Abstract
Background
Evidence on clinical presentation of benign prostatic hyperplasia (BPH) is scarce, and studies involving outpatients are lacking. We aimed to provide an insight into the contemporary Italian scenario of BPH-affected outpatients using symptom scores (International Prostate Symptom Score [IPSS], BPH Impact Index [BII]), and to compare characteristics of patients with known BPH and those first-diagnosed at the visit.
Methods
“IMPROVING THE PATH” project working group designed a questionary prospectively administered to BPH-affected outpatients by urologists. A cross-sectional study was performed. Data were adjusted for patient age as a potential confounding factor.
Results
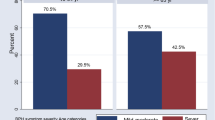
Of 5815 patients enrolled, BPH was already diagnosed in 4144 (71.3%), and not in 1671 (28.7%). Patients with known BPH, compared to newly diagnosed, were older (median 68 versus [vs] 55), had more frequent smoking (smoker 27.2 vs 22.6%, and ex-smoker 16.4 vs 12.5%) and drinking habits (55.4 vs 45.1%), were more frequently affected by hypertension (60.0 vs 42.4%), obesity (15.3 vs 9.6%), diabetes (17.9 vs 12.5%), and cardiovascular diseases (14.2 vs 9.5%), p < 0.001. At IPSS, moderate and severe symptoms correlated with already known BPH (56.1 vs 47.3% and 24.8 vs 7.8%), whereas newly diagnosed patients showed milder symptoms (44.9 vs 19.1%), all p < 0.001. At BII, concern for one’s health and time lost due to urinary problems were higher in patients with known BPH (p < 0.001). For these patients, the urologist changes at least one of the ongoing medications in 63.5%. For patients newly diagnosed, supplements/phytotherapeutics, alpha-blockers, and 5-alfa reductase inhibitors were prescribed in 54.6%, 21.6%, and 7.1%, respectively.
Conclusions
Despite medical treatment, natural history of BPH leads to a progressive deterioration of symptoms. This may reflect the difference between newly diagnosed patients and those with known BPH in lifestyle and associated comorbidities. A healthy lifestyle and treatments including local anti-inflammatory agents may delay worsening of symptoms and improve quality of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Devlin CM, Simms MS, Maitland NJ. Benign prostatic hyperplasia - what do we know? BJU Int. 2021;127:389–99. https://doi.org/10.1111/bju.15229
Vuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol. 2015;22 Suppl 1:1–6.
Rhodes T, Girman CJ, Jacobsen SJ, Roberts RO, Guess HA, Lieber MM. Longitudinal prostate growth rates during 5 years in randomly selected community men 40 to 79 years old. J Urol. 1999;161:1174–9.
Madersbacher S, Haidinger G, Temml C, Schmidbauer CP. Prevalence of lower urinary tract symptoms in Austria as assessed by an open survey of 2,096 men. Eur Urol. 1998;34:136–41. https://doi.org/10.1159/000019699
Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin N Am. 2016;43:289–97. https://doi.org/10.1016/j.ucl.2016.04.001
Madersbacher S, Sampson N, Culig Z. Pathophysiology of benign prostatic hyperplasia and benign prostatic enlargement: a mini-review. Gerontology. 2019;65:458–64. https://doi.org/10.1159/000496289
Choi WS, Son H. The change of IPSS 7 (nocturia) score has the maximum influence on the change of Qol score in patients with lower urinary tract symptoms. World J Urol. 2019;37:719–25. https://doi.org/10.1007/s00345-018-2410-8
Albisinni S, Aoun F, Roumeguère T, Porpiglia F, Tubaro A, DE Nunzio C. New treatment strategies for benign prostatic hyperplasia in the frail elderly population: a systematic review. Minerva Urol Nefrol. 2017;69:119–32. https://doi.org/10.23736/S0393-2249.16.02743-0
Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–57. https://doi.org/10.1016/s0022-5347(17)36966-5.
Abrams P, Chapple C, Khoury S, Roehrborn C, de la Rosette J. International Scientific Committee. Evaluation and treatment of lower urinary tract symptoms in older men. J Urol. 2009;181:1779–87. https://doi.org/10.1016/j.juro.2008.11.127
Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK. Measuring disease-specific health status in men with benign prostatic hyperplasia. Measurement Committee of The American Urological Association. Med Care. 1995;33:AS145–55.
Mobley D, Feibus A, Baum N. Benign prostatic hyperplasia and urinary symptoms: evaluation and treatment. Postgrad Med. 2015;127:301–7. https://doi.org/10.1080/00325481.2015.1018799
O’Leary MP, Wei JT, Roehrborn CG, Miner M, BPH Registry and Patient Survey Steering Committee. Correlation of the International Prostate Symptom Score bother question with the Benign Prostatic Hyperplasia Impact Index in a clinical practice setting. BJU Int. 2008;101:1531–5. https://doi.org/10.1111/j.1464-410X.2008.07574.x
Kingery L, Martin ML, Naegeli AN, Khan S, Viktrup L. Content validity of the Benign Prostatic Hyperplasia Impact Index (BII); a measure of how urinary trouble and problems associated with BPH may impact the patient. Int J Clin Pract. 2012;66:883–90. https://doi.org/10.1111/j.1742-1241.2012.02960.x
Fusco F, Palmieri A, Ficarra V, Giannarini G, Novara G, Longo N, et al. α1-Blockers improve benign prostatic obstruction in men with lower urinary tract symptoms: a systematic review and meta-analysis of urodynamic studies. Eur Urol. 2016;69:1091–101. https://doi.org/10.1016/j.eururo.2015.12.034
Sebastianelli A, Spatafora P, Morselli S, Vignozzi L, Serni S, McVary KT, et al. Tadalafil alone or in combination with tamsulosin for the management for LUTS/BPH and ED. Curr Urol Rep. 2020;21:56 https://doi.org/10.1007/s11934-020-01009-7
Hong SK, Min GE, Ha SB, Doo SH, Kang MY, Park HJ, et al. Effect of the dual 5alpha-reductase inhibitor, dutasteride, on serum testosterone and body mass index in men with benign prostatic hyperplasia. BJU Int. 2010;105:970–4. https://doi.org/10.1111/j.1464-410X.2009.08915.x
Joo K-J, Sung W-S, Park S-H, Yang W-J, Kim T-H. Comparison of α-blocker monotherapy and α-blocker plus 5α-reductase inhibitor combination therapy based on prostate volume for treatment of benign prostatic hyperplasia. J Int Med Res. 2012;40:899–908. https://doi.org/10.1177/147323001204000308
Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57:123–31. https://doi.org/10.1016/j.eururo.2009.09.035
Roehrborn CG, Perez IO, Roos EPM, Calomfirescu N, Brotherton B, Wang F, et al. Efficacy and safety of a fixed-dose combination of dutasteride and tamsulosin treatment (Duodart(®)) compared with watchful waiting with initiation of tamsulosin therapy if symptoms do not improve, both provided with lifestyle advice, in the management of treatment-naïve men with moderately symptomatic benign prostatic hyperplasia: 2-year CONDUCT study results. BJU Int. 2015;116:450–9. https://doi.org/10.1111/bju.13033
Choi JD, Kim JH, Ahn SH. Transitional zone index as a predictor of the efficacy of α-blocker and 5α-reductase inhibitor combination therapy in Korean patients with benign prostatic hyperplasia. Urol Int. 2016;96:406–12. https://doi.org/10.1159/000442995
Mari A, Antonelli A, Cindolo L, Fusco F, Minervini A, De Nunzio C. Alfuzosin for the medical treatment of benign prostatic hyperplasia and lower urinary tract symptoms: a systematic review of the literature and narrative synthesis. Ther Adv Urol. 2021;13. https://doi.org/10.1177/1756287221993283
Jiang Y-L, Qian L-J. Transurethral resection of the prostate versus prostatic artery embolization in the treatment of benign prostatic hyperplasia: a meta-analysis. BMC Urol. 2019;19:11 https://doi.org/10.1186/s12894-019-0440-1
Liu Y, Cheng Y, Zhuo L, Liu K, Xiao C, Zhao R, et al. Impact on sexual function of endoscopic enucleation vs transurethral resection of the prostate for lower urinary tract symptoms due to benign prostatic hyperplasia: a systematic review and meta-analysis. J Endourol. 2020;34:1064–74. https://doi.org/10.1089/end.2020.0141
Tanneru K, Jazayeri SB, Alam MU, Kumar J, Bazargani S, Kuntz G, et al. An indirect comparison of newer minimally invasive treatments for benign prostatic hyperplasia: a network meta-analysis model. J Endourol. 2021;35:409–16. https://doi.org/10.1089/end.2020.0739
Abt D, Hechelhammer L, Müllhaupt G, Markart S, Güsewell S, Kessler TM, et al. Comparison of prostatic artery embolisation (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: randomised, open label, non-inferiority trial. BMJ. 2018;361:k2338 https://doi.org/10.1136/bmj.k2338
Spatafora S, Canepa G, Migliari R, Rotondo S, Mandressi A, Puppo P. Diagnostic procedures by Italian general practitioners in response to lower urinary tract symptoms in male patients: a prospective study. Curr Med Res Opin. 2004;20:713–21. https://doi.org/10.1185/030079904125003557
McNicholas TA. Lower urinary tract symptoms suggestive of benign prostatic obstruction: what are the current practice patterns? Eur Urol. 2001;39 Suppl 3:26–30. https://doi.org/10.1159/000052564
Spatafora S, Canepa G, Migliari R, Rotondo S, Mandressi A, Puppo P, et al. Effects of a shared protocol between urologists and general practitioners on referral patterns and initial diagnostic management of men with lower urinary tract symptoms in Italy: the Prostate Destination study. BJU Int. 2005;95:563–70. https://doi.org/10.1111/j.1464-410X.2005.05340.x
Li J, Peng L, Cao D, Gou H, Li Y, Wei O. The association between metabolic syndrome and benign prostatic hyperplasia: a systematic review and meta-analysis. Aging Male. 2020;23:1388–99. https://doi.org/10.1080/13685538.2020.1771552
Xia B-W, Zhao S, Chen Z, Chen C, Liu T, Yang F, et al. The underlying mechanism of metabolic syndrome on benign prostatic hyperplasia and prostate volume. Prostate. 2020;80:481–90. https://doi.org/10.1002/pros.23962
Gandaglia G, Briganti A, Gontero P, Mondaini N, Novara G, Salonia A, et al. The role of chronic prostatic inflammation in the pathogenesis and progression of benign prostatic hyperplasia (BPH). BJU Int. 2013;112:432–41. https://doi.org/10.1111/bju.12118
Abdollah F, Briganti A, Suardi N, Castiglione F, Gallina A, Capitanio U, et al. Metabolic syndrome and benign prostatic hyperplasia: evidence of a potential relationship, hypothesized etiology, and prevention. Korean J Urol. 2011;52:507–16. https://doi.org/10.4111/kju.2011.52.8.507
Wang X, Su Y, Yang C, Hu Y, Dong J-Y. Benign prostatic hyperplasia and cardiovascular risk: a prospective study among Chinese men. World J Urol. 2021. https://doi.org/10.1007/s00345-021-03817-z.
Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016;13:108–19. https://doi.org/10.1038/nrurol.2015.301
Ngai H-Y, Yuen K-KS, Ng C-M, Cheng C-H, Chu S-KP. Metabolic syndrome and benign prostatic hyperplasia: an update. Asian J Urol. 2017;4:164–73. https://doi.org/10.1016/j.ajur.2017.05.001
De Nunzio C, Presicce F, Tubaro A. Inflammatory mediators in the development and progression of benign prostatic hyperplasia. Nat Rev Urol. 2016;13:613–26. https://doi.org/10.1038/nrurol.2016.168
Sarma AV, Burke JP, Jacobson DJ, McGree ME, St Sauver J, Girman CJ, et al. Associations between diabetes and clinical markers of benign prostatic hyperplasia among community-dwelling Black and White men. Diabetes Care. 2008;31:476–82. https://doi.org/10.2337/dc07-1148
Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 2015;67:1066–96. https://doi.org/10.1016/j.eururo.2014.06.017
Cindolo L, Pirozzi L, Sountoulides P, Fanizza C, Romero M, Castellan P, et al. Patient’s adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)-associated lower urinary tract symptoms (LUTS) is different: is combination therapy better than monotherapy? BMC Urol. 2015;15:96. https://doi.org/10.1186/s12894-015-0090-x
Acknowledgements
We sincerely acknowledge all the urologists who participated in the project: AMBRUOSI Carlo, ANDRETTA Elena, AUTIERI Domenico, AZZARITO Giuseppina, BASSI Silvia, BERTOLONI Rossella, CALI’ Claudia Carmela Maria, CASSONE Giuseppe, CASTRO Riccardo, CATANZARITI Francesco, CECCHETTI Giampiero, CEGLIA Antonio, COCO Angela, CROCE Francesco, DE VECCHIS Massimiliano, DELL’AGLIO Francesco, DI GIROLAMO Angela Grazia, DI PALMA Paolo, DI TRAPANI Danilo, FERRI Claudio, FINOCCHIARO Marinella, FLORIO Mirko, FUCCI Carminantonio, GAETA Francesco, GALASSO Raffaele, GAMBARDELLA Raffaele, GAROFALO Francesco, GASTALDI Christian, GITANA Carlo, GRASSO Vincenzo Maria Giuseppe, HEFFAWI Naif, IACONA Gabriele, IACONE Mario, IACOVETTA Domenico, INGRASSIA Antonino, LEMBO Francesco, LEO Salvatore, LUCERA Rossana, MAIMONE Maria Rosa, MANASSERO Francesca, MANGRAVITI Giuseppe, MASIELLO Giuseppe, MATTIELLO Gennaro, MINI’ Salvatore, MOTTA Luigi, PAPERINI Davide, PEZZOTTI Domenico, PICOZZI Stefano, PIROLA Giacomo Maria, PORROZZI Carlo, PORTOGHESE Filippo, QUARESIMA Luigi, QUATTRONE Carmelo, REALE Giulio Francesco, ROMAGNOLI Daniele, ROMANO Giuseppe, SALAME’ Leonardo Mosé, SALDUTTO Pietro, SAVINO Mario Paolo Nicola, SIMONE Maurizio, SOZZI Francesco, SPERONI Alberto, STENER Silvio, TALLIS Valeria, VANNINI Luciano, VENEZIA Valeria Carolina, VITELLI Ferdinando Daniele, ZAPPIA Domenico Giuseppe.
Funding
The study was unconditionally supported by Neopharmed Gentili.
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission have contributed sufficiently to the scientific work and share collective responsibility and accountability for the results. All authors read and approved the final version of the manuscript. PIO: Project development, data collection, data analysis, Manuscript writing/editing. AP: Project development, manuscript editing. MS: Project development, data analysis, manuscript editing. AS: Project development, manuscript editing. MF: Project development, manuscript editing. GML: Project development, manuscript editing. MAC: Project development, manuscript editing. AA: Project development, manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent for the collection of anonymized data for scientific purposes was obtained from all patients included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ornaghi, P.I., Porreca, A., Sandri, M. et al. Features of patients referring to the outpatient office due to benign prostatic hyperplasia: analysis of a national prospective cohort of 5815 cases. Prostate Cancer Prostatic Dis 26, 730–735 (2023). https://doi.org/10.1038/s41391-022-00575-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41391-022-00575-w
This article is cited by
-
Endoscopic en bloc prostate enucleation: a propensity score matched analysis between greenlight enucleation of prostate (GreenLEP) vs holmium laser enucleation of prostate (HOLEP) outcomes and safety with a 12-month follow-up
International Urology and Nephrology (2025)
-
When you say “Prostate”, don’t forget to say “Bladder”!
Prostate Cancer and Prostatic Diseases (2024)
-
Prevalence of lower urinary tract symptoms in taxi drivers: a cross-sectional web-based survey
Prostate Cancer and Prostatic Diseases (2024)
-
Ejaculation physiology and dysfunction after BPH surgery: the role of the new MISTs
Prostate Cancer and Prostatic Diseases (2023)
-
To all men with urinary symptoms – seek help early!
Prostate Cancer and Prostatic Diseases (2023)