Abstract
Background
Proton pump inhibitors (PPIs) are commonly prescribed medications that have been shown to have contradicting effects on cancer. We aimed to investigate the effect of pantoprazole and other PPIs on prostate cancer (PCa) specific mortality (PCSM), use of androgen deprivation therapy (ADT), and PCa diagnosis using a large Canadian population-based cohort.
Methods
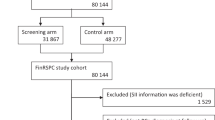
We identified 21,512 men aged ≥ 66, with a history of a single negative prostate biopsy and no previous use of any of the analyzed medications between 1994 and 2016. Multivariable Cox regression models with time-dependent covariates were used to assess the associations of PPIs with PCa outcomes. All models included other medications with a putative chemopreventative effect on PCa-outcomes, and were adjusted for age, rurality, comorbidity, and study inclusion year.
Results
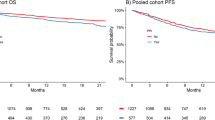
Over a mean follow-up of 8.06 years (SD 5.44 years), 10,999 patients (51.1%) used a PPI, 5187 patients (24.1%) had PCa, 2043 patients (9.5%) were treated with ADT, and 805 patients (3.7%) died from PCa. For every 6 months of cumulative use, pantoprazole was associated with a 3.0% (95% CI 0.3–6.0%) increased rate of ADT use, while any use of other PPIs was associated with a 39.0% (95% CI 18.0–64.0%) increased risk of PCSM. No association was found with PCa diagnosis.
Conclusions
Upon validation of the potentially negative association of PPIs with PCa, PPI use may need to be reassessed in PCa patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
CCSsACoCS. Canadian Cancer Statistics 2018. 2018. http://www.cancer.ca/Canadian-Cancer-Statistics-2018-EN.
CoAC S. Key Statistics for Prostate Cancer. 2019. https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html.
Sarkar RR, Parsons JK, Bryant AK, Ryan ST, Kader AK, McKay RR, et al. Association of treatment with 5alpha-reductase inhibitors with time to diagnosis and mortality in prostate cancer. JAMA Intern Med. 2019;179:812–9.
Margel D, Urbach D, Lipscombe LL, Bell CM, Kulkarni G, Austin PC, et al. Association between metformin use and risk of prostate cancer and its grade. J Natl Cancer Inst. 2013;105:1123–31.
Nielsen SF, Nordestgaard BG, Bojesen SE. Statin use and reduced cancer-related mortality. N. Engl J Med. 2012;367:1792–802.
Gesmundo I, Di Blasio L, Banfi D, Villanova T, Fanciulli A, Favaro E, et al. Proton pump inhibitors promote the growth of androgen-sensitive prostate cancer cells through ErbB2, ERK1/2, PI3K/Akt, GSK-3beta signaling and inhibition of cellular prostatic acid phosphatase. Cancer Lett. 2019;449:252–62.
Klinkenberg-Knol EC, Nelis F, Dent J, Snel P, Mitchell B, Prichard P, et al. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Gastroenterology. 2000;118:661–9.
Brusselaers N, Wahlin K, Engstrand L, Lagergren J. Maintenance therapy with proton pump inhibitors and risk of gastric cancer: a nationwide population-based cohort study in Sweden. BMJ Open. 2017;7:e017739.
Brusselaers N, Engstrand L, Lagergren J. Maintenance proton pump inhibition therapy and risk of oesophageal cancer. Cancer Epidemiol. 2018;53:172–7.
Tran KT, McMenamin UC, Proton pump inhibitor histamine-2 receptor antagon use risk liver cancer two population-based studies. 2018;48:55–64.
Halfdanarson OO, Fall K, Ogmundsdottir MH, Lund SH, Steingrimsson E, Ogmundsdottir HM, et al. Proton pump inhibitor use and risk of breast cancer, prostate cancer, and malignant melanoma: An Icelandic population-based case-control study. Pharmacoepidemiology drug Saf. 2019;28:471–8.
Canitano A, Iessi E, Spugnini EP, Federici C, Fais S. Proton pump inhibitors induce a caspase-independent antitumor effect against human multiple myeloma. Cancer Lett. 2016;376:278–83.
Cheung KS, Chan EW, Wong AYS, Chen L, Wong ICK, Leung WK. Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study. Gut. 2018;67:28–35.
Xie Y, Bowe B, Yan Y, Xian H, Li T, Al-Aly Z. Estimates of all cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: cohort study. BMJ. 2019;365:l1580.
Soriano LC, Soriano-Gabarró M, García Rodríguez LA. Trends in the contemporary incidence of colorectal cancer and patient characteristics in the United Kingdom: a population-based cohort study using The Health Improvement Network. BMC Cancer. 2018;18:402.
Kearns MD, Boursi B, Yang YX. Proton pump inhibitors on pancreatic cancer risk and survival. Cancer Epidemiol. 2017;46:80–4.
Cao Y, Chen M, Tang D, Yan H, Ding X, Zhou F, et al. The proton pump inhibitor pantoprazole disrupts protein degradation systems and sensitizes cancer cells to death under various stresses. Cell Death Dis. 2018;9:604.
Tan Q, Joshua AM, Saggar JK, Yu M, Wang M, Kanga N, et al. Effect of pantoprazole to enhance activity of docetaxel against human tumour xenografts by inhibiting autophagy. Br J cancer. 2015;112:832–40.
Hansen AR, Tannock IF, Templeton A, Chen E, Evans A, Knox J, et al. Pantoprazole affecting docetaxel resistance pathways via autophagy (PANDORA): phase II trial of high dose pantoprazole (autophagy inhibitor) with docetaxel in metastatic castration-resistant prostate cancer (mCRPC). Oncologist. 2019;24:1188–94.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885.
Institute of Clinical Evaluative Sciences Homepage. 2019. http://www.ices.on.ca.
The Johns Hopkins ACG (R) System version 10.0.
Sayyid RK, Alibhai SMH, Sutradhar R, Eberg M, Fung K, Klaassen Z, et al. Population-based outcomes of men with a single negative prostate biopsy: importance of continued follow-up among older patients. Urologic Oncol. 2019;37:298.e19–.e27.
The Top 300 of 2019. 2019. www.clincalc.com.
Malfertheiner P, Kandulski A, Venerito M. Proton-pump inhibitors: understanding the complications and risks. Nat Rev Gastroenterol Hepatol. 2017;14:697–710.
Vaezi MF, Yang YX, Howden CW. Complications of proton pump inhibitor therapy. Gastroenterology 2017;153:35–48.
Hayashi H, Taniai E, Morita R, Hayashi M, Nakamura D, Wakita A, et al. Enhanced liver tumor promotion but not liver initiation activity in rats subjected to combined administration of omeprazole and beta-naphthoflavone. J toxicological Sci. 2012;37:969–85.
Huang L, Qi DJ, He W, Xu AM. Omeprazole promotes carcinogenesis of fore-stomach in mice with co-stimulation of nitrosamine. Oncotarget. 2017;8:70332–44.
Peng YC, Lin CL, Hsu WY, Lu IT, Yeh HZ, Chang CS, et al. Proton Pump inhibitor use is associated with risk of pancreatic cancer: a nested case-control study. Dose Response. 2018;16:1559325818803283.
Hwang IC, Chang J, Park SM. Emerging hazard effects of proton pump inhibitor on the risk of colorectal cancer in low-risk populations: a Korean nationwide prospective cohort study. PloS ONE. 2017;12:e0189114.
Giridhar KV, Sanhueza C, Hillman DW, Alkhateeb H, Carlson R, Tan W, et al. Serum chromogranin-A-based prognosis in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2018;21:431–7.
Quinn DI, Sandler HM, Horvath LG, Goldkorn A, Eastham JA. The evolution of chemotherapy for the treatment of prostate cancer. Ann Oncol: Off J Eur Soc Med Oncol. 2017;28:2658–69.
Spanogiannopoulos P, Bess EN, Carmody RN, Turnbaugh PJ. The microbial pharmacists within us: a metagenomic view of xenobiotic metabolism. Nat Rev Microbiol. 2016;14:273–87.
Sfanos KS, Markowski MC, Peiffer LB, Ernst SE, White JR, Pienta KJ, et al. Compositional differences in gastrointestinal microbiota in prostate cancer patients treated with androgen axis-targeted therapies. Prostate Cancer Prostatic Dis. 2018;21:539–48.
Porter CM, Shrestha E, Peiffer LB, Sfanos KS. The microbiome in prostate inflammation and prostate cancer. Prostate Cancer Prostatic Dis. 2018;21:345–54.
Shrestha E, White JR, Yu SH, Kulac I, Ertunc O, De Marzo AM, et al. Profiling the urinary microbiome in men with positive versus negative biopsies for prostate cancer. J Urol. 2018;199:161–71.
Imhann F, Vich Vila A, Bonder MJ, Lopez Manosalva AG, Koonen DPY, Fu J, et al. The influence of proton pump inhibitors and other commonly used medication on the gut microbiota. Gut Microbes. 2017;8:351–8.
Yood MU, Campbell UB, Rothman KJ, Jick SS, Lang J, Wells KE, et al. Using prescription claims data for drugs available over-the-counter (OTC). Pharmacoepidemiol Drug Saf. 2007;16:961–8.
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding source. No endorsement by ICES of the Ontario MOHLTC is intended or should be inferred. The datasets used in this study were linked using unique encoded identifiers and analyzed at ICES. Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred. We thank IMS Brogan Inc. for use of their Drug Information Database.
Author information
Authors and Affiliations
Contributions
Design and conception: HG, NF, SA, GSK, RS. Data collection and analyses: HG, FKM, OS, RS, AB, SH, CJDW, LP, GSK, NF. Writing of manuscript: HG, FKM. Editing and reviewing of manuscript: FKM, AB, SA, RS, CJDW, ZK, TC, AEA, RKS, OS, LP, GB, GSK, NF.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goldberg, H., Mohsin, F.K., Saskin, R. et al. The deleterious association between proton pump inhibitors and prostate cancer-specific mortality – a population-based cohort study. Prostate Cancer Prostatic Dis 23, 622–629 (2020). https://doi.org/10.1038/s41391-020-0248-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41391-020-0248-9
This article is cited by
-
Association between the use of proton pump inhibitors and serum PSA levels in the general U.S. population
World Journal of Urology (2025)
-
Association between concomitant proton pump inhibitor use and survival of patients with metastatic prostate cancer receiving abiraterone acetate: a post-hoc analysis of pooled data from three randomized controlled trials
Prostate Cancer and Prostatic Diseases (2024)