experience on fetal voice recognition. Psychol. Sci. 14, 220–224 (2003).
Swain, J. E., Lorberbaum, J. P., Kose, S. & Strathearn, L. Brain basis of early parent–infant interactions: psychology, physiology, and in vivo functional neuroimaging studies. J. Child Psychol. Psychiatry 48, 262–287 (2007).
Schore, A. N. Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Ment. Health J. Off. Publ. World Assoc. Infant Ment. Health 22, 7–66 (2001).
Dileo, C. & Bradt, J. Medical Music Therapy: A Meta-Analysis & Agenda for Future Research (Jeffrey Books, 2005).
Kong, H.-K. & Karahalios, K. Parental perceptions, experiences, and desires of music therapy. AMIA. Annu. Symp. Proc. 2016, 1870 (2017).
Rolvsjord, R. & Stige, B. Concepts of context in music therapy. Nord. J. Music Ther. 24, 44–66 (2015).
Lee, J. Y., Lee, J. H., Yeon, G. M. & Jung, Y. J. Parental anxiety regarding premature infants and factors affecting parental concern. J. Spec. Pediatr. Nurs. 24, e12266 (2019).
Baia, I. et al. Parenting very preterm infants and stress in Neonatal Intensive Care Units. Early Hum. Dev. 101, 3–9 (2016).
Montirosso, R., Provenzi, L., Calciolari, G., Borgatti, R. & Neo-Acqua Study Group Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr. 101, 136–142 (2012).
Zanardo, V., Freato, F. & Zacchello, F. Maternal anxiety upon NICU discharge of high-risk infants. J. Reprod. Infant Psychol. 21, 69–75 (2003).
Purdy, I., Craig, J. & Zeanah, P. NICU discharge planning and beyond: recommendations for parent psychosocial support. J. Perinatol. 35, S24–S28 (2015).
Vahdati, M., Mohammadizadeh, M. & Talakoub, S. Effect of Kangaroo care combined with music on the mother–premature neonate attachment: a randomized controlled trial. Iran. J. Nurs. Midwifery Res. 22, 403 (2017).
Acknowledgements
The authors extend their sincere thanks to our colleagues for their valuable insights and professional support during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
S.F. conceptualized the study, designed the methodology, performed the analysis, and drafted the manuscript. D.T. reviewed and revised the manuscript and supervised the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All authors consent to the publication of this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, F., Tang, D. Effectiveness of music therapy intervention on parent-infant attachment and parental anxiety in premature infants care: a systematic review and meta-analysis. Pediatr Res (2026). https://doi.org/10.1038/s41390-025-04739-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04739-x